Abstract
The objective of the study was to determine the correlation of thyroid hormones (THs) and survival in patients with amyotrophic lateral sclerosis (ALS). A total of 278 patients with ALS were enrolled and followed up prospectively every 3 months by face-to-face interviews or phone calls. Level of fasting serum TH was determined at the time of enrollment. Clinical data including age, onset age, onset body region, ALS Functional Rating Scale- Revised (ALS-FRS-R), and survival were collected. Patients were separated into four subgroups according to the quartile distribution of TH, and survival was compared among them. There was no significant difference in baseline characteristics, including onset age, gender, onset form as well as treatment with riluzole among different levels of TH subgroups. Chi-square test indicated that the lowest quartile of FT3 (<4.26 mg/L) might correlate with higher incidences of death (OR 0.374, 95 % CI 0.173–0.813), while second and third quartiles of FT4 (range 14.25–18.0 mg/L) with lower incidences of death in ALS. However, after correction for onset age and onset form using logistic regression analysis, no statistical difference was revealed in survival among patients with different TH levels. TH does not correlate with survival and is not a prognostic factor for ALS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Amyotrophic lateral sclerosis (ALS) is a chronic, typically adult-onset neurodegenerative disease, involving both the upper and lower motor neurons in the motor areas of cerebral cortex, brainstem and spinal cord, leading to death within 3–5 years through failure of respiration mostly [1].
Despite the traditional view considering that ALS was a pure motor neuron disorder affecting motor functions simply, increasing evidence has been suggesting that ALS is a multi-system disease with additional extra-motor neurologic and extra-neurological manifestations [2–5]. Beyond the nervous system, intriguing metabolic abnormalities have been reported in ALS patients, such as elevated systematic metabolism [6, 7], dyslipidemia [8], uric acid abnormality [9], disturbed glucose tolerance [10] and insulin resistance [11].
It has been well known that thyroid hormone (TH) plays a major role in normal development, metabolism and growth of many organ systems including central nervous system [12]. Several basic researches reported that thyroid hormone was involved in the up-regulation of growth of neuronal cells including motor neurons [13–15]. There was evidence that hypermetabolism could exacerbate the rate of motor neuron degeneration by increasing the production of reactive oxygen species in mitochondria [16], whose dysfunction closely correlated with the pathogenesis of ALS [17]. Therefore, reducing metabolism systemically may in theory prolong the survival in ALS. Nevertheless, the life span of SOD1G93A ALS mice did not get prolonged using non-pharmacologic calorie restriction [18], nor by a pharmacologic approach such as methimazole which can lead to hypothyroidism by inhibiting TH synthesis [19].
Therefore, there has been increasing interest in investigating the role of TH in the progression of ALS. We determined the TH status in a large sample of patients with ALS, and analyzed the correlation of different levels of TH with the survival of ALS patients.
Methods
Patients
Patients with clinical diagnosis of definite or probable ALS (El Escorial revised criteria) from a large, regional referral ALS clinic of Southwest China, from May 2006 to March 2013 were enrolled in the study. Level of fasting serum TH including free triiodothyronine (FT3), free thyroxine (FT4) and thyroid stimulating hormone (TSH) was determined at enrollment. The demographic features and clinical data such as age, onset age, onset body region, disease duration, and survival time were collected. Forced vital capacity (FVC) and ALS Functional Rating Scale-Revised (ALS-FRS-R) assessed the severity of ALS patients. Patients were followed up every 3 months by face-to-face interviews or by phone calls. Survival was determined when patients were alive without tracheotomy. Patients with pre-ALS thyroid diseases diagnosed by endocrine specialists were excluded. The study was approved by the local ethics committee of West China Hospital, Sichuan University. All the patients were informed about the purpose of the study.
Statistical analysis
Analysis was performed using SPSS version 17.0 software. All continuous data including mean age, onset age, disease duration, and ALS-FRS-R were presented in the form of mean ± standard deviation, and compared between subgroups with Kruskal–Wallis H test. The levels of TH were separated into quartiles based on their distribution of the ALS patients, and the highest quartile of each variable was applied as a reference for analysis of investigating its possible role in ALS survival (Table 1). Odds ratios (OR) and 95 % confidence intervals (CI) were estimated by Chi-square test, and by Logistic Regression analysis. Kaplan–Meier curves using log-rank test were performed in survival analysis of ALS patients.
Results
A total of 278 patients with probable or definite diagnosed ALS were enrolled, with the baseline demographic data collected at the date of the study enrollment displayed in Table 1. Among them, there were 119 females and 159 males, i.e., male-to-female ratio was 1.34:1. The mean age at ALS onset was 53.0 ± 12.4 years (range 22.6–78.5 years), and 64 patients (23.0 %) had a bulbar form at onset. The mean TSH value was 2.59 ± 2.42 mg/dL (range 0.21–33.48 mg/dL), and FT3 4.64 ± 0.70 mg/dL (2.58–7.89 mg/dL), FT4 16.35 ± 4.45 mg/dL (ranged 9.30–76.7 mg/dL). A total of 20 (7.2 %) patients had abnormal TH levels, of whom 14 (5.1 %) ALS had lower FT3, 10 (3.6 %) lower FT4, and 6 (2.2 %) ALS patients increased FT4. None of the ALS patients had abnormal TSH and increased FT3. None of these patients needed to receive medication treatment according to endocrine specialists. Three patients with higher serum TSH level had hypertension managed with antihypertensive agents. One patient with normal TH levels had type 2 diabetes mellitus, and was diet controlled. None of these patients reported any significant hypertensive or diabetic complications. Two patients with lower FT3 levels and six patients with normal TH levels had a history of taking creatine or enzyme Q10.
FT3 was significantly higher in males than in females (4.75 ± 0.69 vs. 4.50 ± 0.68, P = 0.002), but not between limb- and bulbar-onset patients (P = 0.108), nor between early and late onset groups (P = 0.922). No statistical differences were revealed while analyzing TSH and FT4 levels in different gender, onset form as well as early or late onset groups (P > 0.05) (Table 2).The patients were separated into four subgroups according to the quartile distribution of TH. There were no significant differences in baseline characteristics including onset age, gender, onset form, treatment with riluzole as well as survival among the four subgroups (Table 1).
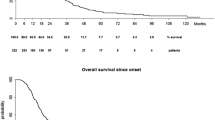
At the end of our study, 74 ALS patients had died, with 70 (94 %) of respiratory dysfunction. With the highest quartile of each variable being applied as a reference for analysis, we investigated the possible role in ALS survival by Chi-square test, which showed that lowest quartile of FT3 (<4.26 mg/L) correlated with higher incidences of death in ALS, second and third quartile of FT4 (range 14.25–18.0 mg/L) correlated with less incidences of death, while no correlation was found between different levels of TSH and survival in ALS. Kaplan–Meier curve with log-rank test indicated that the lowest quartile of FT3 was significantly associated with shorter survival time of ALS than the highest quartile of FT3 (P = 0.007; Fig. 1a). There were no differences in survival time between the first, second, third, and highest quartile of FT4 and TSH (P > 0.05; Fig. 1b, c). However, considering the relation between FT3 and FT4, and the close correlations of onset age, onset form with survival in ALS [20], we, therefore, performed the logistic regression analysis with adjusted for onset age, onset form to further analyze the effects on the survival of different levels of TH. As illustrated in Table 3, after correction for onset age and onset form, there was no correlation between different levels of TH and survival of ALS.
Correlation between TH levels and survival in ALS patients. Kaplan–Meier survival curves of 278 patients with ALS stratified according to their thyroid hormones’ levels. a FT3 level. Blue line <4.26 mg/dL, green line 4.26–4.64 mg/dL, orange line 4.65–5.05 mg/dL, purple line >5.05 mg/dL. The lowest quartile of FT3 (<4.26 mg/dL) in early onset ALS patients was associated with shorter survival time of the disease in pairwise analysis (P = 0.007). b FT4 level. Blue line <14.25 mg/dL, green line 14.25–15.89 mg/dL, orange line 15.90–18.00 mg/dL, purple line >18.00 mg/dL. c TSH level. Blue line <1.51 mg/dL, green line 1.51–2.09 mg/dL, orange line 2.10–3.14 mg/dL, purple line >3.14 mg/dL. FT3 free triiodothyronine, FT4 free thyroxine, TSH thyroid stimulating hormone, ALS amyotrophic lateral sclerosis (color figure online)
Discussion
To the best of our knowledge, this is the first study to analyze the correlation of TH and survival in a relatively large cohort of ALS patients. The demographic data of included patients were in accordance with previous reports, showing that the patients included in the present study are good representatives of the ALS population.
In the current study, ALS patients who had abnormal level of TH were not common (7.2 %). Although the association of FT3 level with survival of ALS in monovariate analysis was found in the current study, the significance of which was not maintained in multivariate analysis after adjusting for gender, onset age and onset form. Moreover, it has been indicated that thyroid hormone could be influenced by age, gender and even tested season in previous studies [21, 22]. In a word, the data we presented here indicated that TH does not have impact on survival of patients with ALS. Our findings were in accordance with these human studies and animal studies. Many researchers found that TH status was not relevant to the pathogenesis of ALS [23–25], although Malin et al.’s study found elevation of TH (r-T3) in the cerebrospinal fluid in 12 definite ALS patients [26]. Furthermore, no prolonged lifespan was observed in hypometabolism in SOD1-G93A mice treated with methimazole and calorie restriction [19].
TH has been demonstrated to play direct roles in the proliferations and differentiations of neuronal cell and glial cells [14], but also indirect actions through the presence of TH receptors, which have been demonstrated in cultured astrocytes [27]. On the other hand, there was evidence of TH action on the neuronal–glial interactions. In vitro, TH has been demonstrated to regulate the expression of extracellular matrix and adhesion molecules that are important for neuronal migration and development, such as tenascin- C [28], neural cell adhesion molecule [29], laminin and fibronectin [30–32]. And in vivo, TH was proved to be important in the Xenopus spinal cord neurogenesis by comparing between controls and those with injections of different dosage of T3, which indicated that TH administrations could result in increased numbers of neurons and up-regulate the neurogenesis of Xenopus spinal cord.
Taken together, despite the restrictions of study designs and sample sizes, the inconsistent views drawn by in vitro, in vivo and human studies indicate that the regulation of neuronal cells in human subjects may involve more mechanism, but not simply through TH regulation.
Our study and together with those basic studies give the evidence that TH does not correlate with survival time in ALS and is not a prognostic factor for ALS patients.
References
Brooks BR, Sanjak M, Belden D, Juhasz-Poscine K, Waclawik A (eds) (2000) Natural history of amyotrophic lateral sclerosis. Dunitz, London
Dupuis L, Corcia P, Fergani A, Gonzalez De Aguilar J-L, Bonnefont-Rousselot D, Bittar R, Seilhean D, Hauw J-J, Lacomblez L, Loeffler J-P, Meininger V (2008) Dyslipidemia is a protective factor in amyotrophic lateral sclerosis. Neurology 70(13):1004–1009
Hiroo Ichikawa MK (2010) Language impairment in amyotrophic lateral sclerosis. Brain Nerve 62:435–440
Donaghy C, Thurtell MJ, Pioro EP, Gibson JM, Leigh RJ (2011) Eye movements in amyotrophic lateral sclerosis and its mimics: a review with illustrative cases. J Neurol Neurosurg Psychiatry 82:110–116
Hammad M, Silva A, Glass J, Sladky JT, Benatar M (2007) Clinical, electrophysiologic, and pathologic evidence for sensory abnormailities in ALS. Neurology 69:2236–2242
Bouteloup C, Desport JC, Clavelou P, Guy N, Derumeaux-Burel H, Ferrier A, Couratier P (2009) Hypermetabolism in ALS patients: an early and persistent phenomenon. J Neurol 256:1236–1242. doi:10.1007/s00415-009-5100-z
Desport JC, Torny F, Lacoste M, Preux PM, Couratier P (2005) Hypermetabolism in ALS: correlations with clinical and paraclinical parameters. Neurodegener Dis 2:202–207. doi:10.1159/000089626
Dupuis L, Corcia P, Fergani A, Gonzalez De Aguilar JL, Bonnefont-Rousselot D, Bittar R, Seilhean D, Hauw JJ, Lacomblez L, Loeffler JP, Meininger V (2008) Dyslipidemia is a protective factor in amyotrophic lateral sclerosis. Neurology 70:1004–1009. doi:10.1212/01.wnl.0000285080.70324.27
Paganoni S, Zhang M, Quiroz Zarate A, Jaffa M, Yu H, Cudkowicz ME, Wills AM (2012) Uric acid levels predict survival in men with amyotrophic lateral sclerosis. J Neurol 259:1923–1928. doi:10.1007/s00415-012-6440-7
Harno K, Rissanen A, Palo J (1984) Glucose tolerance in amyotrophic lateral sclerosis. Acta Neurol Scand 70:451–455
Reyes ET, Perurena OH, Festoff BW, Jorgensen R, Moore WV (1984) Insulin resistance in amyotrophic lateral sclerosis. J Neurol Sci 63:317–324
Shulga A, Rivera C (2012) Interplay between Thyroxin, BDNF and GABA in injured neurons. Neuroscience 239:241–252. doi:10.1016/j.neuroscience.2012.12.007
Sampson D, Pickard M, Evans I, Leonard A, Sinha A, Ekins R (2002) Thyroid hormone regulates the expression of alpha-internexin in neurons in culture. NeuroReport 13:273–276
Konig S, Moura Neto V (2002) Thyroid hormone actions on neural cells. Cell Mol Neurobiol 22:517–544
Schlosser G, Koyano-Nakagawa N, Kintner C (2002) Thyroid hormone promotes neurogenesis in the Xenopus spinal cord. Dev Dyn 225:485–498. doi:10.1002/dvdy.10179
Funalot B, Desport JC, Sturtz F, Camu W, Couratier P (2009) High metabolic level in patients with familial amyotrophic lateral sclerosis. Amyotroph Lateral Scler 10:113–117. doi:10.1080/17482960802295192
Cozzolino M, Ferri A, Valle C, Carri MT (2012) Mitochondria and ALS: implications from novel genes and pathways. Mol Cell Neurosci. doi:10.1016/j.mcn.2012.06.001
Hamadeh MJ, Rodriguez MC, Kaczor JJ, Tarnopolsky MA (2005) Caloric restriction transiently improves motor performance but hastens clinical onset of disease in the Cu/Zn-superoxide dismutase mutant G93A mouse. Muscle Nerve 31:214–220. doi:10.1002/mus.20255
Li J, Paulson JM, Ye FD, Sung M, Hollenberg AN, Rutkove SB (2012) Reducing systemic hypermetabolism by inducing hypothyroidism does not prolong survival in the SOD1-G93A mouse. Amyotroph Lateral Scler 13:372–377. doi:10.3109/17482968.2012.662988
Zoccolella S, Beghi E, Palagano G, Fraddosio A, Guerra V, Samarelli V, Lepore V, Simone IL, Lamberti P, Serlenga L, Logroscino G (2008) Predictors of long survival in amyotrophic lateral sclerosis: a population-based study. J Neurol Sci 268:28–32. doi:10.1016/j.jns.2007.10.023
Pallavi C, Bhautik M, Sarita M, Pranay J, Rita S (2011) Variation in thyroid hormones level among people of different age, gender and seasons, Piparia, Gujarat. Natl J Med Res 2:57–59
Jang YY, Kim CY, Hwang TY, Kim KD, Lee CH (2008) Reference interval of serum thyroid hormones in healthy Korean adults. J Prev Med Public Health 41:128–134 [pii] 200803128
Iwasaki Y, Kinoshita M, Ikeda K, Takamiya K, Shiojima T (1989) Amyotrophic lateral sclerosis and thyroid function. J Neurol 236:373–374
Ilzecka J, Stelmasiak Z (2003) Thyroid function in patients with amyotrophic lateral sclerosis. Ann Univ Mariae Curie Sklodowska Med 58:343–347
Kiessling WR (1982) Thyroid function in 44 patients with amyotrophic lateral sclerosis. Arch Neurol 39:241–242
Malin JP, Kodding R, Fuhrmann H, von zur Muhlen A (1989) T4, T3 and rT3 levels in serum and cerebrospinal fluid of patients with amyotrophic lateral sclerosis. J Neurol 236:57–59
Trentin AG (2006) Thyroid hormone and astrocyte morphogenesis. J Endocrinol 189:189–197. doi:10.1677/joe.1.06680
Alvarez-Dolado M, Gonzalez-Sancho JM, Bernal J, Munoz A (1998) Developmental expression of the tenascin-C is altered by hypothyroidism in the rat brain. Neuroscience 84:309–322 [pii] S0306452297005113
Iglesias T, Caubin J, Stunnenberg HG, Zaballos A, Bernal J, Munoz A (1996) Thyroid hormone-dependent transcriptional repression of neural cell adhesion molecule during brain maturation. EMBO J 15:4307–4316
Trentin AG, Moura Neto V (1995) T3 affects cerebellar astrocyte proliferation, GFAP and fibronectin organization. NeuroReport 6:293–296
Martinez R, Gomes FC (2005) Proliferation of cerebellar neurons induced by astrocytes treated with thyroid hormone is mediated by a cooperation between cell contact and soluble factors and involves the epidermal growth factor-protein kinase a pathway. J Neurosci Res 80:341–349. doi:10.1002/jnr.20463
Trentin AG, De Aguiar CB, Garcez RC, Alvarez-Silva M (2003) Thyroid hormone modulates the extracellular matrix organization and expression in cerebellar astrocyte: effects on astrocyte adhesion. Glia 42:359–369. doi:10.1002/glia.10228
Conflict of interest
The authors report no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zheng, Z., Guo, X., Huang, R. et al. An exploratory study of the association between thyroid hormone and survival of amyotrophic lateral sclerosis. Neurol Sci 35, 1103–1108 (2014). https://doi.org/10.1007/s10072-014-1658-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-014-1658-z