Abstract
Objective
To assess incidence, time-trends, and outcomes of serious infections in people with polymyalgia rheumatica (PMR) or giant cell arteritis (GCA).
Methods
We examined the 1998–2016 US National Inpatient Sample for serious infections in PMR or GCA, namely, opportunistic infections (OI), skin and soft tissue infections (SSTI), urinary tract infection (UTI), pneumonia, and sepsis/bacteremia. Multivariable-adjusted logistic regressions assessed association of the type of infection, demographics, comorbidity, and hospital characteristics with healthcare utilization and mortality.
Results
Hospitalized with serious infections, those with PMR or GCA were 2 decades older than people without PMR or GCA, and more likely to be female or white or have higher Deyo-Charlson index score or higher income. Sepsis rates in the general population, PMR, and GCA cohorts were 10.2%, 17.7%, and 18.9% in 2015–2016, respectively. Incidence rates of serious infections/100,000 NIS claims in PMR and GCA in 2015–2016 were as follows (rounded off): OI, < 1 and < 1; SSTI, 4 and 1; UTI, 4 and 1; pneumonia, 9 and 2; and sepsis, 20 and 4, respectively. Sepsis surpassed pneumonia as the most common serious infection in 2011–2012. In multivariable-adjusted analyses in the PMR cohort, sepsis, female sex, Deyo-Charlson comorbidity score ≥ 2, Medicare or Medicaid insurance, urban hospital location, and large hospital bed size were associated with significantly higher healthcare utilization and/or in-hospital mortality. Similar associations were noted in the GCA cohort.
Conclusions
Incidence of serious infections, especially sepsis, increased in both PMR and GCA cohorts over time. Interventions to improve serious infection outcomes in PMR/GCA are needed.
Key Points • PMR/GCA patients with hospitalized serious infections were 2 decades older than the general population. • Sepsis surpassed pneumonia as the commonest hospitalized serious infection in PMR/GCA in 2011–2012. • Sepsis, female sex, comorbidity, Medicare/Medicaid insurance, and urban location were associated with higher healthcare utilization and in-hospital mortality. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Giant cell arteritis (GCA) is the most frequent type of vasculitis in adults [1]. GCA is a vasculitis of large and medium-sized vessels that presents most commonly with headache and/or visual symptoms [2]. Polymyalgia rheumatica (PMR) is a condition affecting the elderly, characterized by proximal muscle pain and stiffness, and systemic inflammation [3, 4]. GCA and PMR are often concurrent and overlapping conditions [5,6,7]. Most studies of infections in GCA and PMR examined their role in disease etiology [8,9,10], rather than disease-related or a treatment complication. Glucocorticoids are the mainstay of therapy for GCA [11] and PMR [5], which have been long-recognized as risk factors for infections and serious infections [12,13,14]. Therefore, studies of infections in GCA and PMR are needed.
Three population-based studies of incidence of infections in GCA demonstrated contradictory results. A study of The UK Health Improvement Research Network (THIN) data, a population-representative study of 300 practices, showed that the people with GCA had an increased rate of infections compared to the general population [15], especially in the first 6 months of the treatment. At a mean follow-up of 5 years, 48% patients with GCA versus 37% patients without GCA had at least 1 episode of systemic infection [15]. A French population based study of 486 patients with GCA and age- and sex-matched general population controls of 5-year follow-up reported a significantly higher incidence of severe infections in GCA versus non-GCA during the first year after diagnosis, 11.1/100 patient-years versus 5.9/100 patient-years [16], with an incidence rate ratio of 2-fold higher. In contrast, in a population-based US study of Olmsted County cohort of 245 GCA patients and 245 age-, sex-, and calendar-year-matched cohort without GCA, the incidence rates of hospitalized infections were similar, 5.6/100 person-years in GCA (74 people; 134 episodes) and 6.0/100 person-years in non-GCA (79 people; 153 episodes); the rates of pneumonia, UTI, and skin and soft tissue infections were not significantly different between GCA and non-GCA cohorts [17]. Thus, the evidence to-date is contradictory with some studies indicating higher infection risk in GCA, but not other studies. Therefore, a better understanding of infection risk in GCA is needed. No studies have been published for PMR, another condition where chronic glucocorticoid therapy is frequently used, and serious infection risk may be increased.
Our specific aim was to study the incidence of serious/hospitalized infections in GCA and PMR in a national US sample, time-trends over 2 decades, and predictors of associated healthcare utilization and mortality. Our study objectives were to: [1] provide the national US estimates of serious infections, and rates of specific serious infections in people with GCA or PMR; [2] examine the time-trends in serious infections over 2 decades; and [3] explore the factors associated with healthcare utilization and mortality associated with serious infections in people with GCA or PMR.
Methods
Data source
We analyzed the US National Inpatient Sample (NIS) data from 1998 to 2014. The NIS represents a 20% stratified sample of discharges for the USA, which allows estimation of the US national estimates of hospital inpatient stays and key healthcare utilization outcomes. The NIS has data from more than 7 million US hospitalizations each year (unweighted), which estimates more than 35 million hospitalizations nationally (weighted) [18]. NIS data, that are a part of the healthcare cost and utilization project (HCUP), are publicly available from the Agency for Healthcare Research and Quality’s (AHRQ). Recently, a slight change in the design of the NIS made it a sample of discharge records from all HCUP-participating hospitals; in the prior years, it was a sample of hospitals [19]. The NIS provides new weights to account for the design change.
Ethics statement
The University of Alabama at Birmingham’s Institutional Review Board (IRB) approved the study (X120207004). All investigations were conducted in conformity with ethical principles of research. The IRB waived the need for an informed consent for this database study.
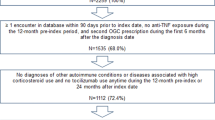
Inclusion and exclusion criteria
The study cohort included people hospitalized with versus without an International Classification of Diseases, ninth or tenth revision, clinical modification (ICD-9-CM or ICD-10-CM) code for serious infection (primary diagnosis) among people with PMR (725 or M35.3) or GCA (446.5, M31.5, M31.6), in any position other than the primary diagnosis position during index hospitalization. A previous database study showed sensitivity of 93% and specificity of 95% for PMR diagnosis and 93% sensitivity and 95% specificity for vasculitis diagnoses using this approach [20].
Serious infections of interest and covariates
Among people with GCA or PMR, we identified five common serious infections by their listing as the primary diagnosis for hospitalization using ICD-9-CM codes: (1) opportunistic infections (OI, 010.xx − 018.xx, 031.xx, 078.5, 075.xx, 053.xx, 112.4, 112.5, 112.81, 112.83, 130.xx, 136.3, 117.5, 027.0, 039.xx, 117.3, 114.xx, 115.xx, 116.0); (2) skin and soft tissue infections (SSTI; 040.0, 569.61, 681.xx, 682.xx, 785.4, 728.86, and 035.xx); (3) urinary tract infection (UTI; 590.xx); (4) pneumonia (003.22, 481.0, 513.0, 480.xx, 482.xx, 483.xx, 485.xx, and 486.xx); and (5) sepsis/bacteremia (sepsis; 038.xx and 790.7), as previously [21, 22]. These codes for infections were valid in administrative datasets, with positive predictive values of 70–100% in people with rheumatoid arthritis [23,24,25]. We also used the ICD-10-CM codes for infections for the 2015–2016 data since the coding system changed from the ICD-9-CM to ICD-10-CM in 2015 in the U.S. (Appendix 1).
We examined several important covariates and potential confounders including demographics (age, gender, race/ethnicity, income), comorbidity, insurance type, and hospital characteristics. We categorized household income, based on patient’s zip code, into 4 quartile ranging from the lowest (poorest) to the highest quartile (wealthiest), based on the thresholds for each quartile provided by the NIS that varied each year [26]. Comorbidity was assessed by the Deyo-Charlson index, a valid measure consisting of 17 medical comorbidities (myocardial infarction, heart failure, cerebrovascular disease, dementia, renal disease, liver disease, chronic pulmonary disease, diabetes, etc.), based on the presence of ICD-9-CM codes at index admission [27]. It was categorized as none, one or two, or above. We assessed insurance payer type and categorized it as Medicaid (coverage for the low income and disabled Americans), Medicare (healthcare coverage for Americans 65 years or older), private insurance, and self/other [28], as previously [29]. Hospitals were categorized based on location and teaching status as rural, urban nonteaching or urban teaching hospital, region (Northeast, Midwest, South, West), and bed size (small, medium, large), which are standard NIS variables.
Healthcare utilization outcomes and in-hospital mortality
We examined healthcare utilization outcomes and in-hospital mortality. Utilization outcomes included the total hospital charges (NIS variable, TOTALCHG), the length of hospital stay (NIS variable, LOS; median, 3 days), both categorized as above/below the median, and the proportion discharged to home versus a non-home setting, i.e., short-term hospital, skilled nursing facility, intermediate care facility etc. (NIS variable, DISPUNIFORM).
Statistical analysis
We compared demographics of serious infections in 2 cohorts of people, those with versus without PMR and similarly for GCA separate analyses. Rates and time-trends for each serious infection were calculated per 100,000 hospitalization claims in the PMR or GCA cohort. Rates of and time-trends in serious infections in PMR or GCA were also calculated per 100,000 NIS claims. Rates of the five infections (/100,000 NIS claims) were each analyzed for trends over time using Cochran Armitage test. All other analyses were limited to serious infections in people with PMR or GCA. We assessed patient characteristics of hospitalizations for each of the five serious infections in PMR or GCA. We used adjusted logistic regression models for total hospital charges above the median, the length of hospital stay > 3 days (median), discharge to non-home setting, and in-hospital mortality. We calculated odds ratios (OR) and 95% confidence intervals (CI).
Results
Cohort characteristics
Among people with serious infections, those with PMR or GCA were 2 decades older than their counter-parts without PMR or GCA, more likely to be female, white, have higher Deyo-Charlson index score, and higher income (Table 1). Mean age of non-PMR and non-GCA cohorts was 60 years, PMR was 80 years and GCA, 79 years. Unadjusted rate of discharge to home was lower, and the length of hospital stay was longer in those with PMR or GCA admitted with serious infections, compared with people without PMR of GCA (Table 1). In-hospital mortality rates were similar 6.2% in general population versus 5.7% in PMR versus 7% in GCA.
In people with PMR, pneumonia (n = 72,723; 44%), sepsis (n = 56,426; 35%), and skin and soft tissue infections (SSTI; n = 23,134; 12%) were the most common serious infections following by UTI (n = 6604; 4%) and opportunistic infections (OI; n = 3244; 2%; Table 2). The order, numbers, and proportions were similar in people with GCA (Table 2).
Detailed characteristics of people with PMR (Table 2) and GCA (Table 3) with each infection of interest are shown. Three-quarter of people with each infection of interest in PMR or GCA groups had a Deyo-Charlson index score of 2 or higher. Unadjusted mortality ranged from 0.7 to 11%; the length of hospital stay ranged from 2.9 days for UTI to 4.6 days for opportunistic infection; and the total hospital charges ranged from $30,398 for UTI to $76,160 for OI (Tables 2 and 3).
Annual rates of serious infections: PMR versus GCA versus general population
Unadjusted frequency (Appendix 1) and rates of serious infections (Table 4) were higher in PMR and GCA cohorts compared with the general population cohort. Overall, the incidence of serious infections increased in both PMR and GCA cohorts over time (Table 4). Among respective hospitalizations, sepsis rates in the general population, PMR, and GCA cohorts were 5.8%, 9.8%, and 11.2% in 1998–2000 and 10.2%, 17.7%, and 18.9% in 2015–2016, respectively (Table 4; Fig. 1a, c). Serious infections showed similar trends when using a different denominator, i.e., per 100,000 NIS claims (Appendix 2; Fig. 1b, d).
Rates of hospitalized/serious infections in people with PMR or GCA per 100,000 claims over time. 1A. Hospitalized/serious infections per 100,000 PMR claims. 1B. Hospitalized/serious infections in PMR cohort per 100,000 NIS claims. 1C. Hospitalized/serious infections per 100,000 GCA claims. 1D. Hospitalized/serious infections in GCA cohort per 100,000 NIS claims
Incidence rates of serious infections in PMR /100,000 NIS claims in 2015–2016 were as follows (rounded off): OI, < 1; SSTI, 4; UTI, 4; pneumonia, 9; and sepsis, 20; and in GCA were: OI, < 1; SSTI, 1; UTI, 1; pneumonia, 2; and sepsis, 4 (Appendix 2). Rates decreased over time for OI and pneumonia and increased for SSTI, UTI, and sepsis (Table 4); time-trends in each infection were statistically significant for PMR and GCA (p < 0.001). During the study period, we noted increase in mean Deyo-Charlson comorbidity score in both PMR and GCA cohorts, with minimal changes in the mean age. Sepsis surpassed pneumonia as the most common serious infection in 2011–2012. The ratio of sepsis to pneumonia rates was 0.3 in 1998–2000 and 2.1 in 2015–2016.
Comparing last with the first study period, we noted decreasing length of hospital stay, in-hospital mortality, but increasing hospital charges for both PMR (Appendix 3) and GCA (Appendix 4).
Factors associated with healthcare utilization and in-hospital mortality
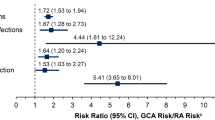
PMR
Compared with sepsis, OI, pneumonia, UTI, and SSTI had significantly lower healthcare utilization and in-hospital mortality (Table 5). Female sex, Deyo-Charlson comorbidity score ≥ 2, Medicare or Medicaid insurance, urban hospital location, and large hospital bed size were associated with significantly higher healthcare utilization and in-hospital mortality (Table 5).
GCA
Compared with sepsis, pneumonia, UTI, and SSTI had significantly lower healthcare utilization and in-hospital mortality, and OI had significantly higher healthcare utilization (Table 6). Deyo-Charlson comorbidity score ≥ 2, urban hospital location, and large hospital bed size were associated with significantly higher healthcare utilization, and Deyo-Charlson comorbidity score ≥ 2 was associated with significantly higher in-hospital mortality (Table 6).
Discussion
In this national study of serious infections in people with PMR or GCA, we found that the characteristics of people with serious infections in PMR of GCA differed from those of the general population, outcomes differed by the type of serious infection, the rate of several serious infections increased over time in both cohorts. We described the factors associated with healthcare utilization and mortality outcomes. Several findings deserve further discussion.
We noted that serious infection rates were higher in people with PMR or GCA, compared with the general US population, i.e., composite serious infection was seen in 17% in PMR, 19% in GCA hospital claims versus 10% in the NIS cohorts. This finding indicates that infections in PMR/GCA can be more severe and need to be intensively treated. This finding agrees with findings from two population-based studies that showed a higher proportion (48% in GCA versus 37% in non-GCA) with at least 1 episode of systemic infection, especially in the first 6 months of the treatment [15], and 2-fold higher incidence of severe infections in GCA versus non-GCA during the first year after diagnosis, 11.1/100 patient-years versus 5.9/100 patient-years [16]. Our finding is in contrast to Olmsted county study of the incidence of hospitalized infections in an age-, sex-, and calendar-year-matched cohort, 5.6/100 person-years in GCA (74 people; 134 episodes) versus 6.0/100 person-years in non-GCA (79 people; 153 episodes) [17]. It is possible that older age in PMR/GCA cohorts compared with the general population in our study may have contributed to higher rate of serious infection.
Both disease and its treatment in PMR or GCA are risk factors for serious infections, and associated comorbidities can also contribute. Glucocorticoids, commonly used for the treatment of PMR and GCA, reduce the migration, phagocytosis, and intracellular killing in macrophages, T cell-medicated cellular immunity, and are associated with delayed healing of skin and mucous membranes [30]. A meta-analysis of randomized trials showed that the risk of infections was higher in glucocorticoids compared with placebo [31]. Mortality caused by infections was significantly higher in patients with GCA compared with controls [16]. Diabetes and corticosteroid dose > 10 mg/day after 12 months of treatment were predictors of death in people with GCA hospitalized with severe infection [16].
Our study adds serious infection incidence rates in PMR and GCA to the literature using the national US data and time-trends, novel findings to our knowledge. An increasing medical comorbidity over time may have been a potential contributing factor to time-trends in serious infection hospitalizations in PMR and GCA cohorts. The incidence rate for the five serious infections ranged from < 1 to 20/100,000 in PMR and from < 1 to 4/100,000 in the GCA cohort. In the PMR cohort in 2015–2016, the rates in our study were 0.3 for OI, 4.5 for SSTI, 4 for UTI, 9.4 for pneumonia, and 19.6 for sepsis/100,000 NIS claims. These were 0.2 for OI, 0.7 for SSTI, 0.7 for UTI, 1.7 for pneumonia, and 4.4 for sepsis /100,000 NIS claims in the GCA cohort in 2015–2016. Time-trends of increase in serious infection incidence rates in PMR and GCA may be related to an increasing proportion of older people, increasing medical comorbidity, and worsening.
Our overall incidence of serious infections of 17.7/100 in PMR and 18.9/100 in GCA among each respective cohort in the most recent study period of 2015–2016 is similar to the reported incidence of severe infection at 11.1/100 patient-years (95% CI 8.3–14.6) in a 1991–2009 French population-based cohort of patients with GCA during the first year after diagnosis of GCA [16]. Our reported incidence of serious infections of 11.9/100 in PMR and 12.3/100 claims in GCA (within each cohort) replicates the previously reported incidence in a new country setting.
In a previous 1987–2007 UK study, the incidence rates in GCA versus non-GCA were as follows: lower respiratory tract infection (LRTI), 22.5 versus 13.5/100 person-years; UTI, 12.7 versus 9.5/100 person-years; and sepsis, 0.2 versus 0.1/100 person-years [15]. Rates in our study for the corresponding period 2007–2008 were 5.5/100 claims for pneumonia, 0.4/100 claims for UTI, and 3.4 for sepsis /100 NIS claims in GCA, i.e., higher for sepsis and lower for UTI and pneumonia. Differences in the rates between these studies may be related to differences in the country setting, time-frame (20- versus 2-year period), or definitions of various infections.
The association of sepsis with significantly higher healthcare utilization and in-hospital mortality compared with other serious infections in both cohorts was no surprise. The only exception was OI which was associated with higher healthcare utilization compared with sepsis in the GCA cohort, and no difference in mortality. In both the PMR and GCA cohorts, Deyo-Charlson comorbidity score ≥ 2, urban hospital location, and large bed size hospital were associated with significantly higher healthcare utilization and in-hospital mortality; female sex, Medicare, or Medicaid insurance were also associated in PMR cohort. Thus, our study is among the few studies of potential risk factors for higher healthcare utilization and in-hospital mortality after admission for serious infection in people with GCA or PMR.
Our study findings must be interpreted considering study limitations. Our study findings are at the risk of misclassification bias, since we used the ICD-9-CM codes to identify people with PMR/GCA (and not disease classification criteria) and serious infections, and this would likely bias the findings towards the null hypothesis. However, the infection [21,22,23,24,25] and PMR/GCA [20] diagnostic codes were shown to be valid in other similar administrative datasets, including in cohorts of people with rheumatic diseases, with high positive predictive values. NIS contains de-identified data. Therefore, a validation study for diagnostic codes cannot be performed in the NIS. Incidence rates in 2015–2016 should be interpreted with caution, since the coding system changed from ICD-9-CM in 2015 to ICD-10-CM. This may have led to up or down-coding for a given serious infection, and misclassification rates may differ between the two coding systems.
The NIS counts hospitalizations, which is our unit of analysis. NIS does not provide longitudinal data after hospital discharge, and therefore, we are unable to examine the post-discharge outcomes, and/or readmission risk. However, understanding associated healthcare utilization and mortality for serious infection in PMR and GCA fills an important knowledge gap, given the lack of these national data for the USA. NIS also does not have data on disease severity measure, laboratory test, and medications, and therefore, we could not examine the impact of these important disease variables on various outcomes. Our study strengths include the use of the US national inpatient data, inclusion of several potential confounders, and the occurrence of enough hospitalized infections in people with lupus.
Conclusions
In one of the first studies using the national US data, we described the epidemiology of hospitalized serious infections in cohorts of people with PMR or GCA. Serious infection epidemiology in PMR or GCA differed from the general population without these conditions. Sepsis surpassed pneumonia as the most frequent serious infection in 2011–2012. The ratio of sepsis to pneumonia rates increased from 0.3 in 1998–2000 to 2.1 in 2015–2016 for PMR and 2.6 for GCA. Rates decreased over time for OI and pneumonia and increased for SSTI, UTI, and sepsis. Novel patient, comorbidity, and hospital characteristic correlates of higher healthcare utilization and in-hospital mortality were found in cohorts of people with hospitalized serious infections and PMR or GCA.
References
Gonzalez-Gay MA, Vazquez-Rodriguez TR, Lopez-Diaz MJ, Miranda-Filloy JA, Gonzalez-Juanatey C, Martin J, Llorca J (2009) Epidemiology of giant cell arteritis and polymyalgia rheumatica. Arthritis Rheum 61:1454–1461
Salvarani C, Cantini F, Boiardi L, Hunder GG (2002) Polymyalgia rheumatica and giant-cell arteritis. N Engl J Med 347:261–271
Raheel S, Shbeeb I, Crowson CS, Matteson EL (2017) Epidemiology of polymyalgia rheumatica 2000-2014 and examination of incidence and survival trends over 45 years: a population-based study. Arthritis Care Res (Hoboken) 69:1282–1285
Michet CJ, Matteson EL (2008) Polymyalgia rheumatica. BMJ 336:765–769
Gonzalez-Gay MA, Matteson EL, Castaneda S (2017) Polymyalgia rheumatica. Lancet 390:1700–1712
Gonzalez-Gay MA (2004) Giant cell arteritis and polymyalgia rheumatica: two different but often overlapping conditions. Semin Arthritis Rheum 33:289–293
Evans JM, Hunder GG (2000) Polymyalgia rheumatica and giant cell arteritis. Rheum Dis Clin N Am 26:493–515
de Worm S, Giot JB, Courtoy C, Gillet E, Amrane S, Huynen P, van Esbroeck M, Prudent E, Lepidi H, Million M, Moutschen M, Raoult D (2018) A case of giant cell arteritis associated with culture-proven Coxiella burnetii aortitis. Int J Infect Dis 69:50–54
Baymakova M, Demirev A, Kostadinova I, Andonova R, Popov GT, Plochev K (2018) Giant-cell arteritis without cranial manifestations presenting as fever of unknown origin: a diagnostic value of 18F-FDG PET/CT. Clin Ter 169:e274–e2e6
Buckingham EM, Foley MA, Grose C, Syed NA, Smith ME, Margolis TP, Thurtell MJ, Kardon R (2018) Identification of herpes zoster-associated temporal arteritis among cases of giant cell arteritis. Am J Ophthalmol 187:51–60
Proven A, Gabriel SE, Orces C, O'Fallon WM, Hunder GG (2003) Glucocorticoid therapy in giant cell arteritis: duration and adverse outcomes. Arthritis Rheum 49:703–708
Dixon WG, Abrahamowicz M, Beauchamp ME, Ray DW, Bernatsky S, Suissa S, Sylvestre MP (2012) Immediate and delayed impact of oral glucocorticoid therapy on risk of serious infection in older patients with rheumatoid arthritis: a nested case-control analysis. Ann Rheum Dis 71:1128–1133
Jick SS, Lieberman ES, Rahman MU, Choi HK (2006) Glucocorticoid use, other associated factors, and the risk of tuberculosis. Arthritis Rheum 55:19–26
Singh JA, Hossain A, Kotb A, Wells G (2016) Risk of serious infections with immunosuppressive drugs and glucocorticoids for lupus nephritis: a systematic review and network meta-analysis. BMC Med 14:137
Durand M, Thomas SL (2012) Incidence of infections in patients with giant cell arteritis: a cohort study. Arthritis Care Res (Hoboken) 64:581–588
Schmidt J, Smail A, Roche B, Gay P, Salle V, Pellet H, Duhaut P (2016) Incidence of severe infections and infection-related mortality during the course of giant cell arteritis: a multicenter, prospective, double-cohort study. Arthritis Rheumatol 68:1477–1482
Udayakumar PD, Chandran AK, Crowson CS, Warrington KJ, Matteson EL (2014) Hospitalized infections in giant cell arteritis: a population-based retrospective cohort study. J Rheumatol 41:2447–2451
HCUP. Overview of the National (Nationwide) Inpatient Sample (NIS). https://www.hcup-us.ahrq.gov/nisoverview.jsp. Rockville, MD: AHRQ; 2018
HCUP Databases. Healthcare Cost and Utilization Project (HCUP). Overview of the Nationwide Inpatient Sample (NIS). http://www.hcup-us.ahrq.gov/nisoverview.jsp. Last modified 8/13/18 Rockville, MD: Agency for Healthcare Research and Quality; 2018 [cited 2019 04/26/2019]
Bernatsky S, Linehan T, Hanly JG (2011) The accuracy of administrative data diagnoses of systemic autoimmune rheumatic diseases. J Rheumatol 38:1612–1616
Jinno S, Lu N, Jafarzadeh SR, Dubreuil M (2018) Trends in hospitalizations for serious infections in patients with rheumatoid arthritis in the US between 1993 and 2013. Arthritis Care Res (Hoboken) 70:652–658
Tektonidou MG, Wang Z, Dasgupta A, Ward MM. Burden of serious infections in adults with systemic lupus erythematosus: a national population-based study, 1996-2011. Arthritis Care Res (Hoboken) 2015;67:1078–1085
Schneeweiss S, Robicsek A, Scranton R, Zuckerman D, Solomon DH (2007) Veteran’s affairs hospital discharge databases coded serious bacterial infections accurately. J Clin Epidemiol 60:397–409
Grijalva CG, Chung CP, Stein CM, Gideon PS, Dyer SM, Mitchel EF Jr, Griffin MR (2008) Computerized definitions showed high positive predictive values for identifying hospitalizations for congestive heart failure and selected infections in Medicaid enrollees with rheumatoid arthritis. Pharmacoepidemiol Drug Saf 17:890–895
Patkar NM, Curtis JR, Teng GG, Allison JJ, Saag M, Martin C et al (2009) Administrative codes combined with medical records based criteria accurately identified bacterial infections among rheumatoid arthritis patients. J Clin Epidemiol 62:321–327 7 e1-7
HCUP NIS Description of Data Elements. ZIPINC_QRTL - Median household income for patient's ZIP Code (based on current year). Healthcare Cost and Utilization Project (HCUP). September 2008. Agency for Healthcare Research and Quality, Rockville, MD. www.hcup-us.ahrq.gov/db/vars/zipinc_qrtl/nisnote.jsp Bethesda, MD: Agency for Health Care Research and Quality; 2017 [cited 2017 08/19/2017]
Deyo RA, Cherkin DC, Ciol MA (1992) Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol 45:613–619
Medicare Eligibility: Who may enroll in Medicare. https://www.ehealthmedicare.com/about-medicare/eligibility/ Baltimore, MD: Centers for Medicare and Medicaid Services; 2017 [cited 2017 08/19/2017]
Sabesan VJ, Petersen-Fitts G, Lombardo D, Briggs D, Whaley J (2017) Medicaid payer status is linked to increased rates of complications after treatment of proximal humerus fractures. J Shoulder Elb Surg 26:948–953
Klein NC, Go CH, Cunha BA (2001) Infections associated with steroid use. Infect Dis Clin N Am 15:423–432 viii
Stuck AE, Minder CE, Frey FJ (1989) Risk of infectious complications in patients taking glucocorticosteroids. Rev Infect Dis 11:954–963
Role of the funder/supporter
The funding body did not play any role in design, in the collection, analysis, and interpretation of data; in the writing of the manuscript; and in the decision to submit the manuscript for publication.
Funding
This study is funded by the research funds from the Division of Rheumatology at the University of Alabama at Birmingham and the resources and use of facilities at the Birmingham VA Medical Center, Birmingham, Alabama, USA.
Author information
Authors and Affiliations
Contributions
Mr. Cleveland had full access to all of the data in the study and takes the responsibility for the integrity of the data and accuracy of the data analysis. He was supervised by Dr. Singh, who reviewed all results. Study concept and design: Singh. Data acquisition, analysis, and interpretation of results: Singh, Cleveland. Drafting of the manuscript: Singh. Critical revision of the manuscript for important intellectual content: Singh, Cleveland. Statistical analysis: Cleveland.
Obtained funding: Singh. Administrative, technical, or material support: Singh. Study supervision: Singh.
Corresponding author
Ethics declarations
Conflict of interest
JAS has received consultant fees from Crealta/Horizon, Medisys, Fidia, UBM LLC, Trio health, Medscape, WebMD, Clinical Care options, Clearview healthcare partners, Putnam associates, Focus forward, Navigant consulting, Spherix, Practice Point communications, the National Institutes of Health and the American College of Rheumatology. JAS owns stock options in Amarin pharmaceuticals and Viking therapeutics. JAS is on the speaker’s bureau of Simply Speaking. JAS is a member of the executive of OMERACT, an organization that develops outcome measures in rheumatology and receives arms-length funding from 12 companies. JAS serves on the FDA Arthritis Advisory Committee. JAS is the chair of the Veterans Affairs Rheumatology Field Advisory Committee. JAS is the editor and the Director of the UAB Cochrane Musculoskeletal Group Satellite Center on Network Meta-analysis. JAS previously served as a member of the following committees: member, the American College of Rheumatology’s (ACR) Annual Meeting Planning Committee (AMPC) and Quality of Care Committees, the Chair of the ACR Meet-the-Professor, Workshop and Study Group Subcommittee and the co-chair of the ACR Criteria and Response Criteria subcommittee. DC has no conflicts to declare. There are no non-financial competing interests for any of the authors.
Ethics/IRB approval and consent to participate
The University of Alabama at Birmingham’s Institutional Review Board approved this study and all investigations were conducted in conformity with ethical principles of research (UAB X120207004). The IRB waived the need for an informed consent for this database study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 31 kb)
Rights and permissions
About this article
Cite this article
Singh, J.A., Cleveland, J.D. Serious infections in people with polymyalgia rheumatica (PMR) or giant cell arteritis (GCA): a time-trend national US study. Clin Rheumatol 39, 3427–3438 (2020). https://doi.org/10.1007/s10067-020-05129-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-020-05129-w