Abstract
Studies examining the association between alcohol intake and the risk of osteonecrosis of the femoral head (ONFH) have inconsistent results. The purpose of this study was to examine and summarize the evidence regarding the association between alcohol intake and ONFH based on results from case-control studies. This analysis included five case-control studies reporting data from 1251 individuals. Alcohol intake habits (never, former, or current), average drinking consumption (g/week), and cumulative drinking consumption (drink-years) were extracted. The risk of ONFH was evaluated, and a two-stage dose-response meta-analysis was performed using restricted cubic splines with four knots at fixed percentiles of 5, 35, 65, and 95% of the distribution. Former alcohol intake increased the risk of ONFH with a marginal significance (odds ratio [OR], 2.62; p = 0.055). Current alcohol intake was associated with an increased risk of ONFH (OR, 3.63; p < 0.001 in occasional drinkers, OR, 5.90; p < 0.001 in daily drinkers). The dose-response meta-analysis revealed that the risk of ONFH increased by 35.3% for every 100 g/week (95% confidence interval [CI], 1.24–1.47; p < 0.001) and by 44.1% for every 500 g drink-years (95% CI, 1.295–1.601; p < 0.001). Current intake and the dose of alcohol were positively associated with an increased risk of ONFH in a non-linear pattern.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteonecrosis of the femoral head (ONFH) frequently leads to hip joint destruction and damages patient’s quality of life [1]. This debilitating disease represents a significant socioeconomic burden on both individuals and healthcare systems because it commonly occurs in young and active adults and the incidence has increased annually [2, 3]. In nationwide surveys from Korea and Japan, the annual prevalence of the disease was more than 10,000 [4]. In the USA, approximately 20,000 patients are affected with the disease each year [5]. Osteonecrosis has a multifactorial etiology [3]. Underlying genetic predisposition and exposure to risk factors including alcohol and steroids have synergistic role in the pathogenesis of the disease [6].
Although individual sensitivity to alcohol also appears to be an important factor for ONFH development, alcohol has been known as an independent risk factor, when taken in excess [7, 8]. However, detailed pathogenesis for alcohol-induced ONFH has not been well established. Suggested mechanism includes fat cell proliferation and hypertrophy, diminished hematopoiesis, and decreased osteogenesis, which interact together, forming a vicious cycle of ischemia in the femoral head [9, 10].
The relationship between alcohol intake and the risk of ONFH was first reported in a multicenter case-control study [8]. Although a dose-dependent association was observed, the odds ratios (ORs) were not consistent among the studies [11, 12], and the exact dose-response relationship has not been determined yet.
Thus, a dose-response meta-analysis was conducted to assess the relationship between the quantity of alcohol intake and the risk of ONFH [13]. For the measurement of cumulative exposure, we used drink-years of alcohol.
Materials and methods
Literature search and study selection criteria
This review was performed according to the criteria for conducting and reporting meta-analysis of observational studies in epidemiology (Online Resource 1) [14]. PubMed-Medline, Embase, Cochrane Library, and Web of Science were searched in January 2016 by combining synonymous or related key terms (osteonecrosis OR avascular necrosis OR aseptic necrosis) AND (alcohol OR ethanol OR drinking). An overview of the search strategy is presented in Online Resource 2. We restricted our review to English studies, owing to translation of non-English language studies and lack of resources for review. The references of all selected articles were manually searched to identify any additional relevant studies. The decision whether an identified article would be eligible for the review was made prior to initiating the search.
Two independent reviewers (Y.B.H. and K.T.Y.) first screened the titles and abstracts to identify the relevant investigations. A third reviewer (K.K.H.) settled discrepancies between these two reviewers. Population-based epidemiological studies that investigated the association between alcohol intake and the risk of ONFH, including cross-sectional studies, case-control studies, and cohort studies, were included. We also included articles that reported adjusted effect estimates (OR) and 95% confidence intervals (CIs) for comparisons of different categories of alcohol intake. We excluded articles that involved subjects younger than 18 years [15], review articles, basic science articles, comments, letters, and protocols.
Outcome measure and data extraction
The primary outcome of interest was the rate of ONFH. Drinkers were defined as those who consumed more than 6.4 g (8 mL) of alcohol per week [8]. Drinking habits were classified into three categories: never, former, and current. With respect to alcohol intake, average drinking consumption (g/week) and cumulative drinking (drink-years) were extracted. The cumulative amount of drinking (drink-years) was calculated as follows: drink-years = weekly ethanol consumption (g)/7 × the total years of drinking [12].
For every eligible study, the following data were also extracted by two independent reviewers: the first author’s name, the year of publication, enrollment period, study design, sample size, mean age, percentage of male patients, covariates, and patient demographics. Then, all data were entered in a spreadsheet. For studies that reported several multivariable-adjusted ORs, we selected the effect estimate that was maximally adjusted for potential confounders.
Quality assessment
The Newcastle-Ottawa Scale was used to assess the quality of the enrolled studies. This tool comprises three parameters: selection, comparability, and outcome [16]. Each parameter consists of subcategorized questions: selection (a maximum of four stars), comparability (a maximum of two stars), and exposure or outcome (a maximum of three stars). A study can be awarded a maximum of nine stars, indicating the highest quality. Two of the authors (Y.B.H. and K.T.Y.) independently evaluated the quality of all the studies (Online Resource 3).
Data synthesis and analysis
We examined the relationship between alcohol intake and the risk of ONFH based on the effect estimate (relative risk, odds ratio, or hazards ratio) and its 95% CI in each study. Using a comparative meta-analysis, we evaluated the association between the habit of alcohol intake (never, former, or current) and the risk of ONFH. Because no heterogeneity was found, we reported the data from a fixed-effect model [17].
We conducted a two-stage dose-response random-effects meta-regression analysis [18, 19] and estimated the dose-response relationship curve by taking into account the covariance among risk estimates for different exposure categories [18]. A potential non-linear relation between alcohol intake and ONFH risk was investigated using restricted cubic splines with four knots at fixed percentiles (5, 35, 65, and 95%) of the exposure distribution [18, 19]. This method requires stating the distribution of cases and non-cases or person-time and the OR with its CIs for at least three quantitative exposure categories. For this reason, a study that reported only two exposure categories was excluded from this meta-analysis [20]. The midpoint of each exposure category was assigned to each corresponding risk estimate. When the upper category was open-ended, the midpoint between the upper boundary value and the midpoint value of the preceding category was assigned to the risk estimate. Likewise, when the lower category was open-ended, the midpoint between the lower boundary value and the midpoint value of the next category was assigned to the risk estimate. We assigned a null value to the lowest category, composed by never drinkers in all the studies.
Sensitivity analyses were conducted by stratifying for study design and by excluding one study at the time to evaluate if results were particularly influenced by single studies.
In all meta-regression models, statistical heterogeneity between studies was evaluated with the Cochran’s Q-test and the I2 statistic. We assessed publication bias with Begg’s funnel plot [21] and Egger’s test [22]. All analyses were performed using STATA (version 14.0; Stata Corporation, College Station, TX, USA). This study was exempted from institutional review board (IRB) review because it did not involve human subjects.
Results
Literature selection
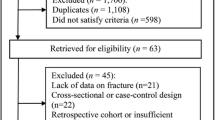
The selection process of the studies is shown in Fig. 1. Five studies were finally selected. All studies were from Japan [7, 8, 11, 12, 23] and involved a total of 1251 subjects. The general characteristics of the five studies are presented in Table 1. All of the five studies showed a significant dose-response relationship.
Drinking habits and the risk of ONFH
Two studies reported the OR of the current drinking habit into subcategory: occasional (at least once a week) and regular (daily) categories [7, 8]. Thus, the meta-analysis was performed using the ORs from occasional drinking and regular drinking from these two studies. Former alcohol intake was marginally associated with an increased risk of ONFH (OR, 2.63; p = 0.055; Fig. 2). Current alcohol intake was significantly associated with an increased risk of ONFH on occasional drinking (OR, 3.63; p < 0.001; Fig. 2) and on regular drinking (OR, 5.90; p < 0.001; Fig. 2). There was no significant heterogeneity across the five studies. A publication bias was found in the analysis of current occasional drinking. However, the OR decreased after adjustment for the publication bias using the Duval and Tweedie trim and fill method (Online Resource 4).
Dose-response meta-analysis
We first assumed a linear-response model for the association between the amount of alcohol consumption and the risk of ONFH. The risk of ONFH increased by 35.3% for every 100 g/week (exp(b) = 1.353, p < 0.001) and by 44.1% for every 500 g drink-years (exp(b) = 1.441, p < 0.001) (Table 2). Then, we allowed departure from linearity by fitting a restricted cubic spline model. We found a statistically significant departure from linear association between alcohol intake and ONFH risk (Fig. 3). The non-linear dose-response trend showed a statistically significant increased risk of developing ONFH with increasing alcohol intake to 560 g/week (Table 3), and then the slope of risk slightly decreased with a concave downward pattern (Fig. 3a). The non-linear dose-response trend showed a statistically significant increased risk of developing ONFH with increasing number of total drinking years up to 2240 g drink-years (Table 3), and then the slope of risk slightly decreased (Fig. 3b) There was no publication bias across ORs (Online Resource 5).
Dose-response relations between alcohol intake and odds ratios for the osteonecrosis of the femoral head: a average and b total consumption. Data were modeled with fixed-effects restricted cubic spline models with four knots and using the Greenland and Longnecker method to estimate the covariances of multivariable-adjusted relative risks. Lines with long dashes represent the pointwise 95% confidence intervals for the fitted non-linear trend (solid line). Lines with short dashes represent the linear trend
Sensitivity analysis
The results of the sensitivity analysis, by excluding each one study from the pool of the five studies, were similar to the results of our overall analysis, and the dose-response relationship consistently showed a non-linear trend (Online Resource 6).
Discussion
Excessive alcohol intake has been known as the second leading risk factor for ONFH next to steroids [5]. Femoral head osteonecrosis remains as an intractable disease, and medical efforts regarding ONFH have mainly focused on treatment rather than prevention [24, 25]. The majority of clinicians still endeavor to warn the effect of alcohol on ONFH, but the exact relationship between dose and risk is not revealed yet. In our study, both current consumption and cumulative amount are positively associated with ONFH, showing a concave downward pattern.
Similar to the effects of corticosteroids, alcohol increases adipogenesis, which increases intraosseous pressure, causing a disruption of blood flow to the femoral head while inhibiting osteogenesis and angiogenesis [9]. In vitro studies showed that alcohol induces the differentiation of marrow stromal cells into adipocytes in a dose-dependent manner [26]. However, unlike the effect of steroids on stromal cells, alcohol-treated cells did not show increases in peroxisome proliferator–activated receptor-γ expression, which suggests that the exact molecular mechanisms may differ between these two important risk factors [27, 28].
Although steroid and alcohol are well-known risk factors, genetic predilections play important roles in the pathogenesis of ONFH. The proportion of patients with alcohol-related ONFH is higher in East Asian populations than Western. Aldehyde dehydrogenase 2 (ALDH2) is a key enzyme in alcohol metabolism that oxidizes acetaldehyde to non-toxic acetic acid. The enzyme is coded by the ALDH2 gene, which is commonly polymorphic in East Asian populations, with a prevalence of the inactive allele variant ALDH2*2 [29]. Those with inactive ALDH2 are likely to experience acetaldehydemia, which could lead to lipodystrophy [30]. Meanwhile, a protective effect of ALDH2 deficiency against alcohol addiction was reported because ALDH2 deficiency accumulates acetaldehyde, which induces an unpleasant feeling. The unpleasant feeling is a strong deterrent against heavy drinking and alcoholism [6].
In our study, regular (daily) drinkers had a higher risk for ONFH than occasional drinkers (OR, 5.90 versus 3.63). The disease involves an evolutionary process—if the duration of ischemia was temporary and shorter than the threshold for complete osteocytic death, the ischemic lesion does not progress to osteonecrosis [31]. A daily pattern of drinking seems to make fall a vicious cycle before fibrinolysis or reparative angiogenesis occurs [32]. Although the pattern measures have not been included in many alcohol-disease epidemiologic studies, not only volume of consumption but also patterns of drinking were found to be an additional influencing factor [33].
Our dose-response meta-analysis shows an ever-increasing pattern, that is, the higher the alcohol intake, the higher risk of ONFH. The risk of heart disease or stroke between alcohol intake has shown a J-shaped correlation (i.e., initially decreases, then steadily increases) [34,35,36]. The decreased risk of cardiovascular disease in light alcohol intake is associated with increased high-density lipoprotein cholesterol levels [37] or decreased plasma fibrinogen levels and platelet aggregation in low alcohol concentration [38]. However, the pathogenesis of ONFH is more multifactorial [5]. Besides hemostatic abnormalities, decreased bony turnover [10], adipocyte hypertrophy [39], and higher bone marrow pressure [40] contribute to the development of ONFH. A different pattern of correlation between alcohol intake and ONFH might result from the variability of underlying risk factors.
Steroid use can be a critical confounding factor when evaluating the effect of alcohol intake for ONFH. In this analysis, four studies had included patients without history of systemic corticosteroid use as selection criteria [7, 8, 12, 23]. One study investigated the possible interactions between alcohol intake and oral corticosteroid use [11]. However, no combined effect of alcohol intake and steroid use was observed, and there was no further increase in the OR of patients who had both alcohol intake and steroid use [11]. The added effect of alcohol intake was too small to make any significant difference in the presence of the overwhelming effect of steroids in the development of ONFH.
Although the estimated proportion of drinkers among ONFH patients is high, the reverse is not. The incidence of ONFH has been reported between 0.3 and 5.0% among patients who were treated for alcoholism [41, 42]. The role of an underlying genetic predisposition in the development of ONFH in these patients has not been fully elucidated but could explain why some chronic users of alcohol do not acquire the disease.
To date, no universal definition regarding alcohol-induced ONFH was established. In some studies, alcohol overuse was defined as consumption of pure alcohol >400 mL/week [43] or >400 mL/week for at least 6 months [44]. However, the risk of ONFH increased with even lower alcohol consumption in our analysis. The critical dose of alcohol necessary to induce ONFH remains unknown, and the determination of the proper dosage of alcohol is needed, in view of public health. Based on our analysis, clinicians could assess the risk of ONFH according to alcohol intake through a more detailed approach.
The limitations of our study are as follows. First, all case-control studies used to determine the factors associated with ONFH came from a single country (Japan). However, the development of ONFH cannot be tested in randomized experiments, and a case-control study is particularly suited for healthcare interventions of low incidence disease, and the study design and questionnaires used to obtain a detailed history of each subject were very similar between studies. Second, the ONFH can be influenced by many variables other than steroid use, such as underlying diseases, the use of anticoagulants, flushing pattern, history of liver diseases, and occupation. Thus, we have only used adjusted ORs, which were adjusted from several potential confounders that were comparable between studies (Table 1). Third, the OR can vary depending on the type of alcohol (liquid, wine, or beer), but it could not be evaluated in our analysis. Fourth, the size of ONFH is an important factor, but the relationship between size and alcohol intake could not be evaluated and also there was a lack of effort to contact the original authors.
Based on our meta-analysis, current drinking habit significantly increased the risk of ONFH and the risk was markedly pronounced among those who regularly drink. Moreover, the dose-response meta-analysis suggests that the risk of ONFH increased by 35.3% for every 100 g/week and by 44.1% for every 500 g drink-years. Future studies should focus on the cut-off value of alcohol consumption to prevent alcohol-induced ONFH.
References
Ohzono K, Saito M, Takaoka K, Ono K, Saito S, Nishina T, Kadowaki T (1991) Natural history of nontraumatic avascular necrosis of the femoral head. J Bone Joint Surg Br 73:68–72
Cui L, Zhuang Q, Lin J, Jin J, Zhang K, Cao L, Lin J et al (2016) Multicentric epidemiologic study on six thousand three hundred and ninety five cases of femoral head osteonecrosis in China. Int Orthop 40:267–276
Kang JS, Moon KH, Kwon DG, Shin BK, Woo MS (2013) The natural history of asymptomatic osteonecrosis of the femoral head. Int Orthop 37:379–384
Kang JS, Park S, Song JH, Jung YY, Cho MR, Rhyu KH (2009) Prevalence of osteonecrosis of the femoral head: a nationwide epidemiologic analysis in Korea. J Arthrop 24:1178–1183
Mont MA, Cherian JJ, Sierra RJ, Jones LC, Lieberman JR (2015) Nontraumatic osteonecrosis of the femoral head: where do we stand today? A ten-year update. J Bone Joint Surg Am 97(19):1604–1627
Chang JS, Hsiao JR, Chen CH (2017) ALDH2 polymorphism and alcohol-related cancers in Asians: a public health perspective. J Biomed Sci 24:19
Hirota Y, Hirohata T, Fukuda K, Mori M, Yanagawa H, Ohno Y, Sugioka Y (1993) Association of alcohol intake, cigarette smoking, and occupational status with the risk of idiopathic osteonecrosis of the femoral head. Am J Epidemiol 137:530–538
Matsuo K, Hirohata T, Sugioka Y, Ikeda M, Fukuda A (1988) Influence of alcohol intake, cigarette smoking, and occupational status on idiopathic osteonecrosis of the femoral head. Clin Orthop Relat Res 234:115–123
Chen X, Li M, Yan J, Liu T, Pan G, Yang H, Pei M et al (2017) Alcohol induces cellular senescence and impairs osteogenic potential in bone marrow-derived mesenchymal stem cells. Alcohol Alcohol:1–9
Wang Y, Li Y, Mao K, Li J, Cui Q, Wang GJ (2003) Alcohol-induced adipogenesis in bone and marrow: a possible mechanism for osteonecrosis. Clin Orthop Relat Res 410:213–224
Fukushima W, Yamamoto T, Takahashi S, Sakaguchi M, Kubo T, Iwamoto Y, Hirota Y, Idiopathic OMC-CS (2013) The effect of alcohol intake and the use of oral corticosteroids on the risk of idiopathic osteonecrosis of the femoral head: a case-control study in Japan. Bone Joint J 95-B:320–325
Sakata R (2003) A case-control study of association between life-style, alcohol dehydrogenase 2 and aldehyde dehydrogenase 2 genotype and idiopathic osteonecrosis of the femoral head. Kurume Med J 50(3–4):121–130
Orsini N, Li R, Wolk A, Khudyakov P, Spiegelman D (2012) Meta-analysis for linear and nonlinear dose-response relations: examples, an evaluation of approximations, and software. Am J Epidemiol 175:66–73
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D et al (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA 283(15):2008–2012
Guo KJ, Zhao FC, Guo Y, Li FL, Zhu L, Zheng W (2014) The influence of age, gender and treatment with steroids on the incidence of osteonecrosis of the femoral head during the management of severe acute respiratory syndrome: a retrospective study. Bone Joint J 96-B:259–262
Stang A (2010) Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25:603–605
Ades AE, Lu G, Higgins JP (2005) The interpretation of random-effects meta-analysis in decision models. Med Decis Mak 25:646–654
Orsini N, Bellocco R, Greenland S (2006) Generalized least squares for trend estimation of summarized dose–response data. Stata J 6:40–57
Greenland S, Longnecker MP (1992) Methods for trend estimation from summarized dose-response data, with applications to meta-analysis. Am J Epidemiol 135(11):1301–1309
Navarro-Compan V, Melguizo-Madrid E, Hernandez-Cruz B, Santos-Rey K, Leyva-Prado C, Gonzalez-Martin C, Navarro-Sarabia F et al (2013) Interaction between oxidative stress and smoking is associated with an increased risk of rheumatoid arthritis: a case-control study. Rheumatology (Oxford) 52:487–493
Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50:1088–1101
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315:629–634
Shibata A, Fukuda K, Inoue A, Higuchi F, Miyake H, Nishi M, Mori M et al (1996) Flushing pattern and idiopathic avascular necrosis of the femoral head. J Epidemiol 6:37–43
Amstutz HC, Le Duff MJ (2016) Hip resurfacing for osteonecrosis: two- to 18-year results of the conserve plus design and technique. Bone Joint J 98-B:901–909
Morita D, Hasegawa Y, Okura T, Osawa Y, Ishiguro N (2017) Long-term outcomes of transtrochanteric rotational osteotomy for non-traumatic osteonecrosis of the femoral head. Bone Joint J 99-B:175–183
Maurel DB, Boisseau N, Benhamou CL, Jaffre C (2012) Alcohol and bone: review of dose effects and mechanisms. Osteoporos Int 23:1–16
Seamon J, Keller T, Saleh J, Cui Q (2012) The pathogenesis of nontraumatic osteonecrosis. Arthritis 2012:601763
Ikemura S, Yamamoto T, Motomura G, Iwasaki K, Yamaguchi R, Zhao G, Iwamoto Y (2011) Lipid metabolism abnormalities in alcohol-treated rabbits: a morphometric and haematologic study comparing high and low alcohol doses. Int J Exp Pathol 92:290–295
Li H, Borinskaya S, Yoshimura K, Kal'ina N, Marusin A, Stepanov VA, Qin Z et al (2009) Refined geographic distribution of the oriental ALDH2*504Lys (nee 487Lys) variant. Ann Hum Genet 73(Pt 3):335–345
Zhang W, Zhong W, Sun X, Sun Q, Tan X, Li Q, Sun X et al (2015) Visceral white adipose tissue is susceptible to alcohol-induced lipodystrophy in rats: role of acetaldehyde. Alcohol Clin Exp Res 39:416–423
Mutijima E, De Maertelaer V, Deprez M, Malaise M, Hauzeur JP (2014) The apoptosis of osteoblasts and osteocytes in femoral head osteonecrosis: its specificity and its distribution. Clin Rheumatol 33(12):1791–1795
Koo KH, Mont MA, Jones LC (2014) Non-surgical treatment. In: Osteonecrosis, 2nd edn. Springer, Heidelberg, pp 240–273
Rehm J, Room R, Graham K, Monteiro M, Gmel G, Sempos CT (2003) The relationship of average volume of alcohol consumption and patterns of drinking to burden of disease: an overview. Addiction 98:1209–1228
Rimm EB, Klatsky A, Grobbee D, Stampfer MJ (1996) Review of moderate alcohol consumption and reduced risk of coronary heart disease: is the effect due to beer, wine, or spirits. BMJ 312:731–736
Larsson SC, Orsini N, Wolk A (2015) Alcohol consumption and risk of heart failure: a dose-response meta-analysis of prospective studies. Eur J Heart Fail 17:367–373
Mostofsky E, Chahal HS, Mukamal KJ, Rimm EB, Mittleman MA (2016) Alcohol and immediate risk of cardiovascular events: a systematic review and dose-response meta-analysis. Circulation 133(10):979–987
Thornton J, Symes C, Heaton K (1983) Moderate alcohol intake reduces bile cholesterol saturation and raises HDL cholesterol. Lancet 2:819–822
Ridker PM, Vaughan DE, Stampfer MJ, Glynn RJ, Hennekens CH (1994) Association of moderate alcohol consumption and plasma concentration of endogenous tissue-type plasminogen activator. JAMA 272(12):929–933
Sheng H, Sheng CJ, Cheng XY, Zhang G, Lee KM, Leung KS, Qu S et al (2013) Pathomorphological changes of bone marrow adipocytes in process of steroid-associated osteonecrosis. Int J Clin Exp Pathol 6:1046–1050
Powell C, Chang C, Gershwin ME (2011) Current concepts on the pathogenesis and natural history of steroid-induced osteonecrosis. Clin Rev Allergy Immunol 41:102–113
Gold EW, Cangemi PJ (1979) Incidence and pathogenesis of alcohol-induced osteonecrosis of the femoral head. Clin Orthop Relat Res 143:222–226
Orlic D, Jovanovic S, Anticevic D, Zecevic J (1990) Frequency of idiopathic aseptic necrosis in medically treated alcoholics. Int Orthop 14:383–386
Chen CC, Lin CL, Chen WC, Shih HN, Ueng SW, Lee MS (2009) Vascularized iliac bone-grafting for osteonecrosis with segmental collapse of the femoral head. J Bone Joint Surg Am 91(10):2390–2394
Chen CH, Chang JK, Lai KA, Hou SM, Chang CH, Wang GJ (2012) Alendronate in the prevention of collapse of the femoral head in nontraumatic osteonecrosis: a two-year multicenter, prospective, randomized, double-blind, placebo-controlled study. Arthritis Rheum 64:1572–1578
Acknowledgments
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
None.
Source of funding
No external funding was received in support of this work.
Electronic supplementary material
Online Resource 1
MOOSE checklist for meta-analyses of observational studies. (DOCX 22 kb)
Online Resource 2
The search strategy that details the searching process of relevant clinical study selection. (DOCX 207 kb)
Online Resource 3
Methodological quality assessment of included studies measured by Newcastle-Ottawa Scale (DOCX 16 kb)
Online Resource 4
Overall statistics for publication bias analysis among included studies. (DOCX 18 kb)

Online Resource 5
Funnel plot of the association between alcohol intake and the risk of osteonecrosis of the femoral head. (A) Alcohol intake and drinking habit (former and occasional drinking). (B) Alcohol intake and drinking habit (former and regular drinking). (C) Alcohol intake and average alcohol intake. (D) Alcohol intake and cumulative alcohol intake. (JPEG 73 kb)
Online Resource 6
Sensitivity analysis by excluding one study at the time for overall odds ratio. (DOCX 18 kb)
Rights and permissions
About this article
Cite this article
Yoon, BH., Kim, Ty., Shin, IS. et al. Alcohol intake and the risk of osteonecrosis of the femoral head in Japanese populations: a dose-response meta-analysis of case-control studies. Clin Rheumatol 36, 2517–2524 (2017). https://doi.org/10.1007/s10067-017-3740-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-017-3740-4