Abstract
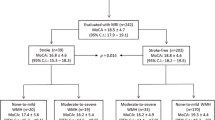
Although some studies have supported the association between white matter hyperintensities (WMH) and cognitive impairment, whether WMH are associated with the impairments in instrumental activities of daily living (IADLs) remains unknown. This cross-sectional study investigated differences in basic ADLs and IADLs among different severity of WMH in a large, well-defined registry of patients with amnestic mild cognitive impairment (aMCI). 1,514 patients with aMCI were divided into three groups according to the degree of WMH (1,026 mild, 393 moderate, and 95 severe). We compared the total IADL scores and analyzed the prevalence of the impairment for each IADL item for each group. The severity of WMH was associated with the impairments in IADLs. Among 15 Seoul IADL items, “using public transportation”, “going out (short distance)”, “grooming” and “participating in leisure activities/hobbies” showed greater positive association with the severity of WMH. WMH in patients with aMCI were associated with the impairments in IADLs but not in basic ADLs. These findings are likely to be more obvious with respect to using public transportation, going out (short distances), shopping, grooming and participating in leisure activities/hobbies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cerebral white matter hyperintensities (WMH) are relatively common in elderly individuals. Several studies, including the Leukoaraiosis and Disability (LADIS) study, found the association of WMH not only with cognitive dysfunctions [1–6] but also with problems with mobility, motor performance [7, 8], and urination [9, 10] in normal elderly people and Alzheimer’s disease (AD) with WMH. Moreover, The LADIS study demonstrated that the severity of WMH affected functional abilities, that is, baseline severe WMH had independent predictor of disability as well as association with worse functional status [11–13]. In addition, recent study has shown that WMH are negatively associated with instrumental ADL (IADL) and physical ADL in dementia [5, 14]. Although previous studies have demonstrated that WMH were related to cognitive decline among those with mild cognitive impairment (MCI), known prodromal AD dementia [15–17], the association between WMH and IADL in MCI remains unknown. Since IADL needs higher complex cognitive demand than basic ADL, it could be more sensitive and useful marker for detecting very subtle changes in functional abilities. In 2004, the International Working Group on MCI proposed the inclusion of “preserved basic ADL with some minimal impairment in complex instrumental functions” in the diagnostic criteria of MCI [18]. However, there is currently no consensus regarding not only which IADLs are affected in MCI but also which IADLs are related to WMH in MCI. Luck et al. [19] have found that when IADL was considered as part of the criteria for diagnosing MCI, reversion rates from MCI to normal decreased from 35 to 11 %. We hypothesized that WMH would have more influence on IADLs. The purpose of the present study was to determine the relationship between WMH and IADLs and to identify which functional abilities of IADLs are influenced by WMH in a large, well-defined registry of patients with amnestic MCI (aMCI).
Methods
Subjects
A total of 1,514 patients with aMCI were consecutively recruited from 43 dementia clinics in university-affiliated hospitals in South Korea from November 2005 to March 2009. This study was performed as part of the national multicenter study on dementia: the Clinical Research Center for Dementia of South Korea (CREDOS) study. It was a large, well-defined, hospital-based registry. The CREDOS study had aimed to understand the characteristics of Korean patients with dementia. It had developed common protocols, including its own ischemic scale, and recruited patients with subjective memory impairment, MCI, AD, and vascular dementia. This study was approved by the Institutional Review Boards of all participating hospitals, and written informed consents were obtained from the patients and their caregivers after they received a complete description of the study.
We generally adhered to the diagnostic criteria for aMCI defined by Petersen et al. [20] and Winblad et al. [18]. The inclusion criteria for aMCI were as follows: (1) memory complaints by patients and caregivers; (2) objective cognitive impairment (at least 1.0 SD below age- and education-adjusted norms) in memory only or memory and ≥1 other cognitive domain (executive functioning, language or visuospatial abilities) in standard neuropsychological tests; (3) normal functional activities; (4) Clinical Dementia Rating (CDR) [21] scores of 0.5; and (5) ‘not demented’ according to the DSM-IV criteria. We excluded the patients with hemiparesis or a history of clinical stroke because these events could affect their physical activity. Additionally, we excluded the patients with histories of neurological disorders (e.g., active epilepsy) or psychiatric illnesses (e.g., schizophrenia, cognitive developmental delay, major depression, and mania), those taking psychotropic medications, and those in significant alcohol and/or other substance abuse. Patients were also excluded if the presence of the secondary causes of cognitive deficits had been suggested by abnormal laboratory findings including complete blood counts, blood chemistry, vitamin B12/folate levels, syphilis serology and thyroid function tests. We also excluded those with large-territory infarctions and those exhibiting high MRI signal abnormalities that were related to brain tumors, radiation injury, hippocampal sclerosis, and multiple sclerosis according to brain MRIs conducted to detect organic brain lesions that were related to cognitive impairment.
Cognitive and functional assessments
We used the Barthel Index of ADL (B-ADL) (ratings between 0 and 20, with higher scores reflecting lower levels of dependence) [22] to evaluate basic ADLs and the Seoul-Instrumental Activities of Daily Living (S-IADL) (Table 3) [23] to evaluate IADLs.
S-IADL is a caregiver-administered instrument designed to measure IADLs. This questionnaire was completed by the informants after they have received appropriate instructions and while the patients were undergoing neuropsychological assessment. The S-IADL consisted of 15 items: using the telephone, shopping, preparing food/cooking, household chores, using public transportation, going out (short distances), taking medication, managing finances, grooming, using household appliances, managing belongings, locking a door, keeping appointments, talking about recent events and participating in leisure activities/hobbies. All items in the S-IADL were scored on a 4-point scale ranging from 0 to 3; 0 indicates normal performance, and higher scores indicate poorer performance on IADLs. All S-IADL items had been carefully reviewed by experts at the meetings in which they were adopted with consensus and, in addition, had been validated to be the items widely practiced in the Republic of Korea [5, 14].
Cognitive functions were assessed by neuropsychologists with a standard comprehensive neuropsychological battery, which was composed of cognitive subsets for attention and working memory (digit span-forward/backward), visuospatial function (Rey–Osterrieth Complex Figure test [RCFT]), language (Korean version of Boston Naming Test), verbal memory (Seoul Verbal Learning Test, which is the modified Korean version of the Hopkins Verbal Learning Test-immediate/delayed recall), visual memory (RCFT-immediate/delayed recall) and frontal lobe function (Word fluency test-semantic/phonemic, Stroop-word/color reading test).
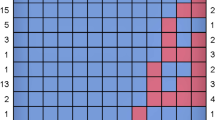
Assessment of WMH
All subjects received an MRI scan using a standard protocol. MRI scans performed at each center using 1.5 or 3.0 T MRI with anterior commissure–posterior commissure line as a reference. MRIs were set as ideal parameters on their own. Axial T2, T1 and fluid attenuated inversion recovery (FLAIR) images were cut in 5 mm thickness without gap. The severity of WMH was rated based on the FLAIR sequences. The neurologist and radiologist who worked at the attended centers performed rating and, if there is a case with debatable rating at each center, the central committee members decided the rating again after discussion. The CREDOS white matter (WM) rating scales were developed by the central committee of the CREDOS study and modified using the scales developed by Fazekas [24] and Scheltens [25]. The longest diameter WMH around the lateral ventricles (capping or banding on the periventricular areas) or deepest WMH (especially in the centrum semiovale) was evaluated separately. Periventricular WMH were rated as P1 (<5 mm), P2 (≥5 mm, <10 mm) or P3 (≥10 mm), and deep WMH were rated as D1 (<10 mm), D2 (≥10 mm, < 25 mm) or D3 (≥25 mm). Periventricular and deep WMH were combined to produce the final scores for mild, moderate or severe degree. The combinations of D1 with P1 (D1P1) and of D1 with P2 (D1P2) were classified as “mild”. Combinations of D2P1, D3P1, D2P2, D3P2, D1P3 and D2P3 were classified as “moderate”, whereas D3P3 was classified as “severe”. Table 1 summarized the information given above. For assessing the reliability, 138 MRI scans were randomly selected and rated by two neurologists. The inter-rater reliabilities for the periventricular WMH (κ = 0.595), deep WMH (κ = 0.787), and WMH (κ = 0.785) were good as well as intra-rater reliabilities of the WMH including periventricular and deep WMH (κ = 0.694–0.979) were also satisfactory [5, 6, 14, 26]. We divided participants into three groups according to the severity of their WMH.
Statistical Analysis
We used the Chi-square test for categorical variables and Analysis of Variance (ANOVA) and Tukey’s post hoc analysis for continuous variables. We compared the proportion of patients in each group who showed abnormal performance in each S-IADL item using Analysis of Covariance (ANCOVA) adjusted for age and hypertension. We estimated the adjusted odds ratios (OR) and corresponding 95 % confidence intervals (CI) for each 1-point increase in the scores (from the absence to the presence of each dysfunction) for each item of the S-IADL for different the severity of WMH in patients with aMCI (mild vs. moderate group, mild vs. severe group, moderate vs. severe group) using a logistic regression analysis after controlling for age and hypertension. Statistical analyses of groups were performed using SPSS for Windows ver. 12.0 (SPSS, Chicago, IL, USA). The significance level was set to P < 0.05.
Results
Demographics and clinical characteristics of the groups
Of a total of 1,514 patients, 1,026 (67.7 %) had mild, 393 (26.0 %) had moderate and 95 (6.3 %) had severe WMH. Patients with severe WMH had the oldest mean age and highest percentage of hypertension, followed by, in order of, those with moderate WMH and those with mild WMH (P < 0.0001). The groups differed significantly with respect to the HIS (P < 0.0001). No significant differences among the groups were observed in terms of educational level, diabetes mellitus, heart disease, hyperlipidemia or scores on the Korean version Mini-mental state examination, CDR-SB, GDS and B-ADL (Table 2).
IADLs
The total S-IADL score was highest in patients with severe WMH, followed by, in order of, those with moderate WMH and those with mild WMH (P < 0.0001). The three groups showed different results in public transportation, grooming and participating in leisure activities/hobbies after the adjustment for both age and hypertension (Table 2). Of the 15 S-IADL items, the moderate-WMH group showed higher ORs than the mild-WMH group in: (1) shopping (OR = 1.85, 95 % CI = 1.26–2.72, P = 0.002); (2) grooming (OR = 2.43, 95 % CI = 1.12–5.24, P = 0.024); and (3) participating in leisure activities/hobbies (OR = 1.82, 95 % CI = 0.97–3.10, P = 0.027). The severe-WMH group demonstrated higher ORs than the mild-WMH group in: (1) using public transportation (OR = 1.81, 95 % CI = 1.08–3.02, P = 0.024); (2) going out (short distances) (OR = 2.29, 95 % CI = 1.06–4.94, P = 0.035); (3) taking medication (OR = 2.15, 95 % CI = 1.26–3.67, P = 0.005); (4) grooming (OR = 4.09, 95 % CI = 1.42–11.76, P = 0.009); and (5) participating in leisure activities/hobbies (OR = 2.11 95 % CI = 1.27–3.51, P = 0.004) after the adjustment for age and hypertension (Table 3). No variables except grooming had statistically significant higher ORs (OR = 1.92, 95 % CI = 1.13–3.36, P = 0.041) in the severe-WMH group than in the moderate-WMH group (Table 4).
Discussion
The aim of this study was to compare the IADLs among three groups of aMCI patients with different severity of WMH. In this large, well-defined aMCI registry, we found that the degree of WMH was associated with the impairments in IADLs.
This study showed that patients with aMCI with severe WMH were more likely to have more frequent and more severe impairments in IADLs, which corresponds well with the findings of previous studies on dementia which reported that IADL functions were related to WMH severity [5, 14] as well as a study on a cohort of stroke patients which reported that IADL functions were independent correlates of severe WMH [27]. Impairments in cognitive functions such as execution, planning and mental processing that are connected to the severity of WMH may affect the individual and social performances of complex activities, which can contribute to the impaired IADLs.
Among S-IADL items, poorer performances in using public transportation, going out (short distance) and participating in leisure activities/hobbies according to the severity of WMH coincide well with the results of Moon et al. [14]. This could imply that WMH in aMCI and dementia commonly influence poorer performances of these activities. Especially, using public transportation and going out (short distance) in the absence of definitive impairment in basic ADLs may represent the compensatory changes that are related to WMH, which is consistent with the results showing that WMH were related to functional changes in the organization of the motor network for lower-limb movements [28]. In other words, WMH may lead to disturbed movement preparation and motor execution by disrupting the frontosubcortical loops, which may then lead to poorer performance in these two areas. In addition, we found that shopping, grooming and participating in leisure activities/hobbies were closely correlated with the severity of WMH. The significant differences in these items among three groups may be explained by decreased interest, worrisomeness or apathy which was associated with WMH [29]. This were also supported by our sub-analysis results that the frequency score of apathy in NPI was shown statistical significance (P = 0.032), that is, the frequency of apathy have increased as WMH severity have worsened, although there were no statistical significance in the composite score (frequency x severity) of apathy in NPI (Data was not presented).
The present study has several limitations. First, the incidences of WMH increase with age. Thus, the sample used was unbalanced with regard to the age. We therefore corrected all analyses by including age as a covariate. Nevertheless, it is likely that the differences observed resulted from the interactions between the effects of aging on IADLs and WMH rather than from the effects of WMH alone. Second, this study focused on WMH rather than on other differences (e.g., lacunar infarcts and hippocampal atrophy), which may also has affected the functional performances of the groups. Third, this study used a cross-sectional design. Nevertheless, the strengths of the study include its large sample size, the standardized assessment of WMH and the detailed clinical evaluation. Moreover, to our knowledge, this study was the first to have conducted a detailed analysis of the impact of WMH on IADLs in patients with aMCI. The longitudinal observation of these patients will clarify whether WMH independently predict overt functional impairment in IADLs in patients with aMCI.
Taken together, our findings suggest that WMH are associated with impaired IADLs in patients with aMCI. Furthermore, severe WMH may be associated with greater impairments in ‘using public transportation’ and ‘going out (short distance)’, which may be related to functional decline in mobility, ‘shopping’, ‘grooming’ and ‘participation in leisure activities/hobbies’, which may, in turn, be related to the loss of interest/worrisomeness or apathy.
References
Poggesi A, Pantoni L, Inzitari D, Fazekas F, Ferro J, O’Brien J, Hennerici M, Scheltens P, Erkinjuntti T, Visser M, Langhorne P, Chabriat H, Waldemar G, Wallin A, Wahlund A (2011) 2001–2011: A decade of the ladis (leukoaraiosis and disability) study: What have we learned about white matter changes and small-vessel disease? Cerebrovasc Dis 32:577–588
Au R, Massaro J, Wolf P, Young M, Beiser A, Seshadri S, D’Agostino R, DeCarli C (2006) Association of white matter hyperintensity volume with decreased cognitive functioning: The Framingham Heart Study. Arch Neurol 63:246–250
De Groot J, de Leeuw F, Oudkerk M, van Gijn J, Hofman A, Jolles J, Breteler M (2000) Cerebral white matter hyperintensities and cognitive function: The Rotterdam Scan Study. Ann Neurol 47:145–151
Gouw AA, van der Flier WM, van Straaten EC, Barkhof F, Ferro JM, Baezner H, Pantoni L, Inzitari D, Erkinjuntti T, Wahlund LO, Waldemar G, Schmidt R, Fazekas F, Scheltens P (2006) Simple versus complex assessment of white matter hyperintensities in relation to physical performance and cognition: The LADIS study. J Neurol 253:1189–1196
Kee Hyung P, Lee JY, Na DL, Kim SY, Cheong HK, Moon SY, Shim YS, Park KW, Ku BD, Choi SH, Joo H, Lee JS, Go SM, Kim SH, Kim S, Cha KR, Lee J, Seo SW (2011) Different associations of periventricular and deep white matter hyperintensities with cognition, neuropsychiatric symptoms, and daily activities in dementia. J Geriatr Psychiatry Neurol 24:84–90
Ku BD, Na DL, Moon SY, Kim SY, Seo SW, Cheong HK, Park KW, Park KH, Lee JY, Cha KR, Shim YS, Youn YC, Chung CS, Kim JE, Kang HY, Choi SH, Han SH (2011) Neuropsychological correlates of the proportional impact of white matter hyperintensities on mild to moderate dementia: the MRI 300 study. Dement Geriatr Cogn Disord 31:397–405
Baezner H, Blahak C, Poggesi A, Pantoni L, Inzitari D, Chabriat H, Erkinjuntti T, Fazekas F, Ferro JM, Langhorne P, O’Brien J, Scheltens P, Visser MC, Wahlund LO, Waldemar G, Wallin A, Hennerici MG (2008) Association of gait and balance disorders with age-related white matter changes: The LADIS study. Neurology 70:935–942
Moscufo N, Guttmann CR, Meier D, Csapo I, Hildenbrand PG, Healy BC, Schmidt JA, Wofson L (2011) Brain regional lesion burden and impaired mobility in the elderly. Neurobiol Aging 32:646–654
Poggesi A, Pracucci G, Chabriat H, Erkinjuntti T, Fazekas F, Verdelho A, Hennerici M, Langhorne P, O’Brien J, Scheltens P, Visser MC, Crisby M, Waldemar G, Wallin A, Inzitari D, Pantoni L (2008) Urinary complaints in nondisabled elderly people with age-related white matter changes: The leukoaraiosis and disability (LADIS) study. J Am Geriatr Soc 56:1638–1643
Wakefield DB, Moscufo N, Guttmann CR, Kuchel GA, Kaplan RF, Pearlson G, Wolfson L (2010) White matter hyperintensities predict functional decline in voiding, mobility, and cognition in older adults. J Am Geriatr Soc 58:275–281
Pantoni L, Poggesi A, Basile AM, Pracucci G, Barkhof F, Chabriat H, Erkinjuntti T, Ferro JM, Hennerici M, O’Brien J, Schmidt R, Visser MC, Wahlund LO, Waldemar G, Wallin A, Inzitari D (2006) Leukoaraiosis predicts hidden global functioning impairment in nondisabled older people: The LADIS (leukoaraiosis and disability in the elderly) study. J Am Geriatr Soc 54:1095–1101
Inzitari D, Pracucci G, Poggesi A, Carlucci G, Barkhof F, Chabriat H, Erkinjuntti T, Fazekas F, Ferro JM, Hennerici M, Langhorne P, O’Brien J, Scheltens P, Visser MC, Wahlund LO, Waldemar G, Wallin A, Pantoni L (2009) Changes in white matter as determinant of global functional decline in older independent outpatients: three year follow-up of LADIS (leukoaraiosis and disability) study cohort. BMJ 339:b2477
Inzitari D, Simoni M, Pracucci G, Poggesi A, Basile AM, Chabriat H, Erkinjuntti T, Fazekas F, Ferro JM, Hennerici M, Langhorne P, O’Brien J, Barkhof F, Visser MC, Wahlund LO, Waldemar G, Wallin A, Pantoni L (2007) Risk of rapid global functional decline in elderly patients with severe cerebral age-related white matter changes: The LADIS study. Arch Intern Med 167:81–88
Moon SY, Na DL, Seo SW, Lee JY, Ku BD, Kim SY, Park KW, Shim YS, Youn YC, Chung CS, Cheong HK, Choi SH, Cha KR, Kim JE, Jeong JH (2011) Impact of white matter changes on activities of daily living in mild to moderate dementia. Eur Neurol 65:223–230
Bombois S, Debette S, Delbeuck X, Bruandet A, Lepoittevin S, Delmaire C, Leys D, Pasquier F (2007) Prevalence of subcortical vascular lesions and association with executive function in mild cognitive impairment subtypes. Stroke 38:2595–2597
Debette S, Bombois S, Bruandet A, Delbeuck X, Lepoittevin S, Delmaire C, Leys D, Pasquier F (2007) Subcortical hyperintensities are associated with cognitive decline in patients with mild cognitive impairment. Stroke 38:2924–2930
Frisoni GB, Galluzzi S, Bresciani L, Zanetti O, Geroldi C (2002) Mild cognitive impairment with subcortical vascular features. J Neurol 249:1423–1432
Winblad B, Palmer K, Kivipelto M, Jelic V, Fratiglioni L, Wahlund LO, Nordberg A, Bäckman L, Albert M, Almkvist O, Arai H, Basun H, Blennow K, de Leon M, DeCarli C, Erkinjuntti T, Giacobini E, Graff C, Hardy J, Jack C, Jorm A, Ritchie K, van Duijn C, Visser P, Petersen RC (2004) Mild cognitive impairment-beyond controversies, towards a consensus: report of the International Working Group on Mild Cognitive Impairment. J Intern Med 256:240–246
Luck T, Luppa M, Angermeyer MC, Villringer A, Konig HH, Riedel-Heller SG (2011) Impact of impairment in instrumental activities of daily living and mild cognitive impairment on time to incident dementia: results of the Leipzig Longitudinal Study of the Aged. Psychol Med 41:1087–1097
Petersen RC, Stevens JC, Ganguli M, Tangalos EG, Cummings JL, DeKosky ST (2001) Practice parameter: early detection of dementia: mild cognitive impairment (an evidence-based review). Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology 56:1133–1142
Morris JC (1993) The Clinical Dementia Rating (CDR): current version and scoring rules. Neurology 43:2412–2414
Mahoney FI, Barthel DW (1965) Functional evaluation: the barthel index. Md State Med J 14:61–65
Ku H, Kim J, Kwon E, Kim S, Lee H, Ko H, Jo S, Kim D (2004) A study on the reliability and validity of Seoul-instrumental activities of daily living (S-IADL). J Korean Neuropsychiatr Assoc 43:189–199
Fazekas F, Chawluk J, Alavi A, Hurtig H, Zimmerman R (1987) MR signal abnormalities at 1.5 T in Alzheimer’s dementia and normal aging. Am J Roentgenol 149:351–356
Scheltens P, Barkhof F, Leys D, Pruvo JP, Nauta JJ, Vermersch P, Steinling M, Valk J (1993) A semiquantative rating scale for the assessment of signal hyperintensities on magnetic resonance imaging. J Neurol Sci 114:7–12
Shim YS, Youn YC, Na DL, Kim SY, Cheong HK, Moon SY, Park KW, Ku BD, Lee JY, Jeong JH, Kang H, Kim EJ, Lee JS, Go SM, Kim SH, Cha KR, Seo SW (2011) Effects of medial temporal atrophy and white matter hyperintensities on the cognitive functions in patients with Alzheimer’s disease. Eur Neurol 66:75–82
Pohjasvaara TI, Jokinen H, Ylikoski R, Kalska H, Mantyla R, Kaste M, Erkinjuntti T (2007) White matter hyperintensities are related to impaired instrumental activities of daily living poststroke. J Stroke Cerebrovasc Dis 16:251–258
Linortner P, Fazekas F, Schmidt R, Ropele S, Pendl B, Petrovic K, Loitfelder M, Neuper C, Enzinger C (2010) White matter hyperintensities alter functional organization of the motor system. Neurobiol aging
Cacciari C, Moraschi M, Paola MD, Cherubini A, Orfei MD, Giove F, Maraviglia B, Caltagirone C, Spalletta G (2010) White matter microstructure and apathy level in amnestic mild cognitive impairment. J Alzheimers Dis 20:501–507
Acknowledgments
This study was supported by a grant of the Korea Healthcare technology R&D Project, Ministry of Health and Welfare, Republic of Korea. (A102065).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yoon, B., Shim, Y.S., Kim, YD. et al. Correlation between instrumental activities of daily living and white matter hyperintensities in amnestic mild cognitive impairment: results of a cross-sectional study. Neurol Sci 34, 715–721 (2013). https://doi.org/10.1007/s10072-012-1120-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-012-1120-z