Abstract
Chronic daily headache (CDH) is one of the more frequently observed headache syndromes at major tertiary care centers. CDH is defined as headache occurring >15 days/month. Different mechanisms are involved in the development of CDH but what factors specifically contributing to the transformation from episodic into CDH remain largely unknown. Analgesic overuse is commonly identified as the most important factor for such transformation. Hypertension, allergy, asthma, arthritis, diabetes, obesity and hypothyroidism were associated with CDH in clinical series. The objective of this study is to identify risk factors of chronicity in patients with headache. A total of 1,483 consecutive patients were studied. We collected information on age, gender, headache type and comorbidity. Patients were divided into three diagnostic groups: migraine and tension-type headache (CTT) diagnosis were made according to ICHD-II, and CDH fulfilling the Proposal Headache Classification for Chronic Daily Headache described by Silberstein and Lipton (in Chronic daily headache including transformed migraine, chronic tension-type headache, and medication overuse, 2001). We used descriptive statistics and Chi-square test. Our data show that age, gender and headache onset were similar in the three groups. Diabetes, hypercolesterolaemia, smoke and cardiopathy prevalence did not differ in the three groups (P > 0.05). Hypertension prevalence in CDH group (16.2%) was significantly higher than in the other two groups (migraine 7.3%; CTT 6.6%; P < 0.01). There were no differences (P > 0.05) in hypertension prevalence between CDH with and without medication overuse. CDH patients (mean age 41.8 ± 14) referred to the Headache Center later than migraine and CTT patients (mean age 37 ± 12) (P > 0.05). According to previous studies we found that hypertension is more frequent in CDH than in migraine and CTT. Examining this result it is possible to conclude that there exists an association between CDH and hypertension, but not that a causal relationship necessarily exists. Considering the other somatic conditions we did not find any correlation. The potential role of somatic comorbidity in CDH has to be studied in further clinical trials.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Chronic daily headache (CDH) is defined as headache occurring >15 days/month, for >3 months. Transformation from episodic migraine into CDH is often gradual and reversible with possible spontaneous or induced remission [1, 2]. CDH happens in some but not most individuals; patients are dramatically impaired in their ability to function and in their quality of life [3]. Therefore, identification of factors that predict the change from episodic to chronic migraine is very important because they provide insights into the different mechanisms involved in the development of CDH. However, what factors specifically contribute to the transformation from episodic into CDH remain largely unknown. On the basis of several previous studies, risk factors for migraine chronification have been divided into three categories: non-modifiable (age, female sex, white race, low educational level, socioeconomic status and genetic factors), modifiable (attack frequency, obesity, medication overuse, psychiatric comorbidities, stressful life events and snoring) and putative (allodynia, pro-inflammatory states and prothrombotic states) [2]. Analgesic overuse is commonly identified as the most important factor for such transformation. Hypertension, allergy, asthma, arthritis, diabetes, obesity and hypothyroidism have been reported to be associated with CDH in clinical series [4]. A number of small case–control studies reported contradictory results concerning the relationship between migraine and hypertension. The largest population-based longitudinal study [5] did not find association between migraine and hypertension.
On this basis, the aim of this study is to identify possible risk factors to the development of chronic headache.
Methods
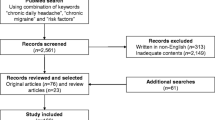
1,483 consecutive patients referred to our Headache Centre were studied. Patients were divided into three diagnostic groups: migraine (1,120 pts) and tension-type headache (CTT) (166 pts) (according to ICHD-II) [6], and CDH (daily or near-daily headache lasting more than 4 h if not treated, occurring more than 15 days/month) (197 pts) fulfilling the Proposal Headache Classification for Chronic Daily Headache described by Silberstein and Lipton [7]. A neurological examination was assessed to all patients. For all patients we collected information about age, gender, headache type and frequency (using headache diary), and comorbidity (cardiovascular disease, hypertension, diabetes, hypercholesterolaemia, smoke, and oral contraceptive therapy). Patients were considered affected by hypertension if there were a clinical diagnosis and an adequate therapy.
Statistical analysis was performed using descriptive statistics and Chi-square test.
Results
There are no significant differences concerning age, education and headache family history between the three groups (P > 0.05). Headache onset is also similar in the three groups (P > 0.05). Females/males ratio is higher in CDH (F:M = 4:1) than in migraine and CTT groups (F:M = 3:1). CDH patients (mean age 41.8 ± 14) referred to the Headache Centre later than migraine and CTT patients (mean age 37 ± 12) (P > 0.05). Diabetes, hypercolesterolaemia, smoke, oral contraceptive therapy and cardiac disease prevalence did not differ in the three groups (P > 0.05).
We observed that hypertension prevalence in CDH group (16.2%) is significantly higher than in the other two groups (migraine 7.3%, CTT 6.6%, P < 0.01). No statistical differences (P > 0.05) in hypertension prevalence were found between migraine and CTT patients and also between CDH with and without medication overuse (Table 1).
Discussion
Our study shows that hypertension is more frequent in CDH than in migraine and CTT. Examining this result it is possible to conclude that there is an association between CDH and hypertension, but not that a causal relationship necessarily exists. Indeed, the assessment of the migraine patient may include an evaluation of risk factors for progression. The explanation for an increased prevalence of hypertension in CDH patients remains unclear. Vascular endothelial damage or dysfunction, genetic predisposition, or medication overuse might be factors involved in the pathogenesis of CDH. However, a causal role of drug overuse on the development of hypertension in CDH patients has been excluded because there is no significant difference between CDH patients with and without overuse.
Considering the other somatic conditions, in contrast with some previous studies, we did not find any correlation. The potential role of somatic comorbidity in CDH has to be studied in further clinical trials.
References
Stovner LJ, Zwart JA, Hagen K, Terwindt GM, Pascual J (2006) Epidemiology of headache in Europe. Eur J Neurol 13:333–345
Bigal ME, Lipton RB (2008) Clinical course in migraine: conceptualizing migraine transformation. Neurology 71:848–855
Bigal ME, Rapaport AM, Lipton RB et al (2003) Assessment of migraine disability using the migraine disability assessment (MIDAS) questionnaire: a comparison of chronic migraine with apisodic migraine. Headache 43:336–342
Bigal ME, Sheftell FD, Rapaport AM, Tepper SJ, Lipton RB (2002) Chronic daily headache: identification of factors associated with induction and transformation. Headache 42:575–581
Gudmundsson LS, Thorgeirsson G, Sigfusson N, Sigvaldason H, Johannsson M (2006) Migraine patients have lower ssystolic but higher diastolic blood pressure compared with controls in a population-based study of 21,537 subjects. The Reykjavik Study. Cephalalgia 26:436–444
Headache Classification Subcommittee of the International Headache Society (2004) The International Classification of Headache Disorders, 2nd edn. Cephalalgia 24(Suppl 1):1–160
Silberstein SD, Lipton RB (2001) Chronic daily headache including transformed migraine, chronic tension-type headache, and medication overuse. In: Wolff’s headache and other head pain. Oxford University Press, USA, pp 247–282
Conflict of interest statement
The authors declare that they have no conflict of interest related to the publication of this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gipponi, S., Venturelli, E., Rao, R. et al. Hypertension is a factor associated with chronic daily headache. Neurol Sci 31 (Suppl 1), 171–173 (2010). https://doi.org/10.1007/s10072-010-0322-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-010-0322-5