Abstract
The Sunnybrook Facial Grading System (SFGS) is one of the most employed scales to assess the severity of facial palsy. The aim of our study was to produce an Italian version of the SFGS and of its explanatory criteria, and to test their measurement properties when employed by Italian physicians. A multidisciplinary committee translated and adapted the scale and its criteria into Italian. Six native Italian physicians, four of whom experienced in facial palsy and two novices, rated independently 29 videos of facial palsy patients twice. Internal consistency, agreement and repeatability were evaluated. The Italian version of the SFGS showed a high degree of internal consistency with a Cronbach’s α of 0.91. The test–retest reliability was high for both inter-rater and intra-rater measures with an ICC of 0.96 and 0.98, respectively. The scores given by the novice physicians were comparable with the scores given by the expert physicians. Our study suggests that the Italian version of the SFGS has excellent internal consistency and reproducibility, comparable to the original scale. Our study confirms in an independent case record the high measurement properties of SFGS and provides the first validated Italian scale for the assessment of facial palsy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Facial palsy is the most common disease of the cranial nerves and leads to facial disfigurement and functional limitations [1, 2]. The disease presents a wide clinical spectrum and has numerous etiologies [3]. Over the years, a large number of grading systems for facial function have been proposed, but there has long been the need for a universally accepted method to assess the severity of facial palsy and to monitor its clinical course [4]. Such a method would allow the results of different clinical trials to be systematically compared [5].
In 1996, Ross et al. [6] introduced the Sunnybrook Facial Grading System (SFGS), a scale used to assess facial function. This scale provides a clinical score from 0 to 100 which combines a static and dynamic assessment of facial muscles with the degree of synkinesis. This system was proved to have high internal consistency, elevated repeatability and good sensitivity to clinical changes [6, 7]. Furthermore the scale showed a good correlation with other grading systems in use, including the House-Brackmann, Yanagara and Sidney scales [8–10]. Various authors have declared SFGS to be the best grading system available for facial palsy and have encouraged its usage and diffusion over other methods [7–9].
Despite this recommendation, the SFGS is underemployed by the Italian medical community. This might be due to the idiomatic English expressions used in the scale. Moreover, the system is not intuitive, especially for novice users. To complete the scale, Neely et al. [5] have recently published explanatory criteria which are admittedly aimed at reducing potential ambiguities.
This study aims to produce an Italian version of the SFGS and of its explanatory criteria, and to test the measurement properties of the scale by native Italian speaking physicians.
Materials and methods
The Italian version of the SFGS
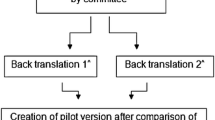
In accordance with the international guidelines for translation and cross-cultural adaptation [11], the original version of the SFGS and its explanatory criteria were independently translated into Italian by two Italian physicians who were fluent in English and familiar with the original version of the scale (versions 1 and 2).
Subsequently, a committee of three Italian physicians with experience in facial palsy rehabilitation compared the Italian versions 1 and 2 and compiled a consensus version, which they considered to be linguistically and culturally appropriate (version 3). Version 3 of the Italian translation was then translated back into English by a native English speaking professional translator with experience in medical writing (version 4).
Finally, in order to agree on the definitive Italian version of the SFGS, a large committee of six physicians with various backgrounds and the professional translator systematically compared the original version, version 3 and version 4 of the SFGS by examining the semantic correspondence and the cultural adaptations. Figure 1 illustrates the translation and cross-cultural adaptation procedure.
As the original version [6], the Italian SFGS (Fig. 2) provides a clinical composite score from 0, for complete facial paralysis, to 100, for normal facial function, considering the symmetry at rest and during voluntary movements, and the presence and severity of synkinesis. The criteria for grading give a guide for the evaluation procedure (Fig. 3). Resting symmetry is assessed by comparison of the paralysed half face with the normal side at rest, evaluating the palpebral fissure, the naso-labial fold and the mouth. The symmetry of voluntary movement is evaluated by means of five standard expressions (wrinkling the forehead, closing eyes gently, snarling, smiling with the mouth open and puckering the lips), assessing the degree of maximal excursion of affected facial muscles compared with the normal side and grading on a five-point scale from 1 (no movement) to 5 (movement complete). The degree of synkinesis associated with each of the five standard facial expressions is graded on a four-point scale from 0 (no synkinesis) to 3 (severe synkinesis). The scores are then weighted: the resting symmetry score is multiplied by five, and the voluntary movement score is multiplied by four. The composite score is obtained by subtracting the resting symmetry and synkinesis scores from the voluntary movement score.
Validation procedures
Six Italian physicians used the Italian version of the SFGS (Fig. 2) and its explanatory criteria (Fig. 3) to independently assess the severity in 29 clinical evaluations of patients affected by unilateral peripheral facial palsy, each recorded on video.
Prior to rating the 29 videos of facial palsy patients independently, the physicians underwent a short group training session during which they read and discussed the Italian version of the SFGS and its explanatory criteria and collectively filled in the scale while evaluating 5 videos of healthy subjects and 10 videos of patients with varying degrees of facial palsy which were all taken from the video database at our Rehabilitation Unit. Videos of these 15 subjects were not included to test the measurement properties of the scale.
The physicians were not allowed to take notes while independently observing the 29 videos of facial palsy patients, and they had no further access to either the videos or the scores.
One month after this first observation, the same physicians were independently shown the same videos, in a random order, and they re-assessed the severity of facial palsy using the Italian version of the SFGS and its explanatory criteria.
Video recording
Video recording of each patient was performed at the beginning of the clinical evaluation with a standardized procedure. All patients were recorded by the same operator with a Casio EXILIM High Speed EX-F1, while sitting in the same position. First, the face at rest was recorded for 5 s and then the five facial expressions of the SFGS were recorded. Each movement was repeated three times and kept for 5 s. This setting was meant to reproduce a typical clinical evaluation performed for facial palsy patients at our clinic.
Operators
The six Italian physicians who rated the 29 videos were: a specialist in neurology and rehabilitation with 20 years’ experience in the treatment of facial palsy (expert), three physicians with more than 1 year’s experience in the treatment of facial palsy (experienced), and two physicians with no previous experience in the treatment of patients with facial palsy (novices).
Patients
Inclusion criteria
-
Videos of consecutive patients affected by unilateral peripheral facial palsy evaluated at the Rehabilitation Unit, Fondazione IRCCS Policlinico San Matteo, Pavia, between September and December 2010 who gave their written informed consent for the recording of audiovisual material and its usage for research purposes, according to our Institutional Ethics Board requirements.
Exclusion criteria
-
Incomplete videos lacking one or more expressions that are part of the scale.
-
Patients with other pathologic facial alterations.
Control group
To assess content of validity of the Italian version of SFGS, two experienced observers rated independently 29 videos of healthy subjects, age and gender matched to the patients.
Statistical analysis
Categorical variables were presented by numbers and percentages, quantitative variables by mean and standard deviation or median and interquartile range, as appropriate. The internal consistency reliability of the scale was determined by calculating Cronbach’s α. The intraclass correlation coefficient (ICC) was used to measure the correlation within and between operators for the 17 items of the SFGS. ICC 95 % confidence interval (95 % CI) was also presented. According to Altman and Bland [12], the agreement within and between raters on composite score was assessed by the coefficient of repeatability (CR) as well: CR is a precision measure which represents the value below which the absolute difference between two repeated test results may be expected to lie with a probability of 95 %. The comparison between groups was performed using a t test and Kruskal–Wallis test, as appropriate. Statistical analysis was performed with Stata 11.2 software (StataCorp, College Station, TX, USA).
Results
The study included 29 videos of 23 patients (6 of whom were subsequently reassessed) with unilateral peripheral facial palsy, 10 males (43 %). The mean age at the time of the recorded visit was 47 ± 17 years. Paralysis affected the right side in 13 patients (57 %). The etiology was postoperative in 10 patients (44 %), posttraumatic in one patient (4 %), Bell’s palsy in 11 patients (48 %), and Ramsay-Hunt syndrome in one patient (4 %).
To test the measurement properties of the scale, a total of 6,902 items were assessed. Figure 4 and Electronic supplementary material summarize the composite SFGS scores for the 29 videos of patients that were rated twice by the six operators. The Italian version of the scale showed an excellent internal consistency, rated by a Cronbach’s α value of 0.91 [lower limit (CI) at 95 %: 0.81], for all the items from the first observation of the 29 videos.
The SFGS composite score for 29 videos rated twice by 6 physicians using the Italian version of the scale. The SFGS composite score given by 6 independent operators during their first (white) and second (gray) evaluation of each video (1 → 29) of facial palsy patients are represented. The vertical line denotes median value, the box represents the upper and lower quartiles, and the horizontal bars indicate minimum and maximum value
Table 1 shows the correlation values between the operators evaluating 29 videos of patients with facial palsy. During the first observation of the videos, the correlation between the composite scores given by the six operators was almost perfect, in accordance with Landis and Koch [13], with an ICC value of 0.96 (95 % CI 0.93–0.98). The CR mean of all the operators was 12.5 (min. 5.5, max. 26.0).
The correlation between the three experienced operators was very high, with ICC values of 0.95 (95 % CI 0.92–0.98) and CR mean of 7.2 (min. 6.5, max. 8.1). The same was true for the two novice operators, with ICC of 0.99 (95 % CI 0.98–1) and CR of 7.3. No differences emerged in term of ICC with the expert operator between experienced and novice raters (t test, p = 0.11).
Table 2 shows the correlation between the scores for individual items given by the six operators evaluating 29 videos of patients with facial palsy. The correlation between operators was excellent for their assessment of the symmetry of voluntary movement (ICC 0.96, 95 % CI 0.93–0.98), symmetry at rest (ICC 0.89, 95 % CI 0.84–0.95) and synkinesis (ICC 0.89, 95 % CI 0.84–0.95), although it was significantly higher for their assessment of symmetry of voluntary movement than it was for the other two areas (Kruskal–Wallis test, p = 0.02). In all three areas of assessment (symmetry of voluntary movement, symmetry at rest, synkinesis), the composite score showed a higher correlation than the assessment of each individual area, due to compensation of individual items. The item with the lowest inter-operator correlation was synkinesis with activation of the frontal muscle, with ICC 0.58 (95 % CI 0.42–0.74).
During the second observation of the 29 videos of facial palsy patients, the correlation between operators improved, with an ICC of the composite score between all operators of 0.98 (95 % CI 0.97–0.99). Correlation improved during the second observation for 11 of the 17 items.
The repeatability for the assessment of the composite score of facial palsy patients was high for all operators, and comparable for expert, experienced and novice operators: mean ICC 0.98 (range 0.97–0.98), mean CR 9.93 (range 9.02–10.89), approximately 1/10 of the range 0–100 of the scale. Repeatability was excellent for the six operators in the three assessment areas: symmetry at rest (average ICC 0.85, range 0.78–0.90), symmetry of voluntary movement (mean ICC 0.98, range 0.97–0.99), and synkinesis (mean ICC 0.9, range 0.8–0.96).
The grading of the 29 videos of healthy subjects, similar in gender and age to the patients, was employed only to assess the content of validity of the scale. The two raters showed almost perfect correlation and performed an identical evaluation of 19 on 29 videos. All the 29 healthy controls had a SFGS composite score ranging from 90 to 100 and in 18 on 29 individuals (62 %), 100 was scored. The difference between the scores of healthy and affected individuals was highly significant (t test p < 0.0001).
Discussion
The Italian version of the scale and its explanatory criteria was shown to be faithful to the original, and the minor linguistic adjustments made the scale quick and simple to use for the native Italian speaking physicians in our study.
To test the measurement properties of the scale, we used a series of patients who had a wide range of facial paralyses that were difficult to assess. As shown in Fig. 4 and Electronic supplementary material, the majority of patients had indeed a clinical picture of intermediate severity, and in 22 of the 29 videos (76 %), the patients had synkinesis. These are well-known causes of high variability in the assessment scores given when using the SFGS [9, 13].
The Italian version of the SFGS showed excellent internal consistency and an almost perfect inter- and intra-observer correlation, in line with values for the original version reported in the literature [5, 6, 9, 14–16].
In our study, in agreement with Kanerva et al. [9] but not with Neely et al. [5], the assessment of symmetry of voluntary movement showed a statistically higher correlation than the assessment of symmetry at rest and synkinesis, probably due to the ability of physiatrists to assess muscle contraction.
The most difficult item to assess proved to be the presence of synkinesis during the activation of the frontal muscles, in agreement with Kayhan et al. [7]. Our study demonstrates that the Italian version of SFGS could discriminate well between patients with facial palsy and healthy controls. The excellent reproducibility of the Italian version of the scale, combined with the inherent properties of the original version that have been already highlighted, such as sensitivity to clinical changes [6], and good correlation with other grading systems in use [8–10, 17], make this an ideal scale to use when monitoring the clinical course of facial palsy, and encourage its use by native Italian speakers. Furthermore, Kanerva et al. [17] have recently published a conversion table for SFGS and House-Brackmann scale, the latter being a traditional scoring system of wide clinical use. The availability of this conversion system will therefore facilitate the performance of meta-analysis including studies using either systems. The accurate definition of the severity of post-paralytic synkinesis in all facial areas also makes the SFGS an ideal tool to monitor the clinical course of facial palsy during the treatment of these sequelae [18].
Hu et al. [16] reported that novice doctors are able to use the SFGS correctly, and recently Neely et al. [5] demonstrated that the explanatory criteria of the scale facilitate novice doctors when they use the scale. In line with this finding, our study confirms that after a brief training session and with the help of the explanatory criteria, novice physicians are able to assess facial palsy correctly.
Conclusions
Our study uses an independent clinical series of patients with various etiology and severity of facial palsy to demonstrate that the Italian version of SFGS has the same measurement properties as the original scale, including excellent internal consistency and reproducibility. The success of our study should encourage the translation of this scale into other languages. To our knowledge, the SFGS is the first facial palsy scale to be validated in Italian. We hope this will encourage the Italian speaking scientific community to use the SFGS.
References
Gilden DH (2004) Clinical practice. Bell’s Palsy. N Engl J Med 351:1323–1331
de Swart BJ, Verheij JC, Beurskens CH (2003) Problems with eating and drinking in patients with unilateral peripheral facial paralysis. Dysphagia 18:267–273
Peitersen E (2002) Bell’s palsy: the spontaneous course of 2,500 peripheral facial nerve palsies of different etiologies. Acta Otolaryngol Suppl 549:4–30
Chee GH, Nedzelski JM (2000) Facial nerve grading systems. Facial Plast Surg 16:315–324
Neely JG, Cherian NG, Dickerson CB, Nedzelski JM (2010) Sunnybrook facial grading system: reliability and criteria for grading. Laryngoscope 120:1038–1045
Ross BG, Fradet G, Nedzelski JM (1996) Development of a sensitive clinical facial grading system. Otolaryngol Head Neck Surg 114:380–386
Kayhan FT, Zurakowski D, Rauch SD (2000) Toronto facial grading system: interobserver reliability. Otolaryngol Head Neck Surg 122:212–215
Berg T, Jonsson L, Engström M (2004) Agreement between the Sunnybrook, House-Brackmann, and Yanagihara facial nerve grading systems in Bell’s palsy. Otol Neurotol 25:1020–1026
Kanerva M, Poussa T, Pitkäranta A (2006) Sunnybrook and House-Brackmann facial grading systems: intrarater repeatability and interrater agreement. Otolaryngol Head Neck Surg 135:865–871
Coulson SE, Croxson GR, Adams RD, O’Dwyer NJ (2005) Reliability of the “Sydney,” “Sunnybrook,” and “House Brackmann” facial grading systems to assess voluntary movement and synkinesis after facial nerve paralysis. Otolaryngol Head Neck Surg 132:543–549
Guillemin F, Bombardier C, Beaton D (1993) Cross-cultural adaptation of health-related quality of life measures: literature review and proposed guidelines. J Clin Epidemiol 46:1417–1432
Altman DG, Bland JM (1983) Measurement in medicine: the analysis of method comparison studies. Statistician 32:307–317
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Ross BG, Nedzelski JM (1997) Reliability and validity of the Sunnybrook facial grading system. In: Yanagihara N, Muratami S (eds) New horizons in facial nerve research and facial expression: 8th international symposium on the facial nerve. Kugler Publications, Hague, pp 563–567
Ahrens A, Skarada D, Wallace M, Cheung JY, Neely JG (1999) Rapid simultaneous comparison system for subjective grading scales grading scales for facial paralysis. Am J Otol 20:667–671
Hu WL, Ross B, Nedzelski J (2001) Reliability of the Sunnybrook facial grading system by novice users. J Otolaryngol 30:208–211
Kanerva M, Jonsson L, Berg T, Axelsson S, Stjernquist-Desatnik A, Engström M, Pitkäranta A (2011) Sunnybrook and House-Brackmann systems in 5397 facial gradings. Otolaryngol Head Neck Surg 144:570–574
Dalla Toffola E, Furini F, Redaelli C, Prestifilippo E, Bejor M (2010) Evaluation and treatment of synkinesis with botulinum toxin following facial nerve palsy. Disabil Rehabil 32:1414–1418
Acknowledgments
We thank Charlotte Buckmaster for her linguistic expertise. C. Pavese is partially supported by an investigator fellowship from Collegio Ghislieri, Pavia, Italy.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Online Resource: The SFGS scores for 29 videos rated by 6 physicians using the Italian version of the scale.
Rights and permissions
About this article
Cite this article
Pavese, C., Tinelli, C., Furini, F. et al. Validation of the Italian version of the Sunnybrook Facial Grading System. Neurol Sci 34, 457–463 (2013). https://doi.org/10.1007/s10072-012-1025-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-012-1025-x