Abstract
Although tumefactive multiple sclerosis is a well recognized variant of multiple sclerosis, prognostic uncertainty still exists about long term prognosis. The aim of this study was to estimate the occurrence and long term outcome of tumefactive demyelinating lesions (TDLs) in a cohort of multiple sclerosis patients. We reviewed brain MRI of 443 patients referred to our MS clinic. All patients meeting the McDonald criteria for multiple sclerosis and showing at least one TDL were included. Kaplan–Meier estimates of disease-free survival in patient cohort were compared with control group without TDLs using a log-rank test. Seven cases with TDLs were identified (occurrence 1.58 %). Tumefactive demyelinating lesion recurrence was 16.6 %. Cumulative proportion of patients free from clinical relapse and from new T2 lesions was lower in the control group although not reaching statistical significance (30 vs 50 %; P = 0.666 and 21.7 vs 33.3 %; P = 0.761, respectively). Disability progression analysis showed a not significant trend towards lower probability of remaining progression free for TDL patients (50 vs 61 %; P = 0.295). Occurrence of tumefactive demyelinating lesions in our cohort was higher than those reported in other studies. Overall, TDLs were not predictive of poor outcome in terms of disability progression.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The revision of the McDonald diagnostic criteria in 2010 backs up the rapidly growing role of magnetic resonance imaging (MRI) in multiple sclerosis (MS) diagnosis. Characterization of demyelinating lesions by MRI is the mainstay for differential diagnosis with other central nervous system disease [1–3]. Typical MS plaque features encompass small size, ovoid shape, well-defined margins and major axis perpendicular to the ventricular surface [4]. Nevertheless, the occurrence of large pseudotumoral demyelinating lesions with atypical radiological features is well described in multiple sclerosis. These atypical plaques are often referred to as tumefactive demyelinating lesions (TDLs) [5]. Proper identification and description of cases over time has been hampered by the lack of a unifying terminology. Actually the “umbrella heading” of tumefactive demyelinating lesions encompasses a variety of entities previously referred to as Balo’s concentric sclerosis, diffuse myelinoclastic sclerosis and pseudotumoral multiple sclerosis. Of further note, literature lacks uniform definition of TDL as well. Typical MRI features of TDL reported by the vast majority of published cases include 2 cm or more in diameter with or without associated mass effect, perilesional edema and variable contrast enhancement patterns (closed ring, open to ring, arc like, punctate or nodular appearance) [6–15]. The absence of contrast enhancement, albeit rare, has been reported in 5 % of biopsy confirmed cases and therefore should not exclude a demyelinating pathology [16]. The occurrence of tumefactive multiple sclerosis has been estimated of about 1–2/1000 cases of multiple sclerosis [17]. TDL can arise during the course of a known multiple sclerosis or can be the first manifestation of MS. Monophasic isolated TDLs may also occur [16].
Due to dearth of longitudinal studies with long-term clinical and radiological evaluation, the natural history of tumefactive demyelinating lesions is still ill defined. Prior reports from literature suggested a more favorable course compared to classic multiple sclerosis. To date, the largest case series comes up from a study from Lucchinetti et al. reporting 168 biopsy confirmed cases of TDLs [16]. Disability progression was significantly lower compared to that of a paired population-based prevalence cohort among patients with long disease duration (>10 years), suggesting that disease course is not negatively affected by the occurrence of tumefactive lesions [16]. Thus far, few studies have addressed long-term follow-up data in patients diagnosed with tumefactive demyelinating lesions leading to prognostic uncertainty in these patients [18, 19].
The aim of this prospective cohort study was to estimate the occurrence of TDL in patients diagnosed with relapsing-remitting MS (RRMS) and to assess the clinical feature and long-term outcome.
Materials and methods
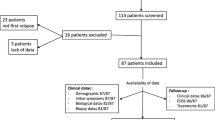
Brain MRI of 443 patients diagnosed with multiple sclerosis who had been referred to our multiple sclerosis clinic between May 2005 and December 2013 were reviewed. Patients were diagnosed with multiple sclerosis in accordance with McDonald diagnostic criteria. Inclusion criteria were the occurrence of at least one TDL on brain imaging as defined by lesion size larger than 2 cm. Patients with past medical history of neoplasm, CNS infection or vascular disease were excluded.
All data were retrospectively gathered by electronic medical records review and demographic and clinical data were obtained, including: gender, birth date, age at disease onset and at the occurrence of TDL, index attack symptoms and EDSS, concomitant medications. As a part of clinical medical routine, in all patients we performed neurological examination and EDSS assessment at least twice a year and MRI at least once a year. Unscheduled visits were performed whenever relapses, adverse events or treatment discontinuation occurred. Patients missing routine visits were recalled to visits before being considered lost to follow-up. Therefore, none of the patients included in this study dropped out.
Standardized contrast enhanced MRI was performed on a GE (General Electric Medical Systems, Milwaukee, WI) Signa 1.5 T MR scanner using birdcage head coils. Slice thickness was 3 mm with no interslice gap. Precontrast axial T2 (TR 3000 TE 102) and axial T1 (TR 450 TE 20) weighted images, axial FLAIR, sagittal T2 W, post-contrast administration axial T1 W and a 3D FSPGR volumetric sequence T1 weighted were performed in each patient. Meanwhile a Gd-chelate at standard dose of 0.1 mMol/kg bw followed by 15 ml of a saline solution was administered through an 18 gauge needle placed into the ante-cubital vein using an automatic injector. MRI were analysed by experienced neurologists and neuroradiologists.
Tumefactive demyelinating lesions were identified by lesion size >2 cm and analysed for radiographic features as defined by Lucchinetti et al. [16]. We assessed lesion size (T2 margin to margin or discernible lesion size when it was possible to tell discrete lesions from surrounding oedema), location, mass effect (mild: sulcal effacement; moderate: minimal subfalcine or uncal hernation, <1 cm; marked: >1 cm subfalcine or uncal hernation), oedema (mild: <1 cm from the lesion; moderate: 1–3 cm from the lesion; marked: >3 cm from the lesion), T2 hypointense rim, and enhancement pattern (homogeneous, ring-like, heterogeneous with patchy, fluffy/cotton ball, nodular or punctate appearance). Brain scans were also reviewed for the presence of other typical MS T2 hyperintense and T1 hypointense lesions.
Ten controls for each patient with TDL were selected from a cohort of MS patients referred to our multiple sclerosis clinic. Controls were matched for sex and age at the time of study entry, namely the date of first MRI performed at our center.
Continuous variables were reported as means, standard deviations and range while discrete data were reported in contingency tables as absolute and relative frequencies.
Kaplan–Meier estimates of disease-free survival as defined by absence of clinical relapse, disability progression and radiological disease activity in TDL cohort were compared with the MS control group by means of the log-rank test.
Multivariate survival analysis was carried out by Cox Regression model including age at the TDL onset, treatment, EDSS at baseline, relapse at TDL onset as covariates. A significance level of 0.05 was used for each test. For all the analysis, IBM SPSS Statistics for Windows, Version 20.0, was used.
Results
Seven out of 443 MS patients (1.58 %) met the inclusion criteria for TDL. Five patients were female. Mean age at onset of first TDL was 24 ± 7.07 years. One patient was excluded from survival analysis because lost to follow-up. During the follow-up (mean 7.93 ± 7.95 years) one patient suffered one TDL recurrence 23 months after the first event. TDL recurrence was 16.6 %.
Radiological features of the TDL are summarized in Table 1.
Three patients experienced neurological deterioration concomitant to TDL occurrence. Sensory loss (n = 2), sensory-motor impairment (n = 2) and aphasia associated with psychomotor agitation (n = 1) were the presenting symptoms in the symptomatic cases, relapse severity being moderate to severe (mean EDSS 3.16 at the time of index attack). One patient has been under fingolimod treatment for 13 months before TDL occurrence [20]. All the other patients were not taking any immunomodulatory drug at TDL onset. Clinical characteristics of TDL cohort are summarized in Table 2.
The cumulative proportion of patients free from new relapse was lower in the control group with respect to TDL cohort, although not achieving statistical significance (30.0 vs 50.0 %; log rank test; P = 0.666).
The cumulative proportion of patients free from EDSS progression was lower, although not significantly, in the group of patients with TDL with respect to control group (50.0 vs 61.0 %; log rank test; P = 0.295).
The cumulative proportion of patients free from new lesions at MRI was lower in the control group with respect to TDL cohort but this result did not reach statistical significance (21.7.0 vs 33.3 %; log rank test; P = 0.761).
Discussion
TDLs are pathologically confirmed demyelinating plaques with atypical radiological features often posing diagnostic issues especially when presenting as solitary lesions mimicking brain neoplasms. TDLs may lead to several diagnostic, therapeutic and prognostic issues for they can be misdiagnosed as primary malignancy or metastatic disease causing unwarranted interventions and treatments. A confident diagnosis can be made through ancillary brain imaging techniques such as diffusion weighted imaging (DWI), magnetic resonance spectroscopy (MRS) and fluoro-deoxyglucose positron emission tomography (FDG-PET), but often diagnostic certainty eventually requires brain biopsy.
Few studies addressed the occurrence of TDL in the context of multiple sclerosis natural disease course [18, 19]. In our cohort of patients carrying a diagnosis of MS, TDL occurrence was 1.58 %, much higher than previous finding from literature reporting TDLs to occur in 1–2/1.000 cases of MS [17]. Many case series suggested TDLs to be far more frequent in Asiatic patients diagnosed with MS, with occurrence ranging from 6.3 to 11.76 % [18, 19]. Racial and ethnic differences reflecting the heterogeneous immunological background may partly account for the apparent higher prevalence of tumefactive plaques in Asiatic population [21]. Paty et al. suggested an estimated prevalence of 3/1.000.000 inhabitants per year while conflicting evidence from neuropathological studies led to inconclusive results [22–24].
TDLs recurred in 16.6 % of patients in our cohort, this finding being in line with previous reports from literature (recurrence rate 16.7 to 25 %) [18, 25].
Despite the pathological basis of TDLs still being poor understood, some studies suggested a developmentally immature isoform of myelin basic protein (MBP) to play a role in atypical forms of MS characterized by extensive demyelination such as Marburg type and possibly TDLs [26, 27]. Different isoforms of MBP may interfere with normal functioning also being more susceptible to protein degradation and antigen presentation and thus making TDL patients more likely to experience TDL recurrence compared to general MS population.
Disability progression analysis showed a trend towards lower probability of remaining progression free for TDL patients compared to control cohort at almost 8-year follow-up, although this result did not achieve statistical significance. Noteworthy, evidence from previous studies has highlighted a possible benign course of tumefactive demyelination compared to other forms of MS [28, 29]. Lucchinetti et al. found lower levels of disability for the TDL cohort with respect to a control group matched for disease duration longer than 10 years, whereas TDL cohort was associated with higher EDSS scores compared to control group matched for disease duration less than 10 years [16]. This finding backs the hypothesis that TDL is not associated with poorer outcome per se and longer follow-up time may disclose a trend towards an even better prognosis compared to general MS population. Additionally, survival analysis also revealed a trend towards a higher probability of remaining MRI disease activity free for the TDL cohort, thus suggesting a less aggressive course for tumefactive MS.
Nevertheless, some shortcomings of our study must be highlighted. We included only patients with a definite diagnosis of MS, possibly leading to selection bias since TDLs at onset, not meeting MS diagnostic criteria at the time of enrolment, might be missed. In addition, the high proportion of patients being asymptomatic at disease onset may point towards a more benign disease course in our TDL cohort.
Since the occurrence of TDLs in MS population is low, larger sample sizes or population study are warranted in order that conclusive results can be drawn.
References
Polman CH, Reingold SC, Banwell B et al (2011) Diagnostic criteria for multiple sclerosis: 2010 revisions to the McDonald criteria. Annal Neurol 69:292–302
Charil A, Yousry TA, Rovaris M et al (2006) MRI and the diagnosis of multiple sclerosis: expanding the concept of “no better explanation”. Lancet Neurol 5:841–852
Marsecano C, Perri M, Michelini G et al (2015) Vascular malformation mimicking multiple sclerosis active plaque: usefulness of susceptibility weighted imaging (SWI) to perform correct diagnosis. Neuroradiol J 28:488–492
Ciccarelli O, Miller DH (2002) Magnetic resonance imaging in multiple sclerosis. Pract Neurol 2:103–112
Hardy TA, Chataway J (2013) Tumefactive demyelination: an approach to diagnosis and management. JNNP 0:1–7
De Medeiros FC, De Albuquerque LAF, Pittella JEH et al (2014) Open-ring enhancement in pseudotumoral multiple sclerosis: important radiological aspect. Case Rep Neurol Med 2014:951690
Ernst T, Chang L, Walot I et al (1998) Physiologic MRI of a tumefactive multiple sclerosis lesion. Neurology 51:1486–1488
Selkirk SM, Shi J (2005) Relapsing-remitting tumefactive multiple sclerosis. Mult Scler 11:731–734
Law M, Meltzer D, Cha S (2002) Spectroscopic magnetic resonance imaging of a tumefactive demyelinating lesion. Neuroradiology 44:986–989
Tsui EYK, Leung WH, Chan JH et al (2002) Tumefactive demyelinating lesions by combined perfusion-weighted and diffusion weighted imaging. Comput Med Imaging Graph 26:343–346
Findling O, Sellner J, Ozdoba C et al (2007) Tumefactive lesion in multiple sclerosis. Acta Neurol Belg 107:134
Kaeser MA, Scali F, Lanzisera FP et al (2011) Tumefactive multiple sclerosis: an uncommon diagnostic challenge. J Chiropr Med 10:29–35
Khoshyomn S, Braff S, Penar P (2002) Tumefactive multiple sclerosis plaque. JNNP 73:85
Malhotra HS, Jain KK, Agarwal A et al (2009) Characterization of tumefactive demyelinating lesions using MR imaging and in vivo proton MR spectroscopy. Mult Scler 15:193–203
Saini J, Chatterjee S, Thomas B et al (2011) Conventional and advanced magnetic resonance imaging in tumefactive demyelination. Acta Radiol 52:1159–1168
Lucchinetti CF, Gavrilova RH, Metz I et al (2008) Clinical and radiographic spectrum of pathologically confirmed tumefactive multiple sclerosis. Brain 131:1759–1775
Poser CM, Paty DW, Scheinberg L et al (1983) New diagnostic criteria for multiple sclerosis: guidelines for research protocols. Ann Neurol 13:227–231
Kuan YC, Wang KC, Yuan WH et al (2013) Tumefactive multiple sclerosis in Taiwan. PLoS One 8:e69919
Kiriyama T, Kataoka H, Taoka T et al (2011) Characteristic neuroimaging in patients with tumefactive demyelinating lesions exceeding 30 mm. J Neuroimaging 21(2):e69–e77
Totaro R, Di Carmine C, Carolei A (2014) Tumefactive demyelinating lesions in patients with relapsing remitting multiple sclerosis treated with Fingolimod. J Neurol Neurophysiol S12:006. doi:10.4172/2155-9562.S12-006
Kira J, Kanai T, Nishimura Y et al (1996) Western versus Asian types of multiple sclerosis: immunogenetically and clinically distinct disorders. Ann Neurol 40:569–574
Paty DW, Oger JJ, Kastrukoff LF et al (1988) MRI in the diagnosis of MS: a prospective study with comparison of clinical evaluation, evoked potentials, oligoclonal banding, and CT. Neurology 38:180–185
Hunter S, Ballinger W, Rubin J (1987) Multiple sclerosis mimicking primary brain tumor. Arch Pathol Lab Med 111:464–468
Annesley-Williams D, Farrell MA, Staunton H et al (2000) Acute demyelination, neuropathological diagnosis, and clinical evolution. J Neuropathol Exp Neurol 59:477–489
Altintas A, Petek B, Isik N et al (2012) Clinical and radiological characteristics of tumefactive demyelinating lesions: follow-up study. Mult Scler 18:1448–1453
Beniac DR, Wood DD, Palaniyar N et al (1999) Marburg’s variant of multiple sclerosis correlates with a less compact structure of myelin basic protein. Mol Cell Biol Res Commun 1:48–51
Wood DD, Bilbao JM, O’Connors P et al (1996) Acute multiple sclerosis (Marburg type) is associated with developmentally immature myelin basic protein. Ann Neurol 40:18–24
Kepes J (1993) Large focal tumor-like demyelinating lesions of the brain: intermediate entity between multiple sclerosis and acute disseminated encephalomyelitis: a study of 31 patients. Ann Neurol 33:18–27
Hayashi T, Kumabe T, Jokura H et al (2003) Inflammatory demyelinating disease mimicking malignant glioma. J Nucl Med 44:565–569
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Totaro, R., Di Carmine, C., Splendiani, A. et al. Occurrence and long-term outcome of tumefactive demyelinating lesions in multiple sclerosis. Neurol Sci 37, 1113–1117 (2016). https://doi.org/10.1007/s10072-016-2558-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-016-2558-1