Abstract
Osteoporosis is a chronic skeletal disease with an increasing prevalence. Romosozumab, as a monoclonal anti-sclerostin antibody with a dual function, has been produced. In this meta-analysis, we aimed to examine the efficacy of Romosozumab in patients with low bone mineral density. A systematic search was conducted in the most important electronic search engines like Cochrane Library, PubMed, Web of Science, Scopus, Google Scholar, and ClinicalTrials.gov at the end of July 2019 to retrieve randomized controlled trials (RCTs), which evaluated the effect of Romosozumab in patients with osteoporosis and/or low bone mineral density. After evaluating the quality of articles with the Cochrane checklist, data related to the outcomes of bone mineral density (BMD) of lumbar spine, femoral neck, and total hip, risk of clinical, vertebral and non-vertebral fractures, and risk of adverse events were extracted. Quality of evidence was assessed according to the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) approach. Heterogeneity between studies was evaluated by I2 and Q statistics. The meta-analysis was performed using CMA v.2.0 software. Of all the 671 initially retrieved articles, seven articles were entered into the meta-analysis after removing duplicates and reviewing papers with inclusion and exclusion criteria. The results of the meta-analysis showed that Romosozumab 210, 140, and 70 mg compared with Alendronate, Teriparatide, and placebo can increase the bone mineral density in the lumbar spine, femoral neck, and total hip. The risk of adverse events like adjudicated cardiovascular serious adverse events and adjudicated cardiovascular death was more in Romosozumab 210 mg in comparison with placebo. However, this difference was not statistically significant. Treatment with anti-sclerostin antibodies can be a proper therapeutic option in patients with osteoporosis and low bone mineral density. Based on the results of this meta-analysis, it seems that Romosozumab, with its dual function, has a positive role in the treatment of osteoporosis and low bone mineral density.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is a chronic skeletal disease characterized by bone mass reduction and bone tissue deterioration. This disorder can increase the fragility of bone and consequently increase the risk of bone fracture especially in the hip, wrist, and spine [1, 2]. Osteoporosis is not restricted to specific gender or race, but the probability of its incidence increases as age increases [3]. However, osteoporosis prevalence is more in women, while the prevalence of osteoporotic fractures in men is higher, about 30–40%. Hence, men experience higher morbidity and mortality related to osteoporosis in comparison with women. This is due to the fact that osteoporosis is an underdiagnosed and undertreated condition in men [4, 5]. The decrease in quality of life, the rise of mortality risk, and the boost of economic burden on health systems are attributable to osteoporosis [6, 7].
During the past three decades, substantial progress has been made in the treatment of osteoporosis [8]. The aim of the existing medications is to maintain and increase bone mass and density and also to reduce the risk of bone fractures. Medications for the treatment of this disease can be classified into antiresorptive and anabolic medications. Examples of antiresorptive medications are estrogen agonist/antagonists (EAAs), estrogens, calcitonin, bisphosphonates, and denosumab. Teriparatide is among the anabolic category [9,10,11,12].
Romosozumab, a monoclonal anti-sclerostin antibody, with a dual function, has been produced throughout the last decade. Its rapid function in treatment is based on binding and inhibiting the sclerostin protein, which is a negative osteogenic regulator. Sclerostin can inhibit the Wnt signaling pathway that has a key role in bone metabolism. Thus, two functions of Romosozumab are increasing bone formation and reducing bone resorption [13,14,15].
Due to its novelty, Romosozumab has rarely been studied for its efficacy and safety. Two studies suggest that Romosozumab, compared with placebo, can significantly increase bone mineral density (BMD) in postmenopausal women [16, 17]. Another study showed a decrease in fracture incidence across groups that received Romosozumab compared with those who received Alendronate [18]. Adverse events such as osteoarthritis, cancer, and cardiovascular events have been reported in randomized controlled trials (RCTs) due to the use of Romosozumab [16,17,18,19,20]. Liu et al. conducted a meta-analysis in which they had included six RCTs evaluating the effect of Romosozuamb in postmenopausal women in osteoporosis [21]. As the gap of osteoporosis treatment is worse in men than women, it is essential that effectiveness in the male population be also carefully examined [22, 23]. Lewiecki et al. study [20] examined the effect of Romosozumab in the male population, which was well tolerated.
Because of the differences in the results of studies, decision making about the efficacy and safety of Romosozumab should be based on structured evidence. Meta-analysis, as a quantitative method, can gather information of independent studies and play a key role in evidence-based medicine [24]. In this meta-analysis, we aimed at examining the efficacy and safety of Romosozumab in patients with low bone mineral density.
Methods
This systematic review was conducted based on recommendations in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses [PRISMA] statement [25]. The protocol was submitted in Iran University of Medical Sciences by grant No [code: 31150–163–02-96].
Study identification
Two authors searched the electronic databases, parallely, through the keywords of BMD, osteoporosis, fractures, and Romosozumab. Articles were searched in major databases, i.e. PubMed, Cochrane Library, Web of Science, ClinicalTrials.gov, and Scopus at the end of July, 2019. Conference abstracts were also considered in our database searching.
Direct contacts to authors were initiated for cases in which the provided information was incomplete or more clarification was needed. Moreover, an identical search strategy was conducted in other databases. Further, the key journals and the reference lists of the included papers were also searched.
Study selection and data extraction
Articles were eligible if they (1) included men or women with osteoporosis or low bone mass and (2) were designed as RCTs that examined the efficacy of monthly subcutaneous Romosozumab injection with a dose of 210, 140, or 70 mg. Studies were excluded if they (1) were conducted on animals, (2) reported incomplete data on the means and standard deviation of outcomes, (3) investigated the effect of transition to another medication, or (4) were conducted or reported as qualitative studies, reviews, case reports, letter to editors, or ongoing clinical trials without posted results. If two studies had been reported from the same cohort, the largest and/or most recent study was included. Two of the authors developed a list of included studies independently and a third author was available for mediation.
Two of the authors independently extracted data from the selected studies into a standardized Microsoft Excel spreadsheet. Any disagreement was resolved by consensus or, if required, discussion with a third author. The following information was extracted from each study: (1) study characteristics (e.g. sample size, demographics, and the country in which the study was performed); (2) study setting; (3) mean of percentage change from baseline in the BMD outcomes with confidence intervals or standard deviation; (4) risk of fracture incidences; (5) number and percentage of adverse events in each group; and (6) the follow-up duration. In case of studies with different doses of Romosozumab and studies with different control groups, each dose and/or control group was considered as a separate study.
Risk of bias in individual studies
The methodology of articles was evaluated using the Standard Cochrane Collaboration risk of bias tool in Revman 5.3 software [26]. Quality of evidence for included outcomes was assessed according to the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach [27]. One of four grades of very low, low, moderate, and high represents the results of the GRADE approach.
Statistical methods
The primary outcome was the mean percentage change in the BMD of the intervention group (Romosozumab) in comparison with the control group (placebo, Alendronate, and Teriparatide). According to the doses of medicine used in the studies, the analysis was performed based on the drug dosage. The standard deviation of the mean percentage of BMD in the two groups was calculated relative to the baseline value using extracted confidence intervals of the studies. In addition, mean difference of percentage changes in BMD of intervention group was calculated relative to the control group and combined with meta-analysis. Random effect model was used for this purpose.
The secondary outcome was the risk of incidence of fractures and adverse events. For this outcome, the number of patients with adverse events and the total number of patients in the intervention and control groups was extracted. Afterwards, odds ratio was calculated for adverse effects and then combined using the random effect model.
The heterogeneity of studies was evaluated using the I2 and Q tests. In the case of heterogeneity, the random effect model was used. Meta-analysis was undertaken using Comprehensive Meta-Analysis (CMA) version 2 and R version 3.5.1 meat package. P value ≤ 0.05 was considered as a significant level [26, 28].
Results
Description of trials
Of total 671 articles retrieved in systematic search, 283 duplicate articles were excluded. Moreover, review of the titles and abstracts of the 388 remaining articles resulted in the exclusion of 366 further articles. After reading the full text of 22 articles, finally, seven of them, which encompassed 13 studies, were eligible to be included in this meta-analysis (Fig. 1). Baseline characteristics of the included studies are shown in Table 1 (excluded articles are listed in Table S1).
Quality assessment
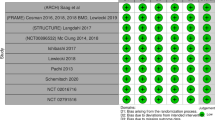
Figures 2 and 3 show the results of quality assessment based on seven criteria of Cochrane risk of bias tool. All of the included studies were randomized controlled trials. In one study, blinding of outcome assessment was not clearly reported, and this issue can impose detection bias [20]. In another study, an open-label manner can cause selection and performance bias [19]. The role of Amgen Inc. and UCB Pharma pharmaceutical companies, as funders, probably impose “other bias” in all included studies.
Meta-analysis
Seven original pepers were included in the meta-analysis, which were considered as 13 separate studies due to subgroup analysis of dosages of Romosozumab.
In all of the included studies, 6393 patients initially received Romosozumab. Among patients who received Romosozumab, 6165 patients were treated with Romosozumab 210 mg, 114 patients were treated with Romosozumab 140 mg, and 114 patients were treated with Romosozumab 70 mg. The mean age of participants was 68.60 years, and mean age based on dosage was 69.26, 68.13, and 66.2 for Romosozumab 210, 140, and 70 mg, respectively. Romosozumab was administered subcutaneously in all patients. Dual-energy x-ray absorptiometry at different stages was done to assess BMD. P1NP and β-CTX were checked via fasting serum samples at the baseline in different months.
BMD (lumbar spine)
Forest plot of BMD of the lumbar spine is shown in Fig. 4.
Romosozumab 210 mg vs. Alendronate
Two articles with 2095 patients in Romosozumab group and 2099 patients in Alendronate group were included. The heterogeneity of studies for the BMD of the lumbar spine in Romosozumab 210 mg compared with Alendronate was significant (I2 = 72.62%, Q-value = 3.65, P value = 0.06). As shown in Fig. 4, Romosozumab 210 mg can change BMD 8.13% more compared with Alendronate (95% CI: 6.07–9.56).
Romosozumab 210 mg vs. Teriparatide
Two articles with 255 patients in Romosozumab group and 264 patients in Teriparatide group were included. The heterogeneity of studies for the BMD of the lumbar spine in Romosozumab 210 mg compared with Teriparatide was not significant (I2 = 0%, Q-value = 0.05, P value = 0.83). As shown in Fig. 4, Romosozumab 210 mg can change BMD 4.34% more compared with Teriparatide (95% CI: 3.49–5.18).
Romosozumab 210 mg vs. placebo
Three articles with 148 patients in Romosozumab group and 146 patients in placebo group were included. The heterogeneity of studies for the BMD of the lumbar spine in Romosozumab 210 mg compared with placebo was significant (I2 = 92.0%, Q-value = 16.18, P value < 0.001). As shown in Fig. 4, Romosozumab 210 mg can change BMD 12.39% more compared with placebo (95% CI: 8.75–16.02).
Romosozumab 140 mg vs. placebo
Two articles with 114 patients in Romosozumab group and 115 patients in placebo group were included. The heterogeneity of studies for the BMD of the lumbar spine in Romosozumab 140 mg compared with placebo was significant (I2 = 97.61%, Q-value = 41.87, P value < 0.001). As shown in Fig. 4, Romosozumab 140 mg can change BMD 8.95% more compared with placebo (95% CI: 2.19–15.71).
Romosozumab 70 mg vs. placebo
Two articles with 114 patients in Romosozumab group and 115 patients in placebo group were included. The heterogeneity of studies for the BMD of the lumbar spine in Romosozumab 70 mg compared with placebo was significant (I2 = 76.25%, Q-value = 4.21, P value = 0.04). As shown in Fig. 4, Romosozumab 70 mg can change BMD 6.55% more compared with placebo (95% CI: 4.59–8.51).
BMD (Total hip)
Forest plot of BMD of the total hip is shown in Fig. 5.
Romosozumab 210 mg vs. Alendronate
Two articles with 2096 patients in Romosozumab group and 2098 patients in Alendronate group were included. The heterogeneity of studies for the BMD of the total hip in Romosozumab 210 mg compared with Alendronate was significant (I2 = 83.22%, Q-value = 5.96, P value = 0.01). As shown in Fig. 5, Romosozumab 210 mg can change BMD 2.88% more compared with Alendronate (95% CI: 1.72–4.05).
Romosozumab 210 mg vs. Teriparatide
Two articles with 256 patients in Romosozumab group and 261 patients in Teriparatide group were included. The heterogeneity of studies for the BMD of the total hip in Romosozumab 210 mg compared with Teriparatide was not significant (I2 = 10.0%, Q-value = 1.11, P value = 0.29). As shown in Fig. 5, Romosozumab 210 mg can change BMD 3.19 % more compared with Teriparatide (95% CI: 2.64–3.75).
Romosozumab 210 mg vs. placebo
Three articles with 149 patients in Romosozumab group and 144 patients in placebo group were included. The heterogeneity of studies for the BMD of the total hip in Romosozumab 210 mg compared with placebo was not significant (I2 = 74.0%, Q-value = 1.03, P value = 0.02). As shown in Fig. 5, Romosozumab 210 mg can change BMD 3.90% more compared with placebo (95% CI: 2.71–5.09).
Romosozumab 140 mg vs. placebo
Two articles with 114 patients in Romosozumab group and 115 patients in placebo group were included. The heterogeneity of studies for the BMD of the total hip in Romosozumab 140 mg compared with placebo was not significant (I2 = 0%, Q-value = 0.84, P value = 0.36). As shown in Fig. 5, Romosozumab 140 mg can change BMD 2.31% more compared with placebo (95% CI: 1.66–2.95).
Romosozumab 70 mg vs. placebo
Two articles with 114 patients in Romosozumab group and 115 patients in placebo group were included. The heterogeneity of studies for the BMD of the total hip in Romosozumab 70 mg compared with placebo was not significant (I2 = 0%, Q-value = 0.53, P value = 0.47). As shown in Fig. 5, Romosozumab 70 mg can change BMD 1.75% more compared with placebo (95% CI: 1.08–2.42).
BMD (femoral neck)
Forest plot of BMD of the femoral neck is shown in Fig. 6.
Romosozumab 210 mg vs. Alendronate
Two articles with 2096 patients in Romosozumab group and 2098 patients in Alendronte group were included. The heterogeneity of studies for the BMD of the femoral neck in Romosozumab 210 mg compared with Alendronate was not significant (I2 = 5.93%, Q-value = 1.06, P value = 0.30). As shown in Fig. 6, Romosozumab 210 mg can change BMD 3.12% more compared with Alendronate (95% CI: 2.7–3.55).
Romosozumab 210 mg vs. Teriparatide
Two articles with 256 patients in Romosozumab group and 264 patients in Teriparatide group were included. The heterogeneity of studies for the BMD of the femoral neck in Romosozumab 210 mg compared with Teriparatide was not significant (I2 = 4.36%, Q-value = 1.05, P value = 0.31). As shown in Fig. 6, Romosozumab 210 mg can change BMD 3.15 % more compared with Teriparatide (95% CI: 2.42–3.88).
Romosozumab 210 mg vs. placebo
Three articles with 146 patients in Romosozumab group and 144 patients in placebo group were included. The heterogeneity of studies for the BMD of the femoral neck in Romosozumab 210 mg compared with placebo was not significant (I2 = 64.0%, Q-value = 1.78, P value = 0.06). As shown in Fig. 6, Romosozumab 210 mg can change BMD 3.61% more compared with placebo (95% CI: 2.18–5.04).
Romosozumab 140 mg vs. placebo
Two articles with 114 patients in Romosozumab group and 115 patients in placebo group were included. The heterogeneity of studies for the BMD of the femoral neck in Romosozumab 140 mg compared with placebo was not significant (I2 = 32.24%, Q-value = 1.84, P value = 0.22). As shown in Fig. 6, Romosozumab 140 mg can change BMD 2.06% more compared with placebo (95% CI: 0.98–3.14).
Romosozumab 70 mg vs. placebo
Two articles with 114 patients in Romosozumab group and 115 patients in placebo group were included. The heterogeneity of studies for the BMD of the femoral neck in Romosozumab 70 mg compared with placebo was significant (I2 = 59.33%, Q-value = 2.46, P value = 0.12). As shown in Fig. 6, Romosozumab 70 mg can change BMD 1.03% more compared with placebo (95% CI: −0.24- 2.29).
Risk of fracture
Risk of clinical, vertebral, and non-vertebral fracture was investigated in two studies comparing Romosozumab 210 mg with Alendronate and placebo [16, 18]. One study reported the incidence of fractures as an adverse effect [20]. Considering that the control group was different in these two studies, we could not conduct analysis in this outcome. We only systematically report the results.
In Cosman et al. study, the risk of new vertebral fracture, in Romosozumab 210 mg was 73% lower than the placebo group (RR = 0.27; 95%CI: 0.16–0.47). Risks of clinical fracture and non-vertebral fractures were 36 and 25% lower in Romosozumab 210 mg than that of placebo group, respectively [16].
In Saag et al. study, the risk of new vertebral fracture in Romosozumab 210 mg was lower than in Alendronate group RR = 0.63; 95%CI: 0.47–0.85). Risk of clinical fractures and non-vertebral fractures was also lower in Romosozumab group than in placebo by 28 and 26%, respectively [18].
In Lewiecki et al. study, the incidence of fractures was reported as an adverse effect, which included combination of vertebral and non-vertebral fractures. Incidence of fractures was 1.8 and 2.5% in Romosozumab 210 mg and placebo group, respectively [20].
Markers of bone turnover
The bone-formation marker P1NP and the bone-resorption marker β-CTX
In the Cosman et al. and Lewieki et al. study, the maximum decrease and increase in the levels of P1NP and β-CTX after the first dose of the Romosozumab in these measurements were significantly more than the placebo group [16, 20].
Ishibashi et al. showed that, in all Romosozumab doses, P1NP had a rapid increase depending on the Romosozumab dose. The decrease in β-CTX was significantly more in Romosozumab groups than in placebo, and the maximum decrease was in week 1 [17].
In Langdhal et al. study, the increase of P1NP levels in the Romosozumab group was more than the increase in the Teriparatide group on day 14. During the 12 months, the P1NP levels decreased to the baseline measurements in the Romosozumab group. The maximum decrease in the levels of β-CTX was on day 14 in the Romosozumab group and after 3 months returned to the baseline measurements. Finally P1NP and β-CTX concentrations in the Teriparatide group were significantly more than Romosozumab group [19].
In McClung et al. study, the levels of P1NP increased after initial administration of Romosozumab, and the largest increase was after one month. The levels of β-CTX returned below the baseline measurements at month 12 [29].
In Saag et al. study, increase in the levels of P1NP and decrease in levels of the β-CTX within 12 months were significant in Romosozumab group [18].
Safety
Death
Romosozumab 210 mg vs. placebo
Three articles with 3801 patients in Romosozumab group and 3720 patients in placebo group were included. In this outcome, the heterogeneity of studies for Romosozumab 210 mg compared with placebo was not significant (I2 = 0%, Q-value = 1.07, P value = 0.58). Odds of death among patients who received placebo was 0.15 times lower than Romosozumab 210 mg (OR = 0.85; 95%CI: 0.5–1.45) (online resource Fig. S1).
Romosozumab 70 mg vs. placebo
Two articles with 114 patients in Romosozumab group and 115 patients in placebo group were included. In this outcome, the heterogeneity of studies for Romosozumab 70 mg compared with placebo was not significant (I2 = 0%, Q-value = 0.05, P value = 0.82). Odds of death among patients who received placebo was 0.75 times lower than Romosozumab 70 mg (OR = 0.25; 95%CI: 0.03–2.26) (online resource Fig. S1).
Adjudicated cardiovascular serious events
Romosozumab 210 mg vs. placebo
Two articles with 3752 patients in Romosozumab group and 3673 patients in placebo group were included. In this outcome, the heterogeneity of studies for Romosozumab 210 mg compared with placebo was not significant (I2 = 0%, Q-value = 0.62, P value = 0.43). Odds of adjudicated cardiovascular serious events among patients who received placebo was 0.11 times lower than in Romosozumab 210 mg group (OR = 0.89; 95% CI: 0.59–1.34) (online resource Fig. S2).
Adjudicated cardiovascular death
Romosozumab 210 mg vs. placebo
Two articles with 3744 patients in Romosozumab group and 3657 patients in placebo group were included. In this outcome, the heterogeneity of studies for Romosozumab 210 mg compared with placebo was not significant (I2 = 0%, Q-value = 0.01, P value = 0.92). Odds of adjudicated cardiovascular death among patients who received placebo was 0.11 times lower than in Romosozumab 210 mg group (OR = 0.89; 95% CI: 0.46–1.74) (online resource Fig. S3).
Osteoarthritis
Romosozumab 210 mg vs. placebo
Three articles with 3815 patients in Romosozumab group and 3736 patients in placebo group were included. In this outcome, the heterogeneity of studies for Romosozumab 210 mg compared with placebo was significant (I2 = 61.94%, Q-value = 5.25, P value = 0.07). Odds of osteoarthritis among patients who received placebo was 0.26 times lower than Romosozumab 210 mg (OR = 0.74; 95% CI: 0.25–2.2) (online resource Fig. S4).
Hypersensitivity
Romosozumab 210 mg vs. placebo
Two articles with 3652 patients in Romosozumab group and 3654 patients in placebo group were included. In this outcome, the heterogeneity of studies for Romosozumab 210 mg compared with placebo was not significant (I2 = 0%, Q-value = 0.49, P value = 0.48). Odds of hypersensitivity among patients who received placebo was 0.02 times more than in Romosozumab 210 mg group (OR = 1.02; 95% CI: 0.85–1.23) (online resource Fig. S5).
Cancer
Romosozumab 210 mg vs. placebo
Three articles with 3815 patients in Romosozumab group and 3736 patients in placebo group were included. In this outcome, the heterogeneity of studies for Romosozumab 210 mg compared with placebo was not significant (I2 = 0%, Q-value = 0.62, P value = 0.73). Odds of cancer among patients who received placebo was 0.16 times more than in Romosozumab 210 mg group (OR = 1.16; 95% CI: 0.82–1.63) (online resource Fig. S6).
Injection-site reaction
Romosozumab 210 mg vs. Alendronate
Two articles with 2098 patients in Romosozumab group and 2098 patients in Alendronte group were included. In this outcome, the heterogeneity of studies for Romosozumab 210 mg compared with Alendronate was not significant (I2 = 0%, Q-value = 0.23, P value = 0.63). Odds of injection-site reaction among patients who received Alendronate was 0.43 times lower than Romosozumab 210 mg (OR = 0.57; 95% CI: 0.41–0.8) (online resource Fig. S7).
Romosozumab 210 mg vs. placebo
Four articles with 3864 patients in Romosozumab group and 3783 patients in placebo group were included. In this outcome, the heterogeneity of studies for Romosozumab 210 mg compared with placebo was not significant (I2 = 0%, Q-value = 0.13, P value = 0.99). Odds of injection-site reaction among patients who received placebo was 0.45 times lower than Romosozumab 210 mg (OR = 0.55; 95% CI: 0.43–0.69) (online resource Fig. S7).
Romosozumab 210 mg vs. Teriparatide
Two articles with 270 patients in Romosozumab group and 273 patients in Teriparatide group were included. In this outcome, the heterogeneity of studies for Romosozumab 210 mg compared with Teriparatide was not significant (I2 = 0%, Q-value = 0.01, P value = 0.94). Odds of injection-site reaction among patients who received Teriparatide was 0.67 times lower than Romosozumab 210 mg (OR = 0.33; 95% CI: 0.14–0.79) (online resource Fig. S7).
Adverse event leading to discontinuation of study drug
Romosozumab 210 mg vs. placebo
Three articles with 3815 patients in Romosozumab group and 3736 patients in placebo group were included. In this outcome, the heterogeneity of studies for Romosozumab 210 mg compared with placebo was not significant (I2 = 0%, Q-value = 1.44, P value = 0.49). Odds of adverse event leading to discontinuation of study drug among patients who received placebo was 0.08 times more than in Romosozumab 210 mg (OR = 1.08; 95% CI: 0.72–1.6) (online resource Fig. S8).
Any adverse event
Romosozumab 210 mg vs. Alendronate
Two articles with 2098 patients in Romosozumab group and 2098 patients in Alendronte group were included. In this outcome, the heterogeneity of studies for Romosozumab 210 mg compared with Alendronate was not significant (I2 = 0%, Q-value = 0.3, P value = 0.58). Odds of any adverse event among patients who received placebo was 0.12 times more than in Romosozumab 210 mg (OR = 1.12; 95% CI: 0.97–1.29) (online resource Fig. S9).
Romosozumab 210 mg vs. Teriparatide
Two articles with 270 patients in Romosozumab group and 273 patients in Teriparatide group were included. In this outcome, the heterogeneity of studies for Romosozumab 210 mg compared with Teriparatide was not significant (I2 = 0%, Q-value = 0.49, P value = 0.48). Odds of any adverse event among patients who received Teriparatide was 0.35 times lower than Romosozumab 210 mg (OR = 0.65; 95% CI: 0.45–0.95) (online resource Fig. S9).
Romosozumab 210 mg vs. placebo
Four articles with 3864 patients in Romosozumab group and 3783 patients in placebo group were included. In this outcome, the heterogeneity of studies for Romosozumab 210 mg compared with placebo was significant (I2 = 74.38%, Q-value = 11.71, P value = 0.01). Odds of any adverse event among patients who received placebo was 0.33 times lower than Romosozumab 210 mg (OR = 0.77; 95% CI: 0.43–1.36) (online resource Fig. S9).
Romosozumab 140 mg vs. placebo
Two articles with 114 patients in Romosozumab group and 115 patients in placebo group were included. In this outcome, the heterogeneity of studies for Romosozumab 140 mg compared with placebo was significant (I2 = 82.97%, Q-value = 5.87, P value = 0.02). Odds of Adverse event leading to discontinuation of study drug among patients who received placebo was 0.55 times lower than Romosozumab 140 mg (OR = 0.45; 95% CI: 0.43–1.36) (online resource Fig. S9).
Romosozumab 70 mg vs. placebo
Two articles with 114 patients in Romosozumab group and 115 patients in placebo group were included. In this outcome, the heterogeneity of studies for Romosozumab 70 mg compared with placebo was significant (I2 = 88.58%, Q-value = 8.76, P value < 0.001). Odds of adverse event leading to discontinuation of study drug among patients who received placebo was 0.79 times lower than Romosozumab 70 mg (OR = 0.21; 95% CI: 0.02–1.94) (online resource Fig. S9).
GRADE of evidence
Based on the results of the GRADE approach, the quality of evidence of outcome measures (BMD of lumbar spine, total hip, femoral neck and risk of adverse events) were rated as high, moderate and low. The results are summarized in Tables 2 and 3.
Sensitivity analysis
All of the included studies were in patients with osteoporosis except McClung et al., which was in patients with low bone mass. In McClung et al. study, the baseline BMD of total hip and femoral neck for Romosozumab 210, 140, and 70 mg, Alendronte, Teriparatide, and placebo were normal (− 1.45, − 1.67, − 1.69, − 1.55, − 1.32, and 1.39 for total hip and − 1.87, − 2.03, − 2.06, − 1.91, − 1.79, and − 1.80 for femoral neck, respectively). However, the low bone mass in lumbar spine had maximum baseline T score for Romosozumab 210, 140, and 70 mg, Alendronte, Teriparatide, and placebo (− 2.33, − 2.27, − 2.35, − 2.08, − 2.29, and − 2.27, respectively). Also, they did not use FRAX for treatment of patients with low bone mass [29]. In order to investigate this heterogeneity in the results, the mentioned study was excluded from meta-analysis, and the changes in primary outcomes of Romosozumab 210 mg compared with placebo were investigated in osteoporosis patients. Based on the results of meta-analysis, in the Romosozumab 210 mg group, the mean change of BMD were 1.67, 2.97, and 1.28% of lumbar spine, femoral neck, and total hip, which were respectively more than in placebo group. The results of meta-analysis without considering McClung et al. study is shown in Table 4. For other groups, it was not possible to conduct meta-analysis after removing the mentioned study.
Discussion
The inhibition of bone formation is done by sclerostin antibody, which is produced by osteocytes. Romosozumab, a monoclonal anti-sclerostin antibody, can neutralize the sclerostin function and increase bone mineral density [30]. According to the mechanism of Romosozumab, there may be hope for those patients who need to increase bone production as well as those who have gotten no results by using bisphosphonates; therefore, this medication can be a good alternative. To investigate the effect of this drug, there are several outcomes that should be considered. Based on clinical trials in this area, Romosozumab can increase BMD and thereby decrease fracture incidence [16,17,18, 29, 31]. Since BMD should be monitored for a long time, at least 1 to 2 years, researchers must notice bone turnover markers like serum procollagen type I N-terminal propeptide (P1NP) and bone resorption marker collagen type 1 β-carboxy-telopeptide (β-CTX), which affect more quickly than BMD [32, 33]. Investigating Romosozumab efficacy and safety has been conducted in several clinical trials in both animals and humans [16, 34,35,36,37].
In this study, we reviewed the changes in BMD of patients with osteoporosis and low bone density treated with Romosozumab in five studies [16, 17, 29, 31, 38]. The results of the meta-analysis showed that different doses of Romosozumab can significantly increase the BMD in lumbar spine, total hip, and femoral neck compared with Alendronate, Teriparatide, and placebo. On the other hand, Romosozumab resulted in a significant increase in BMD and such increase was more obvious at the dose of 210 mg rather than 140 and 70 mg. The overall results showed that Romosozumab 210 mg was more effective in increasing BMD of all three skeletal locations. Quality of evidence was high in outcomes of BMD lumbar spine, total hip, and femoral neck for Romosozumab 210 mg compared with Teriparatide that means the true effect of Romosozumab 210 mg compared with Teriparatide is likely to be similar to our estimates [39]. The results of RCT studies were similar to ours. Moreover, they found that Romosozumab at a dose of 210 mg was more effective than doses of 140 and 70 mg in increasing BMD [17, 29].
Based on the results of previous clinical trials on the efficacy of Romosozumab in increasing BMD and the effect on the risk of fracture incidence, this drug gets the FDA’s approval for osteoporosis treatment in postmenopausal women. However, based on the FDA’s reports, this medication may have a negative effect on patients, such as serious cardiovascular events [23, 40]. In the present meta-analysis, adjudicated cardiovascular serious adverse events and adjudicated cardiovascular were lower in Romosozumab 210 mg compared with the placebo. However, analysis of other Romosozumab doses and control groups was not applicable due to the small number of studies and insufficient data.
Osteoarthritis was another complication investigated in the present meta-analysis. Romosozumab may cause osteoarthritis, especially in patients with homozygous genetic deficiency of sclerostin [41]. Although in our meta-analysis the risk of osteoarthritis was more in Romosozumab 210 mg than the placebo, we should take into consideration that this difference was not statistically significant.
The effect of Romosozumab on the incidence of fractures was investigated in two clinical trials [16, 18]. The result of one study demonstrated that uptake of Romosozumab 210 mg, compared with placebo, resulted in fewer clinical fractures [16]. Another clinical trial showed similar results by comparing Romosozumab 210 mg with Alendronate [18]. The efficacy of Alendronate, compared with Denosumab, was investigated in a meta-analysis according to which there was no significant difference between the two drugs in decreasing fracture incidence [42]. Because the control groups in two included studies were different, we could not conduct analysis on the risk of clinical, new vertebral, and non-vertebral fractures [16, 18].
A meta-analysis by Liu et al. [21] examined the efficacy and safety of Romosozumab in women with osteoporosis by including six RCTs [16,17,18,19, 34]. We excluded Genant et al. study [34] because of the difference in the kind of BMD outcomes, which considered volumetric BMD, areal BMD, and bone mineral content (BMC). On the other hand, our search strategy was based on a longer period of time (the end of July 2019(; therefore, we included Lewiecki et al.’s study and a new RCT from clinicalTrials.gov [20, 38]. The differences in the present study and Liu’s were, first, the included population. In the present meta-analysis, we included both men and women. Another strength of our research was considering all doses of Romosozumab (210, 140, and 70 mg) with all control groups (Alendronte, Teriparatide, and placebo), and analysis was performed with respect to all doses of Romosozumab as well as control groups. In the Liu’s study, just doses of 210 and 70 Romosozumab were considered; however, ultimately, contrary to our study, these different doses of Romosozumab were not analyzed separately in comparison with the control groups. For safety analysis, we have analyzed and reported all possible side effects, while, in the mentioned study, just incidence of adverse effects was reported.
Bone biomarkers, P1NP and β-CTX, were studied in several studies [16, 17, 29]. All the included studies in the present meta-analysis showed consistent results and approved dual effect of Romosozumab in osteoporosis and low bone mineral density [16, 17, 29, 31]. However, in this outcome, there was no sufficient data on different phases of biomarkers measurements; therefore, it wasn’t possible to conduct the meta-analysis.
This study had some limitations. Since Romosozumab was relatively a new medicine at the time of the study, clinical studies on this medication were limited. To confirm the results of efficacy and safety, there will be a need for further studies that compare Romosozumab with common medications for osteoporosis with longer follow-ups. Only one of the included studies in our meta-analysis had examined the effect of this drug on men. However, it was not included for meta-analysis of safety outcomes due to insufficient data in BMD outcomes [20]. Therefore, researchers should be careful about using the safety results of this study in the male population based on the inclusion criteria of the present study for considering both patients with osteoporosis and low bone mass. One of the studies included in our meta-analysis had investigated the effects of Romosozumab in patients with low bone mass. The eligibility criterion for the mentioned study was patients with T score between − 2 and − 3.5. Thus, further studies are required in both populations [29]. Based on National Osteoporosis Foundation (NOF) guidelines, it is better to treat patients based on fracture risk assessment tool (FRAX). The FRAX uses several clinical risk factors with or without BMD to predict 10-year probability of hip fracture and major osteoporotic fractures [43, 44]. Furthermore, using this tool in articles will make reports more consistent and easier to compare.
According to available data at this time, we think that Romosozumab should be considered for patients that have not had adequate response to other osteoporotic drugs. We have to be cautious about prescribing Romosozumab in patients with moderate to severe osteoarthritis because, theoretically, inhibitions of WNT signaling pathways can accelerate osteoarthritis. But, like other drugs, which were first used in refractory patients and then became one of the first choices (for example Rituximab in ANCA associated vasculitis), we have to do more clinical trials so that the Romosozumab in newly diagnosed osteoporotic patients is prescribed with longer follow up and less bias (for example, we refer to McClung et al. study [29] that did not use FRAX and also treated osteopenic patients).
Conclusion
Treatment with anti-sclerostin antibodies can be a proper therapeutic option in patients with low bone mineral density. However, due to the limited number of studies in this area and concerns about safety issues, specifically, cardiovascular events, its widespread use requires more investigation and longer follow-up durations.
References
Papapoulos S, Lippuner K, Roux C, Lin CJ, Kendler DL, Lewiecki EM, Brandi ML, Czerwinski E, Franek E, Lakatos P, Mautalen C, Minisola S, Reginster JY, Jensen S, Daizadeh NS, Wang A, Gavin M, Libanati C, Wagman RB, Bone HG (2015) The effect of 8 or 5 years of denosumab treatment in postmenopausal women with osteoporosis: results from the FREEDOM extension study. Osteoporos Int 26(12):2773–2783. https://doi.org/10.1007/s00198-015-3234-7
Rachner TD, Khosla S, Hofbauer LC (2011) Osteoporosis: now and the future. Lancet 377(9773):1276–1287. https://doi.org/10.1016/s0140-6736(10)62349-5
Kling JM, Clarke BL, Sandhu NP (2014) Osteoporosis prevention, screening, and treatment: a review. J Women's Health (Larchmt) 23(7):563–572. https://doi.org/10.1089/jwh.2013.4611
Amelio P, Isaia GC (2015) Male osteoporosis in the elderly. Int J Endocrinol 2015:8. https://doi.org/10.1155/2015/907689
Bello MO, Garla VV (2019) Osteoporosis in males. In: StatPearls [internet]. StatPearls Publishing
Orive M, Aguirre U, Garcia-Gutierrez S, Las Hayas C, Bilbao A, Gonzalez N, Zabala J, Navarro G, Quintana JM (2015) Changes in health-related quality of life and activities of daily living after hip fracture because of a fall in elderly patients: a prospective cohort study. Int J Clin Pract 69(4):491–500. https://doi.org/10.1111/ijcp.12527
Vergara I, Vrotsou K, Orive M, Gonzalez N, Garcia S, Quintana JM (2014) Factors related to functional prognosis in elderly patients after accidental hip fractures: a prospective cohort study. BMC Geriatr 14:124. https://doi.org/10.1186/1471-2318-14-124
Bolland MJ, Grey AB, Gamble GD, Reid IR (2010) Effect of osteoporosis treatment on mortality: a meta-analysis. J Clin Endocrinol Metab 95(3):1174–1181. https://doi.org/10.1210/jc.2009-0852
Ettinger MP (2003) Aging bone and osteoporosis: strategies for preventing fractures in the elderly. Arch Intern Med 163(18):2237–2246. https://doi.org/10.1001/archinte.163.18.2237
Lewiecki EM (2010) Bisphosphonates for the treatment of osteoporosis: insights for clinicians. Ther Adv Chronic Dis 1(3):115–128. https://doi.org/10.1177/2040622310374783
Tella SH, Gallagher JC (2014) Biological agents in management of osteoporosis. Eur J Clin Pharmacol 70(11):1291–1301
Tu KN, Lie JD, Wan CKV, Cameron M, Austel AG, Nguyen JK, Van K, Hyun D (2018) Osteoporosis: a review of treatment options. P T 43(2):92–104
Becker CB (2014) Sclerostin inhibition for osteoporosis--a new approach. N Engl J Med 370(5):476–477. https://doi.org/10.1056/NEJMe1315500
Costa AG, Bilezikian JP, Lewiecki EM (2014) Update on romosozumab: a humanized monoclonal antibody to sclerostin. Expert Opin Biol Ther 14(5):697–707. https://doi.org/10.1517/14712598.2014.895808
McClung MR (2017) Sclerostin antibodies in osteoporosis: latest evidence and therapeutic potential. Ther Adv Musculoskelet Dis 9(10):263–270. https://doi.org/10.1177/1759720x17726744
Cosman F, Crittenden DB, Adachi JD, Binkley N, Czerwinski E, Ferrari S, Hofbauer LC, Lau E, Lewiecki EM, Miyauchi A, Zerbini CA, Milmont CE, Chen L, Maddox J, Meisner PD, Libanati C, Grauer A (2016) Romosozumab treatment in postmenopausal women with osteoporosis. N Engl J Med 375(16):1532–1543. https://doi.org/10.1056/NEJMoa1607948
Ishibashi H, Crittenden DB, Miyauchi A, Libanati C, Maddox J, Fan M, Chen L, Grauer A (2017) Romosozumab increases bone mineral density in postmenopausal Japanese women with osteoporosis: a phase 2 study. Bone 103:209–215. https://doi.org/10.1016/j.bone.2017.07.005
Saag KG, Petersen J, Brandi ML, Karaplis AC, Lorentzon M, Thomas T, Maddox J, Fan M, Meisner PD, Grauer A (2017) Romosozumab or alendronate for fracture prevention in women with osteoporosis. N Engl J Med 377(15):1417–1427. https://doi.org/10.1056/NEJMoa1708322
Langdahl BL, Libanati C, Crittenden DB, Bolognese MA, Brown JP, Daizadeh NS, Dokoupilova E, Engelke K, Finkelstein JS, Genant HK, Goemaere S, Hyldstrup L, Jodar-Gimeno E, Keaveny TM, Kendler D, Lakatos P, Maddox J, Malouf J, Massari FE, Molina JF, Ulla MR, Grauer A (2017) Romosozumab (sclerostin monoclonal antibody) versus teriparatide in postmenopausal women with osteoporosis transitioning from oral bisphosphonate therapy: a randomised, open-label, phase 3 trial. Lancet 390(10102):1585–1594. https://doi.org/10.1016/s0140-6736(17)31613-6
Lewiecki EM, Blicharski T, Goemaere S, Lippuner K, Meisner PD, Miller PD, Miyauchi A, Maddox J, Chen L, Horlait S (2018) A phase III randomized placebo-controlled trial to evaluate efficacy and safety of Romosozumab in men with osteoporosis. J Clin Endocrinol Metab 103(9):3183–3193. https://doi.org/10.1210/jc.2017-02163
Liu Y, Cao Y, Zhang S, Zhang W, Zhang B, Tang Q, Li Z, Wu J (2018) Romosozumab treatment in postmenopausal women with osteoporosis: a meta-analysis of randomized controlled trials. Climacteric 21(2):189–195. https://doi.org/10.1080/13697137.2018.1433655
Solomon DH, Johnston SS, Boytsov NN, McMorrow D, Lane JM, Krohn KD (2014) Osteoporosis medication use after hip fracture in U.S. patients between 2002 and 2011. J Bone Miner Res 29(9):1929–1937. https://doi.org/10.1002/jbmr.2202
Vidal M, Thibodaux RJ, Neira LFV, Messina OD (2019) Osteoporosis: a clinical and pharmacological update. Clin Rheumatol 38(2):385–395. https://doi.org/10.1007/s10067-018-4370-1
Glasser SP, Duval S (2014) Meta-analysis, evidence-based medicine, and clinical guidelines. In: Essentials of Clinical Research. Springer, pp 203–231
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7):e1000097. https://doi.org/10.1371/journal.pmed.1000097
Higgins JP, Green S (2011) Cochrane handbook for systematic reviews of interventions, vol 4. Wiley
Schünemann HJ, Oxman AD, Brozek J, Glasziou P, Bossuyt P, Chang S, Muti P, Jaeschke R, Guyatt GH (2008) GRADE: assessing the quality of evidence for diagnostic recommendations. BMJ Evid Based Med 13(6):162–163
Deeks JJ, Higgins JP, Altman DG (2008) Analysing data and undertaking meta-analyses. In: Cochrane handbook for systematic reviews of interventions, pp 241–284
McClung MR, Grauer A, Boonen S, Bolognese MA, Brown JP, Diez-Perez A, Langdahl BL, Reginster JY, Zanchetta JR, Wasserman SM, Katz L, Maddox J, Yang YC, Libanati C, Bone HG (2014) Romosozumab in postmenopausal women with low bone mineral density. N Engl J Med 370(5):412–420. https://doi.org/10.1056/NEJMoa1305224
MacNabb C, Patton D, Hayes JS (2016) Sclerostin antibody therapy for the treatment of osteoporosis: clinical prospects and challenges. J Osteoporos 2016:6217286. https://doi.org/10.1155/2016/6217286
Keaveny TM, Crittenden DB, Bolognese MA, Genant HK, Engelke K, Oliveri B, Brown JP, Langdahl BL, Yan C, Grauer A, Libanati C (2017) Greater gains in spine and hip strength for Romosozumab compared with Teriparatide in postmenopausal women with low bone mass. J Bone Miner Res 32(9):1956–1962. https://doi.org/10.1002/jbmr.3176
Tsai JN, Burnett-Bowie SM, Lee H, Leder BZ (2017) Relationship between bone turnover and density with teriparatide, denosumab or both in women in the DATA study. Bone 95:20–25. https://doi.org/10.1016/j.bone.2016.11.009
Tsujimoto M, Chen P, Miyauchi A, Sowa H, Krege JH (2011) PINP as an aid for monitoring patients treated with teriparatide. Bone 48(4):798–803. https://doi.org/10.1016/j.bone.2010.12.006
Genant HK, Engelke K, Bolognese MA, Mautalen C, Brown JP, Recknor C, Goemaere S, Fuerst T, Yang YC, Grauer A, Libanati C (2017) Effects of Romosozumab compared with Teriparatide on bone density and mass at the spine and hip in postmenopausal women with low bone mass. J Bone Miner Res 32(1):181–187. https://doi.org/10.1002/jbmr.2932
Matheny JB, Torres AM, Ominsky MS, Hernandez CJ (2017) Romosozumab treatment converts trabecular rods into trabecular plates in male Cynomolgus monkeys. Calcif Tissue Int 101(1):82–91. https://doi.org/10.1007/s00223-017-0258-3
Ominsky MS, Boyd SK, Varela A, Jolette J, Felx M, Doyle N, Mellal N, Smith SY, Locher K, Buntich S, Pyrah I, Boyce RW (2017) Romosozumab improves bone mass and strength while maintaining bone quality in ovariectomized cynomolgus monkeys. J Bone Miner Res 32(4):788–801. https://doi.org/10.1002/jbmr.3036
Padhi D, Allison M, Kivitz AJ, Gutierrez MJ, Stouch B, Wang C, Jang G (2014) Multiple doses of sclerostin antibody romosozumab in healthy men and postmenopausal women with low bone mass: a randomized, double-blind, placebo-controlled study. J Clin Pharmacol 54(2):168–178. https://doi.org/10.1002/jcph.239
NCT02791516 (2018) A safety and efficacy study to evaluate romosozumab (AMG 785) in South Korean women with osteoporosis. https://ClinicalTrials.gov/show/NCT02791516. Accessed 23 July 2019
Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, Norris S, Falck-Ytter Y, Glasziou P, DeBeer H, Jaeschke R, Rind D, Meerpohl J, Dahm P, Schunemann HJ (2011) GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol 64(4):383–394. https://doi.org/10.1016/j.jclinepi.2010.04.026
FDA approves new treatment for osteoporosis in postmenopausal women at high risk of fracture (2019) FDA. https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm635653.htm. Accessed 10 April 2019
Balemans W, Ebeling M, Patel N, Van Hul E, Olson P, Dioszegi M, Lacza C, Wuyts W, Van Den Ende J, Willems P, Paes-Alves AF, Hill S, Bueno M, Ramos FJ, Tacconi P, Dikkers FG, Stratakis C, Lindpaintner K, Vickery B, Foernzler D, Van Hul W (2001) Increased bone density in sclerosteosis is due to the deficiency of a novel secreted protein (SOST). Hum Mol Genet 10(5):537–543. https://doi.org/10.1093/hmg/10.5.537
Lin T, Wang C, Cai XZ, Zhao X, Shi MM, Ying ZM, Yuan FZ, Guo C, Yan SG (2012) Comparison of clinical efficacy and safety between denosumab and alendronate in postmenopausal women with osteoporosis: a meta-analysis. Int J Clin Pract 66(4):399–408. https://doi.org/10.1111/j.1742-1241.2011.02806.x
Beaudoin C, Moore L, Gagne M, Bessette L, Ste-Marie LG, Brown JP, Jean S (2019) Performance of predictive tools to identify individuals at risk of non-traumatic fracture: a systematic review, meta-analysis, and meta-regression. Osteoporos Int 30(4):721–740. https://doi.org/10.1007/s00198-019-04919-6
Rubin KH, Abrahamsen B, Friis-Holmberg T, Hjelmborg JV, Bech M, Hermann AP, Barkmann R, Gluer CC, Brixen K (2013) Comparison of different screening tools (FRAX(R), OST, ORAI, OSIRIS, SCORE and age alone) to identify women with increased risk of fracture. A population-based prospective study. Bone 56(1):16–22. https://doi.org/10.1016/j.bone.2013.05.002
Acknowledgments
The authors would like to thank Dr. Masoud Mozafari for facilitating this research and author collaborations. Moreover, we would like to express our gratitude to Dr. Bahareh Malmir, Ph.D in Applied Linguistics, who performed the language edition of the present article.
Funding
This research was supported by grant no. [Code: 31150–163–02-96] from Iran University of Medical Sciences.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 971 kb).
Rights and permissions
About this article
Cite this article
Kaveh, S., Hosseinifard, H., Ghadimi, N. et al. Efficacy and safety of Romosozumab in treatment for low bone mineral density: a systematic review and meta-analysis. Clin Rheumatol 39, 3261–3276 (2020). https://doi.org/10.1007/s10067-020-04948-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-020-04948-1