Abstract
Multiple sclerosis (MS) is a chronic inflammatory and degenerative disease of the central nervous system. In the last decade, pathological and magnetic resonance imaging (MRI) studies have shown that a significant portion of inflammatory lesions are located in the grey matter, especially in the cerebral cortex, of MS patients. Cortical inflammatory lesions (CL) can be demonstrated in vivo in MS patients by double inversion recovery (DIR) MRI sequence. Neuropsychological deficits constitute a major clinical aspect of MS, being demonstrated in a percentage ranging from 40 to 65% of patients, and have been shown to be associated with cortical demyelination and atrophy. Recent DIR studies in MS patients having different clinical forms of the disease have disclosed that CL burden not only correlates with the severity of physical disability, but is also one of the major structural changes associated with disease-related cognitive impairment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since the extraordinarily telling remark on the cognitive impairment observed in multiple sclerosis (MS) patients made by Charcot, i.e., “In most of the patients affected by multi-locular sclerosis […] there is a marked enfeeblement of the memory; conceptions are formed slowly; the intellectual and emotional faculties are blunted in their totality” (Charcot 1877), the presence of various degrees of cognitive dysfunctions has been largely documented in MS. Cognitive deficits may affect from 40 to 65% of MS patients, and significantly contribute to their disability [1, 2]. Indeed, cognitive dysfunction disrupts lives, lifestyles, employment status, and yearly earnings of MS patients, has detrimental effects on personal, occupational, and social functioning, thereby affecting overall quality of life. Although more frequent and severe in the progressive forms of MS, a cognitive impairment can be present since the early stages of the disease [1, 2]. MS affects various aspects of cognitive functioning, including attention and concentration, information processing efficiency, executive functions, processing speed, and long-term memory. Processing speed, visual learning and memory seem to be the most commonly affected in MS. Overt dementia is rare in MS, and the more common clinical presentation is one of specific and subtle cognitive deficits that can vary substantially among patients [1, 2].
Magnetic resonance imaging (MRI) has been largely applied to investigate the radiological abnormalities associated with cognitive dysfunction in MS [1, 3]. Although the decline in cognitive performance was ascribed to white matter (WM) and subcortical pathology, the strength of the relationship between WM lesion load and cognitive impairment was modest. Moreover, brain atrophy measures were found to correlate only moderately with MS-related cognitive impairment [4–6]. Other MRI studies, aimed at evaluating the extent of brain tissue loss on a regional basis, have disclosed that neocortical volume loss was more closely associated with cognitive decline than whole-brain atrophy [7, 8].
The cortical involvement in MS is probably a quite complex and heterogeneous phenomenon since it may result from several pathological processes, like meningeal inflammation, neuronal injury, Wallerian or transsynaptic degeneration, and overall from local demyelinating lesions [9, 10]. Indeed, MS is characterized by an extensive cortical inflammation, with a relevant number of focal lesions (cortical lesions, CL) located within the cerebral cortex of patients [9–11]. In the past few years, a large effort was devoted to the development of MRI techniques capable of visualizing at least a portion of CL in vivo. Recently, the application of double inversion recovery (DIR) sequences convincingly demonstrated that CL are a frequent finding in patients with MS [12, 13]. DIR imaging allowed an average increase of 152% in CL detection per patient when compared with FLAIR. Moreover, in comparison with T2-weighted sequences, DIR showed a 500% increase in detection of CL [14]. In previous studies on large cohorts of MS patients, we found that CL could be demonstrated in the early disease stages [12], were associated with critical symptoms, such as epilepsy [15], were inversely correlated with the “benign” course of the disease [16] and could be detected at clinical onset in MS patients having no lesions in the WM, as disclosed by conventional MRI sequences [17]. Moreover, CL were found to correlate with cortical atrophy in primary progressive MS [18], and to play an important role in determining the clinical course of the disease [19]. The hypothesis that CL could be also an additional pathological substrate for MS-related cognitive dysfunction remained to be proved.
CL as a substrate of cognitive dysfunction in MS
Roosendaal and colleagues [20] demonstrated that CL, detected by DIR imaging, might have a significant impact on MS-related cognitive decline. Using the Letter Digit Substitution Test to assess processing speed of visual information and the Location Learning Test (LLT) to evaluate visuospatial memory, their study showed, in 13 MS patients, that CL increased significantly over a time period of 3 years and were associated with a worse performance on neuropsychological measures at follow-up. More specifically, they observed a significant relationship at follow-up between hippocampal lesion number and the LLT delay score, which could be understood in terms of the heavy involvement of the hippocampus in visuospatial memory. Main limitations of the study were the relatively low number of subjects and the use of a cognitive test battery limited to only two cognitive domains.
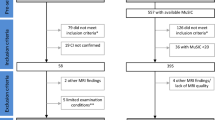
In a different way, we quantified the extent of CL detectable on DIR images in 70 patients affected from relapsing–remitting MS (RRMS), in order to improve our understanding of their relative contribution to disease-related cognitive impairment [21]. Furthermore, in our study, neuropsychological assessment was performed using the Rao Brief Repeatable Battery of Neuropsychological Tests, that includes tests of verbal immediate and delayed recall memory [Selective Reminding Test (SRT) and SRT-Delayed Recall], spatial immediate and delayed recall memory (10/36 Spatial Recall Test and 10/36 Spatial Recall Test-Delayed), sustained attention, concentration, and speed of information processing (Paced Auditory Serial Addition Test at 3 s and Symbol Digit Modalities Test), and verbal fluency on semantic stimulus (Word List Generation). Twenty-four patients (34.3%) were classified as cognitively impaired [i.e, they scored 2 standard deviations (SDs) below the mean normative values in ≥1 cognitive test] and 46 patients (65.7%) were classified as cognitively unimpaired. T2 hyperintense WM lesion volume and contrast-enhancing lesion number were not different between cognitively impaired and cognitively unimpaired patients. CL were detected in 18 of 24 cognitively impaired patients (75.0%) (see Fig. 1) and 44 of 46 cognitively unimpaired patients (95.7%) (P = 0.01), but cognitively impaired patients had a significantly higher CL volume (P < 0.001). The best correlation was found between CL load (number and volume) and tests for sustained attention (SDMT, PASAT-3), test for speed of information processing (PASAT-3), and global cognitive impairment. A multivariate analysis revealed significant contributions from CL volume and, at a lower level, age and grey matter (GM) atrophy as independent predictors of cognitive impairment. Finally, we observed that RRMS patients with cognitive deficits had higher CL load and cortical atrophy than those having normal cognitive performance. The multivariate analysis further revealed that only CL volume and neocortical volume loss were independent predictors of cognitive decline in these patients.
Our results are in agreement with previous pathological [22] and neuroimaging [7] studies, which demonstrated a significant cortical pathology in cognitively impaired RRMS patients. Considering the conflicting observations on the role played by subcortical WM damage in determining the cognitive decline in MS, our data further strengthen the notion that the overall burden of WM lesions does not fully account for the severity of cognitive impairment in MS and indicate the CL burden as one of the major structural changes associated to MS-related cognitive dysfunction.
References
Amato MP, Zipoli V, Portaccio E (2006) Multiple sclerosis-related cognitive changes: a review of cross-sectional and longitudinal studies. J Neurol Sci 245(1–2):41–46
Chiaravalloti ND, DeLuca J (2008) Cognitive impairment in multiple sclerosis. Lancet Neurol 7(12):1139–1151
Rovaris M, Comi G, Filippi M (2006) MRI markers of destructive pathology in multiple sclerosis-related cognitive dysfunction. J Neurol Sci 245(1–2):111–116
Zivadinov R, Sepcic J, Nasuelli D et al (2001) A longitudinal study of brain atrophy and cognitive disturbances in the early phase of relapsing–remitting multiple sclerosis. J Neurol Neurosurg Psychiatry 70(6):773–780
Sanfilipo MP, Benedict RH, Weinstock-Guttman B, Bakshi R (2006) Gray and white matter brain atrophy and neuropsychological impairment in multiple sclerosis. Neurology 66(5):685–692
Sanchez MP, Nieto A, Barroso J, Martin V, Hernandez MA (2008) Brain atrophy as a marker of cognitive impairment in mildly disabling relapsing–remitting multiple sclerosis. Eur J Neurol 15(10):1091–1099
Amato MP, Bartolozzi ML, Zipoli V et al (2004) Neocortical volume decrease in relapsing remitting MS patients with mild cognitive impairment. Neurology 63(1):89–93
Morgen K, Sammer G, Courtney SM et al (2006) Evidence for a direct association between cortical atrophy and cognitive impairment in relapsing–remitting MS. Neuroimage 30(3):891–898
Peterson JW, Bö L, Mörk S et al (2001) Transected neurites, apoptotic neurons, and reduced inflammation in cortical multiple sclerosis lesions. Ann Neurol 50:389–400
Bø L, Vedeler CA, Nyland H et al (2003) Subpial demyelination in the cerebral cortex of multiple sclerosis patients. J Neuropathol Exp Neurol 62:723–732
Kidd D, Barkhof F, McConnell R et al (1999) Cortical lesions in multiple sclerosis. Brain 122:17–26
Calabrese M, De Stefano N, Atzori M et al (2007) Detection of cortical inflammatory lesions by double inversion recovery magnetic resonance imaging in patients with multiple sclerosis. Arch Neurol 64(10):1416–1422
Calabrese M, Filippi M, Rovaris M et al (2008) Morphology and evolution of cortical lesions in multiple sclerosis: a longitudinal MRI study. Neuroimage 42(4):1324–1328
Geurts JJ, Pouwels PJ, Uitdehaag BM et al (2005) Intracortical lesions in multiple sclerosis: improved detection with 3D double inversion-recovery MR imaging. Radiology 236:254–260
Calabrese M, De Stefano N, Atzori M et al (2008) Extensive cortical inflammation is associated with epilepsy in multiple sclerosis. J Neurol 255:581–586
Calabrese M, Filippi M, Rovaris M et al (2009) Evidence for relative cortical sparing in benign multiple sclerosis: a longitudinal magnetic resonance imaging study. Mult Scler 15:36–41
Calabrese M, Gallo P (2009) Magnetic resonance evidence of cortical onset of multiple sclerosis. Mult Scler 15:933–941
Calabrese M, Rocca MA, Atzori M et al (2009) Cortical lesions in primary progressive multiple sclerosis: a 2-year longitudinal MR study. Neurology 72:1330–1336
Calabrese M, Rocca MA, Atzori M et al (2010) A three-year MRI study of cortical lesions in relapse-onset multiple sclerosis. Ann Neurol (in press)
Roosendaal SD, Moraal B, Pouwels PJ et al (2009) Accumulation of cortical lesions in MS: relation with cognitive impairment. Mult Scler 15(6):708–714
Calabrese M, Agosta F, Rinaldi F et al (2009) Cortical lesions and atrophy associated with cognitive impairment in relapsing–remitting multiple sclerosis. Arch Neurol 66:1144–1150
Geurts JJ, Barkhof F (2008) Grey matter pathology in multiple sclerosis. Lancet Neurol 7(9):841–851
Conflict of interest statement
The authors declare that they have no conflict of interest related to the publication of this article.
Author information
Authors and Affiliations
Corresponding author
Additional information
F. Rinaldi and M. Calabrese have equally contributed to the work.
Rights and permissions
About this article
Cite this article
Rinaldi, F., Calabrese, M., Grossi, P. et al. Cortical lesions and cognitive impairment in multiple sclerosis. Neurol Sci 31 (Suppl 2), 235–237 (2010). https://doi.org/10.1007/s10072-010-0368-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-010-0368-4