Abstract
Introduction
Discordance (misalignment) regarding treatment satisfaction may exist in real-life clinical practice between patients and their physicians. We aimed to assess physician and patient treatment satisfaction levels and associated degree of misalignment in rheumatoid arthritis (RA).
Method
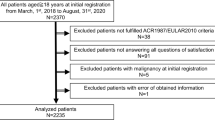
A point-in-time, multinational survey of patients and physicians was conducted in Latin America from December 2014 to October 2015. Physician- and patient-reported satisfaction levels with current RA treatment, alignment levels in satisfaction perception, and factors associated with satisfaction misalignment were assessed through bivariate and logistic regression analyses.
Results
Participating physicians (N = 114) completed 555 patient record forms (PRFs); 372 patients completed self-complete questionnaires (PSC). A total of 346 physician-patient pairs were analyzed. Physicians reported satisfaction with current disease control in 270/346 (78.0%) PRFs; patients reported such satisfaction in 286/346 (82.7%) PSCs. Physician-patient alignment was observed in 78.6% of pairs. Compared with aligned patients, misaligned patients were younger, more likely to have moderate or severe disease (physician subjectively defined), deteriorating or unstable disease (physician subjectively defined), been exposed to a greater number of advanced therapy lines (biologic or Janus kinase inhibitor), greater current pain, a current acute episode, poorer health, and greater disability and impairment. Misaligned patients were less likely to be in remission. Logistic regression analysis revealed that misaligned patients were more likely to experience greater activity impairment.
Conclusions
High treatment satisfaction and alignment were observed among RA patients and their physicians in Latin America. Misaligned patients were more likely to report more severe disease and were less likely to be in remission. Addressing misalignment may lead to improved RA disease control.
Key Points • High treatment satisfaction was observed among RA patients and their treating physicians in Latin America. • One-fifth of physician-patient pairs were misaligned in treatment satisfaction. • Patients misaligned with their physicians reported higher disease activity, lower quality of life, and greater disability than those who were aligned with their physicians. • Understanding and addressing misalignment in treatment satisfaction may improve outcomes in this patient population. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rheumatoid arthritis (RA) is a chronic inflammatory joint disease characterized by persistent synovitis, systemic inflammation and autoantibodies [1, 2]. If left uncontrolled, RA causes joint damage, disability, reduced quality of life, and cardiovascular and other comorbidities [2]. Treating RA in a Latin American healthcare context has been recognized as challenging. This is due to factors such as lack of easy access to the healthcare system thus delaying medical evaluation, few rheumatologists in secondary and tertiary care causing lack of availability of specialist appointments [3, 4], and cultural concepts that assume “rheumatism” is a mild problem and that rheumatic diseases are “irreversible and incurable” and caused by the natural aging process [3].
Low income and lower literacy are associated with delayed and irregular use of biological disease-modifying antirheumatic drugs (DMARDs) [3]. Recent treatment recommendations from both the European League Against Rheumatism (EULAR) [5] and the American College of Rheumatology (ACR) [6] incorporate a treat-to-target approach, which aims for remission or low disease activity in RA patients [7]. While there is knowledge of these goals and strategies in Latin America, it is not thought they are used widely [8]. Several Latin American rheumatology societies and associations (e.g., members of PANLAR) have developed their own guidelines or recommendations for the management of RA [9]. Recommended pharmacologic therapy for RA consists of a “step-up” approach beginning with DMARDs and escalating to biologic or targeted synthetic DMARDs if treatment targets are not achieved [5, 6].
It is hypothesized that the physician-patient relationship (“working alliance”) is an integral component of the treatment of RA patients. The physician-patient working alliance has been shown to predict patient satisfaction, and that patient satisfaction in turn predicts patient adherence to medication [10]. Patient and physician satisfaction with RA treatment have been explored in previous research, particularly in a US and European context [10,11,12]. However, to our knowledge, satisfaction and any associated misalignment in satisfaction have not been explored in a Latin American context and are little understood.
In this study, we explored the clinical and physician-reported implications of misalignment in satisfaction with treatment control between RA patients and their physicians in Latin America. We explored physician- and patient-reported levels of satisfaction with current RA treatment, levels of alignment in perceptions of satisfaction, factors associated with misalignment in satisfaction and the implications of misalignment in RA patients.
Materials and methods
Data were extracted from a survey of physicians and their patients conducted between December 2014 and October 2015 in Latin America (Mexico, Venezuela, Colombia, Argentina). The survey was a large, multinational, cross-sectional study conducted in clinical practice, in which physicians described current disease management, disease-burden impact and associated treatment effects (clinical and physician-perceived) in their patients who presented in a real-world clinical setting. The survey methods have been validated and are presented elsewhere [13,14,15].
Participating physicians and patients
A geographically diverse selection of rheumatologists participated in this study. To be eligible, participating physicians must have been personally responsible for treatment decisions and management of patients with RA. Physicians also had a minimum workload of the following number of RA patients per month: Argentina, 6 patients; Mexico, 4 patients; Columbia, 5 patients; Venezuela, 4 patients. Eligible patients were adult (> 18 years of age), had a physician-confirmed diagnosis of RA, were not currently involved in a clinical trial and visited the physician, and were prescribed advanced therapy (AT), specifically a biologic (originator or biosimilar) or a JAK inhibitor.
Data collection
Patient record forms (PRFs) were completed by physicians; PRFs contain detailed questions on patient demographics, clinical status, concomitant conditions, current treatment and treatment history. Each patient for whom the physician completed a PRF for was then invited to anonymously complete a patient self-complete form (PSC), although this was not mandatory. PSCs contained detailed questions on patient-reported outcomes, such as health (measured via the EuroQol 5-dimension [EQ-5D] instrument) [16], disability (measured via the Patient-Reported Outcomes Measurement Information System Health Assessment Questionnaire [PROMIS HAQ]) [17], work and productivity (measured via the Work Productivity and Activity Impairment [WPAI] questionnaire) [18], comorbidities (Charlson comorbidity index) [19], medication compliance (assessed via PSCs) and satisfaction with disease control. Physicians described their satisfaction with current disease control by choosing one of the following three responses: “Satisfied with control achieved”/“Not satisfied, but I believe this is the best control that can be realistically achieved for this patient”/“Not satisfied, and I believe better control can be achieved for this patient.” Patients described their satisfaction with current disease control by choosing one of the following three responses: “Satisfied”/“Not satisfied, but I believe this it the best that can be achieved for my condition”/“Not satisfied, and I believe better control can be achieved for my condition.” Disease severity was assessed by asking the physician to categorize the patient as mild, moderate, or severe; current disease progression was assessed by asking the physician to categorize the patient as improving, stable, deteriorating slowly, deteriorating rapidly, or unstable; and current remission was assessed by asking the physician to categorize the patient as in remission or not in remission. No definitions of severity, disease progression or remission were provided to the physicians a priori, and patients were categorized solely by subjective physician assessment. Patient-reported emotional burden factors were assessed via patient queries regarding attitudes towards medications (“I am always keen to try the next new treatment for my condition and will ask my doctor about any new ones which become available”) and their physicians (“I feel like my doctor fully involves me in treatment decisions and allows me to help manage my own condition”; “I would change my doctor if I felt that he/she was not willing to try new therapies”; “My current doctor has helped me to deal with the psychological and emotional burden of my disease”). These queries were scored from 1 to 10 (1 = completely disagree; 10 = completely agree).
Ethics
All participating patients provided informed consent for use of their anonymized and aggregated data for research and publication in scientific journals. Data collection was performed such that patients and physicians could not be identified directly, and all data were aggregated and de-identified before receipt. Data collection was performed in accordance with the European Pharmaceutical Marketing Research Association [20] guidelines; ethics committee approval was thus not required. Each survey was performed in full accordance with relevant legislation at the time of data collection, including the US Health Insurance Portability and Accountability Act 1996 [21] and Health Information Technology for Economic and Clinical Health Act legislation [22].
Statistical methods
Statistical analyses were performed with Stata version 15.1 (StataCorp, College Station, Texas).
Comparing physician- and patient-reported treatment satisfaction
Physicians and patients were reclassified as yes/no for satisfaction. The “yes” category included those who selected “Satisfied with control achieved” while the “no” category included those who selected the other two available responses.
By matching satisfaction with treatment responses across physicians and their patients, a binary variable of patients who were aligned/misaligned with their physicians was created. The level of physician-patient pairs classified as aligned (both physician and patient “satisfied” or “dissatisfied”) was then calculated. The level of pairs classified as misaligned (physician “satisfied” and patient “dissatisfied” and vice versa) was also determined. The kappa measure of agreement was determined to assess the level of agreement between patients and physicians, whereby a value of < 0.00 was considered poor; 0.00–0.20 slight; 0.21–0.40 fair; 0.41–0.60 moderate; 0.61–0.80 substantial; and 0.81–1.00 almost perfect agreement [23].
Variation in aligned/misaligned patients according to key sociodemographic, clinical and patient-reported variables (bivariate analysis)
To assess how aligned/misaligned patients varied by key sociodemographic, clinical and patient-reported characteristics, bivariate analysis was performed to compare the aligned/misaligned patient groups. For numerical variables, sample size, mean and standard deviation are given. For categorical variables, sample size, number and percent in each category are given. The Mann-Whitney U test was used for continuous outcomes, chi-squared tests for categorical outcome variables with more than two groups and Fisher’s exact test when the variable was binary.
Association between alignment and sociodemographic, clinical and patient-reported variables (multivariate analysis)
We also performed a logistic regression analysis to explore the association between alignment and sociodemographic, clinical and patient-reported variables. The binary variable of “aligned” or “misaligned” was treated as a dependent (outcome) variable. Variables for inclusion in the regression were selected after authors review of bivariate analysis results. Variables that were shown to be significant (P < 0.05), were of interest or deemed important to reduce confounding were eligible for inclusion in the model. After authors discussion, variables meeting the above criteria and that were not co-linear with each other were included in the model. Demographic factors included age, gender and BMI. Clinical factors included current disease progression, number of symptoms, number of AT lines, current acute episode (flaring) and current remission. Patient-reported characteristics included EQ-5D, medication compliance, activity impairment and tiredness/exhaustion.
Sub-analysis of misaligned patients (bivariate analysis)
Misaligned patients were further grouped on the basis of being satisfied in comparison to their physician (physician dissatisfied); variation in key sociodemographic, clinical and patient-reported characteristics were examined. The binary variable of patient satisfied (and physician dissatisfied) or patient dissatisfied (and physician satisfied) was treated as a dependent (outcome) variable. For categorical variables, sample size and number and percent in each category are reported. The Mann-Whitney U test was used for continuous outcomes, chi-squared test for categorical outcome variables with more than two groups and Fisher’s exact test when the variable was binary. These results are reported in supplementary tables available online (Online Resources 1 and 2).
Results
A total of 114 rheumatologists completed 555 PRFs; 372 patients completed PSCs. A total of 346 matched physician-patient pairs were analyzed. Patient demographic data are shown in Table 1.
Treatment satisfaction
Physicians reported satisfaction with current disease control in 270/346 (78.0%) PRFs; patients reported satisfaction with disease control in 286/346 (82.7%) PSCs (Table 2).
Alignment between physicians and patients
Alignment was observed in 78.6% (272/346) of physician-patient pairs (Table 2). Misalignment between physicians and patients was driven primarily by physicians expressing greater dissatisfaction with disease control (45/346 = 13.0%) than patients (29/346 = 8.4%) (Table 2). Kappa analysis indicated a fair level of agreement (κ = 0.325, 95% confidence interval [CI] 0.205 to 0.445) (Table 2).
Factors associated with alignment
Misaligned vs aligned patients were more likely to be younger (mean age: 49.2 vs 52.8 years; P = 0.04) and to have moderate or severe disease (48.6 vs 25.0%; P = 0.0002), deteriorating or unstable disease (33.8 vs 13.0%; P = 0.0001), greater mean number of AT lines (1.4 vs 1.2; P = 0.03), a higher mean current level of pain (4.6 vs 3.0; P < 0.0001), a current acute episode (43.9 vs 13.6%; P < 0.0001), poorer health according to the EQ-5D (mean score: 0.6 vs 0.7; P < 0.0001) and greater disability according to PROMIS HAQ (mean score 26.2 vs 20.1; P = 0.0004) (Table 3). Misaligned vs aligned patients scored higher in all categories of the WPAI and were less likely to be in remission (23.0 vs 54.4%; P < 0.0001) (Table 3).
A sub-analysis (available in supplementary tables online, Online Resources 1 and 2) of the 74 misaligned physician-patient pairs was performed. This analysis revealed that patients who were satisfied but their physician was dissatisfied (n = 45) were more likely to have moderate to severe disease (64.4 vs 24.1%; P = 0.0009), deteriorating or unstable disease (45.2 vs 15.3%; P = 0.03), been prescribed AT sooner (mean 41.7 vs 28.6 months ago; P = 0.04), a greater current level of pain (mean score 5.3 vs 3.4; P < 0.0001) and a current acute episode (57.5 vs 23.1%; P = 0.01) than patients who were dissatisfied but their physician was satisfied. Satisfied patients with a dissatisfied physician were also less likely to be in remission (8.9 vs 44.8%; P = 0.0005) (available in supplementary tables online, Online Resource 2).
Logistic regression analysis
Logistic regression showed that greater activity impairment as assessed by the WPAI (odds ratio 1.021, 95% CI 1.000 to 1.042; P = 0.048) (Table 4) was independently associated with misalignment. Logistic regression analysis also revealed that unstable disease progression, to be currently experiencing an acute episode, to have poorer health according to the EQ-5D and not to be in remission were also associated with misalignment though these coefficients were not statistically significant.
Discussion
This survey revealed high levels of treatment satisfaction among Latin American RA patients and their treating physicians. Patients misaligned with their physicians reported higher disease activity, lower quality of life and greater disability than those aligned.
On the basis of the physician’s own definition of severity, 30.1% of the patients in this cohort had moderate or severe disease. Although over a quarter of the patients had this level of disease severity, out of the entire cohort most patients (82.7%) expressed satisfaction with treatment. A previous study conducted in a European RA population revealed a statistically significant association between patient satisfaction and disease control (measured as Disease Activity Score in 28 joints [DAS28] > 3.2 [inadequate control] or DAS28 ≤ 3.2 [adequate control]). Over a quarter (27%) of the patients in this cohort had inadequate disease control and over half (55%) of the patients with inadequate disease control nevertheless expressed satisfaction [24]. These two studies in different regional populations suggest that patients may express satisfaction despite suboptimal disease control because of a belief that any improvement from baseline, even if modest, is satisfactory.
A sub-analysis of misaligned patients also revealed that satisfied patients (with a dissatisfied physician) had suboptimal disease control when compared with dissatisfied patients (with a satisfied physician). In this sub-analysis, satisfied patients had more severe disease and were less likely to be in remission despite having been prescribed AT sooner. However, we did not observe any statistically significant factors that could explain the differences between these groups.
A lower proportion of physicians expressed satisfaction when compared with their patients (78.0 vs 82.7%), and most of the discordant physician-patient pairs consisted of a dissatisfied physician and a satisfied patient (13.0 vs 8.4%). Patients misaligned with their physicians were more likely to have greater disease severity, less likely to be in remission, but also more likely to have received a greater number of AT lines. Physician dissatisfaction may thus be driven in part by the observation that misaligned patients were still not achieving sufficient disease control despite having attempted more AT agents.
Logistic regression analysis revealed that while misaligned patients were statistically more likely to experience activity impairment, the effect size was small.
The approach used in this study has some limitations. The cohort presented here may not be representative of the overall RA population in each respective country. Latin America is a region with large economic inequality and not all patients with RA have access to public or private healthcare or specialized rheumatology services [3, 4]. The patients in this analysis may thus be biased towards those who have the logistical and financial means to access such services along with AT. Information on patient socioeconomic status or education was not available; these factors may impact therapy adherence and the physician-patient relationship. Additionally, some variables in the study were assessed using physician’s own subjective definitions, leading to consistency of application fluctuating across physicians. The study does not survey a true random sample of physicians or patients. Although participating physicians were selected via minimal inclusion criteria, participation was influenced by willingness to complete the survey. No formal patient selection verification procedures were in place. To avoid selection bias, physicians were asked to provide data for a consecutive series of patients. While no formalized patient diagnostic criteria were employed, this is representative of the physician’s real-world classification and assessment of the patient. The point-in-time study design prevents any conclusions about causal relationships; however, identification of significant associations is nevertheless possible. Common to other surveys, recall bias might also have affected the responses of both patients and physicians to the questionnaires. However, the data for these analyses were collected at the time of each patient’s appointment and this is expected to have reduced the likelihood of recall bias.
Conclusion
This study of RA patients in Latin America revealed high levels of physician and patient satisfaction with treatment. One-fifth of physician-patient pairs were misaligned in satisfaction. Misaligned patients were more likely to have more severe disease and greater disability and impairment. Understanding and addressing misalignment may improve outcomes in this patient population.
References
Smolen JS, Aletaha D, McInnes IB (2016) Rheumatoid Arthritis. Lancet 388(10055):2023–2038. https://doi.org/10.1016/S0140-6736(16)30173-8
Scott DL, Wolfe F, Huizinga TW (2010) Rheumatoid Arthritis. Lancet 376(9746):1094–1108. https://doi.org/10.1016/S0140-6736(10)60826-4
Rocha FA (2017) Latin-American challenges and opportunities in rheumatology. Arthritis Res Ther 19(1):29. https://doi.org/10.1186/s13075-017-1247-7
da Mota LM, Brenol CV, Palominos P, Pinheiro Gda R (2015) Rheumatoid arthritis in Latin America: the importance of an early diagnosis. Clin Rheumatol 34(Suppl 1):S29–S44. https://doi.org/10.1007/s10067-015-3015-x
Smolen JS, Landewe R, Bijlsma J, Burmester G, Chatzidionysiou K, Dougados M, Nam J, Ramiro S, Voshaar M, van Vollenhoven R, Aletaha D, Aringer M, Boers M, Buckley CD, Buttgereit F, Bykerk V, Cardiel M, Combe B, Cutolo M, van Eijk-Hustings Y, Emery P, Finckh A, Gabay C, Gomez-Reino J, Gossec L, Gottenberg JE, Hazes JMW, Huizinga T, Jani M, Karateev D, Kouloumas M, Kvien T, Li Z, Mariette X, McInnes I, Mysler E, Nash P, Pavelka K, Poor G, Richez C, van Riel P, Rubbert-Roth A, Saag K, da Silva J, Stamm T, Takeuchi T, Westhovens R, de Wit M, van der Heijde D (2017) EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2016 update. Ann Rheum Dis 76(6):960–977. https://doi.org/10.1136/annrheumdis-2016-210715
Singh JA, Saag KG, Bridges SL Jr, Akl EA, Bannuru RR, Sullivan MC, Vaysbrot E, McNaughton C, Osani M, Shmerling RH, Curtis JR, Furst DE, Parks D, Kavanaugh A, O’Dell J, King C, Leong A, Matteson EL, Schousboe JT, Drevlow B, Ginsberg S, Grober J, St Clair EW, Tindall E, Miller AS, McAlindon T, American College of R (2016) 2015 American College of Rheumatology guideline for the treatment of rheumatoid arthritis. Arthritis Care Res 68(1):1–25. https://doi.org/10.1002/acr.22783
Smolen JS, Aletaha D, Bijlsma JW, Breedveld FC, Boumpas D, Burmester G, Combe B, Cutolo M, de Wit M, Dougados M, Emery P, Gibofsky A, Gomez-Reino JJ, Haraoui B, Kalden J, Keystone EC, Kvien TK, McInnes I, Martin-Mola E, Montecucco C, Schoels M, van der Heijde D, Committee TTE (2010) Treating rheumatoid arthritis to target: recommendations of an international task force. Ann Rheum Dis 69(4):631–637. https://doi.org/10.1136/ard.2009.123919
Burgos-Vargas R, Catoggio LJ, Galarza-Maldonado C, Ostojich K, Cardiel MH (2013) Current therapies in rheumatoid arthritis: a Latin American perspective. Reumatol Clin 9(2):106–112. https://doi.org/10.1016/j.reuma.2012.09.001
Brenol CV, Nava JI, Soriano ER (2015) Proper management of rheumatoid arthritis in Latin America. What the guidelines say? Clin Rheumatol 34(Suppl 1):S51–S55. https://doi.org/10.1007/s10067-015-3016-9
Fuertes JN, Anand P, Haggerty G, Kestenbaum M, Rosenblum GC (2015) The physician-patient working alliance and patient psychological attachment, adherence, outcome expectations, and satisfaction in a sample of rheumatology patients. Behav Med 41(2):60–68. https://doi.org/10.1080/08964289.2013.875885
Barton JL (2009) Patient preferences and satisfaction in the treatment of rheumatoid arthritis with biologic therapy. Patient Prefer Adherence 3:335–344
Wolfe F, Michaud K (2007) Resistance of rheumatoid arthritis patients to changing therapy: discordance between disease activity and patients’ treatment choices. Arthritis Rheum 56(7):2135–2142. https://doi.org/10.1002/art.22719
Anderson P, Benford M, Harris N, Karavali M, Piercy J (2008) Real-world physician and patient behaviour across countries: Disease-Specific Programmes - a means to understand. Curr Med Res Opin 24(11):3063–3072. https://doi.org/10.1185/03007990802457040
Babineaux SM, Curtis B, Holbrook T, Milligan G, Piercy J (2016) Evidence for validity of a national physician and patient-reported, cross-sectional survey in China and UK: the Disease Specific Programme. BMJ Open 6(8):e010352. https://doi.org/10.1136/bmjopen-2015-010352
Higgins V, Piercy J, Roughley A, Milligan G, Leith A, Siddall J, Benford M (2016) Trends in medication use in patients with type 2 diabetes mellitus: a long-term view of real-world treatment between 2000 and 2015. Diabetes Metab Syndr Obes 9:371–380. https://doi.org/10.2147/DMSO.S120101
van Reenen MOM (2015) EQ-5D-3L User Guide. EuroQol Research Foundation, Rotterdam
Khanna D, Krishnan E, Dewitt EM, Khanna PP, Spiegel B, Hays RD (2011) The future of measuring patient-reported outcomes in rheumatology: Patient-Reported Outcomes Measurement Information System (PROMIS). Arthritis Care Res 63(Suppl 11):S486–S490. https://doi.org/10.1002/acr.20581
Reilly MC, Zbrozek AS, Dukes EM (1993) The validity and reproducibility of a work productivity and activity impairment instrument. Pharmacoeconomics 4(5):353–365. https://doi.org/10.2165/00019053-199304050-00006
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40(5):373–383
European Pharmaceutical Market Research Association (EphMRA) Code of conduct Updated March 2017. (2017). https://www.ephmra.org/standards/code-of-conduct/code-of-conduct-online/. Accessed 25 Aug 2018
Services UDoHaH (2003) Summary of the HIPAA privacy rule. http://www.hhs.gov/sites/default/files/privacysummary.pdf. Accessed 25 Aug 2018
Technology HI Health information technology act. https://www.hhs.gov/sites/default/files/ocr/privacy/hipaa/administrative/enforcementrule/enfifr.pdf?language=es. Accessed 25 Aug 2018
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33(1):159–174
Taylor PC, Alten R, Gomez-Reino JJ, Caporali R, Bertin P, Sullivan E, Wood R, Piercy J, Vasilescu R, Spurden D, Alvir J, Tarallo M (2018) Clinical characteristics and patient-reported outcomes in patients with inadequately controlled rheumatoid arthritis despite ongoing treatment. RMD Open 4(1):e000615. https://doi.org/10.1136/rmdopen-2017-000615
Acknowledgments
The authors would like to thank all patients and physicians who took part in the survey. Derek Ho, PhD, provided medical writing support in the development of this manuscript. FZ, LA and FL are employees of Janssen, who sponsored this research.
Funding
EH, OM and SL are employees of Adelphi Real World who received funding from Janssen for this research. Other authors do not have a financial relationship with Janssen.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have access to the primary data and agree the journal can review data if requested. FZ, LA and FL are employees of Janssen, who sponsored this research. EH, OM and SL are employees of Adelphi Real World who received funding from Janssen for this research. Other authors do not have a financial relationship with Janssen.
Ethical approval
All participating patients provided informed consent for use of their anonymized and aggregated data for research and publication in scientific journals. Data collection was performed such that patients and physicians could not be identified directly, and all data were aggregated and de-identified before receipt. Data collection was performed in accordance with the European Pharmaceutical Marketing Research Association [20] guidelines; ethics committee approval was thus not required. Each survey was performed in full accordance with relevant legislation at the time of data collection, including the US Health Insurance Portability and Accountability Act 1996 [21] and Health Information Technology for Economic and Clinical Health Act legislation [22].
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 45 kb)
Rights and permissions
About this article
Cite this article
Alves Pereira, I., Maldonado Cocco, J., Feijó Azevedo, V. et al. Levels of satisfaction with rheumatoid arthritis treatment and associated alignment between physicians and patients across Latin America. Clin Rheumatol 39, 1813–1822 (2020). https://doi.org/10.1007/s10067-019-04858-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-019-04858-x