Abstract
Some evidences suggest that obesity impairs the effectiveness of TNF inhibitors. We examined the impact of body mass index (BMI) on the clinical effectiveness of abatacept in rheumatoid arthritis (RA) patients. This is a pooled analysis of 10 prospective cohorts of RA patients. All patients with available BMI were included in this study. The primary endpoint was drug retention of abatacept in the different BMI categories. Multivariable Cox regression was used to estimate hazard ratios (HRs) for drug discontinuation. A secondary endpoint was EULAR/LUNDEX response rates at 6/12 months. Of the 2015 RA patients initiating therapy with IV abatacept, 380 (18.9%) were classified as obese. Obese patients had more functional disability, and were less often RF positive. The median abatacept retention time was 1.91 years for obese RA patients compared to 2.12 years for non-obese patients (p = 0.15). The risk of abatacept discontinuation was not significantly different for overweight (HR 1.03 (95% CI 0.89–1.19)), or for obese (HR 1.08 (95% CI 0.89–1.30)) compared to normal-weight patients. Rheumatoid factor positivity reduced the risk of abatacept discontinuation (HR 0.83 (95% CI 0.72–0.95)), while previous biologic therapy was positively associated with drug interruption (HRs increasing from 1.68 to 2.16 with the line of treatments). Obese and non-obese patients attained similar rates of EULAR/LUNDEX clinical response at 6/12 months. Drug retention and clinical response rates to abatacept do not seem to be decreased by obesity in RA patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A growing body of research suggests a strong association between body mass index (BMI) and development of rheumatoid arthritis (RA). Recently, a large prospective analysis of US nurses found that obesity increased the risk of developing RA by 40–70% depending on age and serological status [1]. Obesity has been reported to be associated with the risk of developing RA, particularly among women diagnosed with RA at earlier ages [1], with higher disease activity in early RA patients [2], and with worse function in early arthritis [3–6]. However, the pathogenic link between obesity and RA is not fully understood and, to some extent, controversial [7]. For example, a recent study reported a negative association between obesity and RA in men [8].
Obesity is nowadays regarded as the cause of mild inflammation associated with an overexpression of pro-inflammatory cytokines and adipokines produced by adipocytes predominately in the visceral fat [9]. Adipose tissue synthetizes an array of adipokines, such as leptin, visfatin, resistin, chemerin, and adiponectin which have direct effects on cartilage, bone, and synovial tissues metabolism [9, 10]. Comorbid obesity has also been associated with a decreased probability of joint damage progression in anti-citrullinated peptide antibody (ACPA-) positive RA patients [3–5]. This paradox has been explained by an unbalanced ratio of leptin/adiponectin in obese subjects. Adiponectin has a negative effect on bone metabolism mediated by the activation of osteoclasts, and its decrease in obesity may explain the less erosive course in RA patients with high BMI [11]. Obesity may also impact the response to anti-rheumatic treatments. Prospective trials and observational studies have provided evidence that RA patients with higher BMI tend to have less favourable responses to conventional disease modifying anti-rheumatic drugs (DMARDs), as well as to anti-tumour necrosis factor (anti-TNF) agents [12–17]. Recently, a cohort study has shown that high BMI also impacts the clinical response to a second biological DMARD (bDMARD), mainly rituximab, in RA patients with inadequate response to a first anti-TNF drug [18]. Abatacept, a CTLA4-IgG fusion protein that inhibits T cell activation by blocking CD28/CD80 co-stimulation, has never been specifically evaluated in RA patients with high BMI. The aim of this article was to examine the impact of obesity on the effectiveness of abatacept in the real-world setting. Furthermore, we intended a priori to compare our results with another observational study, the ACTION study [19], and to aggregate key results, in order to examine the impact of obesity in a larger population of RA patients on abatacept and increase our statistical power.
Patients and methods
The “pan-European registry collaboration for abatacept” (PANABA) is a collaborative project involving 10 national RA registries from Europe (Czech Republic, Denmark, France, Italy, Norway, Portugal, Spain, Sweden, Switzerland), and from Canada with longitudinal data of RA patients initiating abatacept treatment in routine settings [20]. These registries have been described in detail elsewhere and a detailed discussion of their enrolment strategies, similarities, and differences is beyond the scope of this paper [21]. Ethical approval was obtained for all the registries, and patients were recruited after giving their written informed consent in accordance with the Declaration of Helsinki, except in Denmark where registry research does not require ethical approval or informed consent. Abatacept was administered intravenously in the time frame of this analysis, following the indications of drug approval, 500 mg < 60 kg body weight, 750 mg >60 < 100 kg body weight, and 1000 mg >100 kg body weight.
At initiation of abatacept (baseline visit), data to be recorded were the following: age, gender, weight, height, disease duration, concomitant use of disease modifying anti-rheumatic drugs (DMARDs), health assessment questionnaire (HAQ) score, and Disease Activity Score in 28 joints (DAS28). During follow-up, either at predetermined or at open time-points after abatacept initiation, registries further provided information on subsequent DAS28 scores, co-medication with DMARDs, and abatacept maintenance or discontinuation.
The predictor of interest for this analysis was BMI at abatacept initiation. Weight and height at baseline were either self-reported or assessed by the treating physician, and BMI was calculated as weight in kilogrammes divided by the square of height in metres (kg/m2). However, baseline BMI was available only for 34.3% of RA patients in the whole cohort, as height was not collected systematically in all registries. According to the WHO classification of BMI classes, patients were classified into underweight/normal-weight (BMI <25.0 kg/m2), overweight (25.0 kg/m2 ≤ BMI <30 kg/m2), obese (30.0 kg/m2 ≤ BMI <35 kg/m2), and severely obese (BMI ≥35.0 kg/m2). As underweight subjects were very few (n = 31), they were grouped with normal weight patients. The primary outcome for this analysis was abatacept drug retention. A secondary endpoint was the achievement of EULAR moderate/good clinical response [22], as crude value and adjusted for drug retention (Lundex index). The Lundex is calculated as the fraction of patients adhering to therapy multiplied by the fraction of patients achieving the EULAR moderate/good response [23] at 6 and 12 months.
The ACTION (AbataCepT In rOutiNe clinical practice) study is a 2-year prospective, multicentre, observational cohort study initiated by a pharmaceutical company (BMS) that enrolled patients with RA in Europe and Canada to evaluate the tolerance and the effectiveness of abatacept therapy in routine clinical practice [19].
Statistical analysis
We analysed patient demographics and disease characteristics at treatment initiation using standard descriptive statistics. Patients lost to follow up, or patients who stopped therapy due to reasons deemed unrelated to abatacept (pregnancy, relocation or other) were right censored. Time to discontinuation was defined as the time between abatacept initiation and last administration plus 1 month (dispensation interval). We computed abatacept drug retention rate using Kaplan–Meyer (K–M) estimator and compared differences across BMI classes using the log-rank test. We estimated HRs for each BMI category by performing a multivariate Cox regression, adjusting for patient demographics (age, gender), disease characteristics (rheumatoid factor (RF) (pos/neg), DAS28 at baseline, disease duration), and treatment characteristics (number of prior bDMARDs, calendar year of abatacept initiation). To evaluate rates of moderate/good EULAR responders at 6 and 12 months visit, a time-window ± 1.5 month around visit was used. To compute 95% confidence intervals (95% CI), we used bootstrap distributions. To improve the precision of the confidence interval estimation around the HRs, we pooled the HRs obtained in this study with the HRs obtained in the ACTION study [24], performing a meta-analysis with inverse variance method.
Results
PANABA data
Of the 2015 RA patients with available BMI, 380 (18.9%) were obese with a BMI ≥ 30. At baseline, disease activity, according to DAS28, was not significantly different among the BMI classes, and the number of biological drugs prior to abatacept therapy was also similar. In contrast, obese patients had higher disability as measured by the HAQ, shorter disease duration, and were less often RF positive (Table 1).
We found no statistically significant difference in abatacept drug retention across BMI classes (log rank test, p = 0.79, Fig. 1). Median survival time was 2.12 years for underweight/normal-weight, 2.12 years for overweight, 1.91 years for obese, and 2.44 years for severely obese patients. The survival rates at 2 years for treatment interruption due to any reason were 52.8% (95% CI, 49.4%–56.5%), 51.8% (95% CI, 47.4%–56.6%), 48.3% (95% CI, 41.9%–55.6%), and 55.2% (95% CI, 45.6%–66.3%), for RA patients with under/normal-weight, overweight, obesity, and severe obesity RA. Furthermore, we detected no significant differences when focusing only on abatacept discontinuation for ineffectiveness (log rank test, p = 0.36, Fig. 2) or for adverse events (log rank test, p = 0.28). As PANABA is a combination of national registries, we assessed a possible country effect of BMI on drug retention, but a significant difference across registries was found (p = 0.34). In the multivariable adjusted analysis, higher BMI categories were also not associated with increased HRs to discontinue abatacept treatment. Specific disease characteristics were associated with abatacept retention (Table 2). RF positive patients were less likely to stop abatacept, while higher DAS28 at baseline and number of past bDMARD failures were associated with higher risk of drug discontinuation.
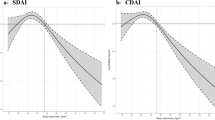
Response to therapy was assessed by EULAR and Lundex-adjusted clinical responses rates at 6 and 12 months. The moderate or good EULAR response rates were similar across BMI categories at 6 months (p = 0.74) and at 12 months (p = 0.49) (Fig. 3). At 6 months, the Lundex (EULAR response adjusted for drug retention) moderate or good response was 39.8% for underweight/normal-weight patients, 42.9% for overweight patients (Lundex difference normal-overweight = 3.1%, 95% CI: [−0.3; 0.10]), 40.0% for obese patients (Lundex difference normal-obesity = 0.20%, 95% CI: [−0.08; 0.08]), and 49.4% for severely obese patients (Lundex difference normal-severe = 9.6%, 95% CI: [−0.04; 0.23]). The pattern of results was similar at 12 months, the Lundex moderate or good EULAR response was 37.3, 41.1, 37.7, and 51.3% for underweight/normal-weight, obese, and severely obese patients, respectively.
ACTION data
Similar results have been also reported in abstract form in a recent sub-analysis of the ACTION study [24]. They investigated 936 RA patients, including 253 obese or severe obese patients, starting intravenously abatacept after failure of at least one anti-TNF. The drug survival rates at 2 years were similar to our study without significant differences among BMI classes (underweight/normal weight 53.8%, overweight 57.4%, obese 50.5%, severe obese 53.2%). To increase the statistical power and the precision of our results, we combined estimates from the PANABA collaboration and the ACTION study. In this large population including a total of 2951 patients (633 with obesity and 198 with severe obesity), BMI did not significantly influence the persistence on abatacept therapy (Table 3).
Discussion
We analysed data of 2015 RA patients (380 with obesity) treated with abatacept from 10 large worldwide cohorts and found no evidence that obese or severe obese patients had lower drug retention on abatacept than normal-weight patients. Treatment interruption for ineffectiveness was not increased in obese patients, suggesting that abatacept is effective in controlling disease activity regardless of BMI. In the adjusted model, drug discontinuation remained unassociated with BMI categories. However, as expected, the number of past biologics was significantly associated with drug discontinuation. Number of past biologics showed a monotonic increase in HR, so that the greater the number of past biologics failure, the higher the hazard of discontinuing abatacept, probably reflecting a progressive patient selection. Of note, RF positive patients were significantly less likely to stop abatacept (estimated risk reduction 17%), as previously reported for abatacep [25], and also for rituximab [26]. Combining HRs of abatacept discontinuation from ACTION and PANABA to increase the statistical power, we confirmed that obesity and severe obesity did not negatively impact the persistence of abatacept treatment.
Previous studies have consistently demonstrated that high BMI negatively affects the clinical response to anti-TNF drugs in RA patients, namely to adalimumab, etanercept, and infliximab [13, 15]. Klaasen et al. [15], have prospectively studied 15 obese patients with RA receiving infliximab, and found a good EULAR response at 16 weeks significantly lower in obese than in normal-weight/underweight patients. Gremese et al. [13] have shown that 66 RA patients with obesity achieved less frequently DAS28-steered remission than normal-weight patients following anti-TNF treatment at 12 months. More recently, it has been shown that 66 obese patients on first ever TNF blocker had a median drug survival time (48 months) shorter than normal-weight patients (60 months), and that the HR to discontinue the therapy was 50% higher in obese than normal-weight patients [18]. Additionally, an impaired clinical response to conventional DMARDs in obese RA patients has been also reported [12, 14, 17], suggesting that RA in these patients is peculiar and intrinsically poorly responsive to treatments.
A clinically important question is thus whether biological drugs other than anti-TNF can be effective in obese RA patients. This was the aim of a recent study [18] showing that 24 obese RA patients starting non-anti-TNF drugs (mainly rituximab), after failure of a first TNF inhibitor, still had a poor clinical response. On the contrary, EULAR based clinical responses were not impaired at 6 months in 35 RA obese patients on treatment with rituximab [27]. Furthermore, two recent retrospective analyses have suggested that rate of EULAR clinical response to tocilizumab in RA patients was not influenced by high BMI [28, 29]. However, available studies have small sample sizes and limited follow-up, and therefore additional data are needed to confirm these preliminary findings.
Additionally, we have shown that rates of RA patients attaining a moderate/good EULAR/LUNDEX response at 6 and 12 months were similar across BMI categories, further confirming that obesity does not seem to influence abatacept effectiveness. It could be argued that joint assessment may be difficult in obese RA patients, thus affecting the evaluation of clinical response, but, in the APPRAISE study, a prospective multinational study using power Doppler ultrasonography (PDUS) to assess early signs of response to abatacept, PDUS scores did also not significantly differ at 6 months among BMI categories [30]. Recently, similar findings have been reported in a small cohort of RA patients, and no difference in EULAR good response across BMI categories (39 obese) after 6 months of treatment with ABA was found [31].
The reason why abatacept does not seem to be impacted by obesity, unlike TNF inhibitors, is unclear and can currently be only a matter of speculations. It can be argued that in our study IV administration per body weight of abatacept may have nullified difference among BMI categories, but infliximab, despite weight-adjusted dosing, is less effective in obese patients [15]. Difference in pharmacokinetics could be taken into account. Indeed, dose-finding studies on sc abatacept have shown that Cminss values were similar in both weight-tiered and flat dosing across BMI categories. For IV abatacept, the standard weight-tiered regimen enables >90% of patients to achieve therapeutic Cminss exposures even at the highest body mass. Elimination of abatacept from the systemic circulation follows first order kinetics regardless of the route of administration. The absorption kinetics for IV administration occurs through a zero order process [32, 33]. Pharmacokinetics data for other current bDMARDs, including anti-TNF drugs, in obese RA patients are lacking. Possible difference in drug compartment distribution based on the lipophilic property of the drug may be only matter of speculation at the moment. Maybe an explanation should be searched in the visceral fat milieu that might generate a state of resistance or neutralization of TNF blocking agents, without affecting the inhibition of dual signalling, CD3/TCR-CD28/CD80, by abatacept. Data on other non-TNF bDMARDs are less extensive and need further investigations. Furthermore, BMI is a rather crude indicator of metabolic status, and investigations using other measures may shed light on the relation between body fat and response to bDMARDs.
Some strengths and limitations of our study must be emphasized. PANABA is a collaborative study of several RA registries across Europe and North America, and country differences in RA patients and rheumatologist behaviour are conceivable. We tested for effect modification by country and have not found any indication that obesity affected abatacept retention differently in specific countries. BMI was available in only 34% of all patients; however, BMI data were missing at random and this information should not be related to the outcome, and thus not cause bias. The ACTION study had a different setting, as a sponsor-initiated observational study and found similar results, supporting the generalizability of our findings. However, in both studies, almost all RA patients were not responders to previous anti-TNF drugs, thus, information on obese patients naïve to biologics is still missing, and further analysis with abatacept as first bDMARD should be considered. Of note, preliminary findings from a recent sub-analysis of ACTION have shown that short-term (6 months) drug retention of abatacept was not influenced by BMI in biologic naïve patients [34]. The main strength of this study is to analyse a very large prospective cohort of RA patients with BMI (over 2000), evaluating the greatest number of obese, and even severe obese, subjects.
As current treatment guidelines suggest that comorbidities should be taken into account in therapeutic decision making [35], the availability of bDMARDs that are not affected by BMI may aid clinicians in their strategy of treatment of RA patients with obesity. This analysis of real-world RA patients demonstrates that IV abatacept maintenance and effectiveness were not negatively influenced by obesity, which is a clinically useful information for some patients.
References
Lu B, Hiraki LT, Sparks JA, Malspeis S, Chen CY, Awosogba JA et al (2014) Being overweight or obese and risk of developing rheumatoid arthritis among women: a prospective cohort study. Ann Rheum Dis 73:1914–1922
Ajeganova S, Andersson ML, Hafström I, BARFOT Study Group (2013) Association of obesity with worse disease severity in rheumatoid arthritis as well as with comorbidities: a long-term followup from disease onset. Arthritis Care Res (Hoboken) 65:78–87
Baker JF, Ostergaard M, George M, Shults J, Emery P, Baker DG, Conaghan PG (2014) Greater body mass independently predicts less radiographic progression on X-ray and MRI over 1-2 years. Ann Rheum Dis 73:1923–1928
van der Helm-van Mil AH, van der Kooij SM, Allaart CF, Toes RE, Huizinga TW (2008) A high body mass index has a protective effect on the amount of joint destruction in small joints in early rheumatoid arthritis. Ann Rheum Dis 67:769–774
Westhoff G, Rau R, Zink A (2007) Radiographic joint damage in early rheumatoid arthritis is highly dependent on body mass index. Arthritis Rheum 56:3575–3582
Humphreys JH, Verstappen SM, Mirjafari H, Bunn D, Lunt M, Bruce IN, Symmons DP (2013) Association of morbid obesity with disability in early inflammatory polyarthritis: results from the Norfolk arthritis register. Arthritis Care Res (Hoboken) 65:122–126
Finckh A, Turesson C (2014) The impact of obesity on the development and progression of rheumatoid arthritis. Ann Rheum Dis 73:1911–1913
Turesson C, Bergström U, Pikwer M, Nilsson JÅ, Jacobsson LT (2016) A high body mass index is associated with reduced risk of rheumatoid arthritis in men, but not in women. Rheumatology (Oxford) 55:307–314
Iannone F, Lapadula G (2010) Obesity and inflammation—targets for OA therapy. Curr Drug Targets 11:586–598
Iannone F, Lapadula G (2011) Chemerin/ChemR23 pathway: a system beyond chemokines. Arthritis Res Ther 13:104
Wang QP, Li XP, Wang M, Zhao LL, Li H, Xie H, Lu ZY (2014) Adiponectin exerts its negative effect on bone metabolism via OPG/RANKL pathway: an in vivo study. Endocrine 47:845–853
Ellerby N, Mattey DL, Packham J, Dawes P, Hider SL (2014) Obesity and comorbidity are independently associated with a failure to achieve remission in patients with established rheumatoid arthritis. Ann Rheum Dis 73:74
Gremese E, Carletto A, Padovan M, Atzeni F, Raffeiner B, Giardina AR et al (2013) Obesity and reduction of the response rate to anti-tumor necrosis factor α in rheumatoid arthritis: an approach to a personalized medicine. Arthritis Care Res (Hoboken) 65:94–100
Heimans L, van den Broek M, le Cessie S, Siegerink B, Riyazi N, Han KH et al (2013) Association of high body mass index with decreased treatment response to combination therapy in recent-onset rheumatoid arthritis patients. Arthritis Care Res (Hoboken) 65:1235–1242
Klaasen R, Wijbrandts CA, Gerlag DM, Tak PP (2011) Body mass index and clinical response to infliximab in rheumatoid arthritis. Arthritis Rheum 63:359–364
Rodrigues AM, Reis JE, Santos C, Pereira MP, Loureiro C, Martins F et al (2014) A1.1 obesity is a risk factor for worse treatment response in rheumatoid arthritis patients—results from reuma.pt. Ann Rheum Dis 73(Suppl 1):A1
Sandberg ME, Bengtsson C, Källberg H, Wesley A, Klareskog L, Alfredsson L, Saevarsdottir S (2014) Overweight decreases the chance of achieving good response and low disease activity in early rheumatoid arthritis. Ann Rheum Dis 73:2029–2033
Iannone F, Fanizzi R, Notarnicola A, Scioscia C, Anelli MG, Lapadula G (2015) Obesity reduces the drug survival of second line biological drugs following a first TNF-α inhibitor in rheumatoid arthritis patients. Joint Bone Spine
Nüßlein HG, Alten R, Galeazzi M, Lorenz HM, Boumpas D, Nurmohamed MT et al (2014) Real-world effectiveness of abatacept for rheumatoid arthritis treatment in European and Canadian populations: a 6-month interim analysis of the 2-year, observational, prospective ACTION study. BMC Musculoskelet Disord 15:14
Finckh, Neto, Iannone, Loza, Lie, van Riel et al. (2015) The impact of patient heterogeneity and socioeconomic factors on abatacept retention in rheumatoid arthritis across nine European countries. RMD Open 1. doi:10.1136/rmdopen
Kearsley-Fleet L, Závada J, Hetland ML, Nordström DC, Aaltonen KJ, Listing J et al (2015) The EULAR Study Group for Registers and Observational Drug Studies: comparability of the patient case mix in the European biologic disease modifying anti-rheumatic drug registers. Rheumatology (Oxford) 54:1074–1079
Fransen J, van Riel PL (2009) The disease activity score and the EULAR response criteria. Rheum Dis Clin N Am 35:745–757 vii-viii
Kristensen LE, Saxne T, Geborek P (2006) The LUNDEX, a new index of drug efficacy in clinical practice: results of a five-year observational study of treatment with infliximab and etanercept among rheumatoid arthritis patients in southern Sweden. Arthritis Rheum 54:600–606
Nüßlein H, Alten R, Galeazzi M, Lorenz HM, Nurmohame MT, Bensen WG, Burmester G (2014) Does body mass index impact long-term retention with abatacept in patients with RA who have received at least one prior biologic agent. 2-year results from a real-world, international, prospective study. Arthritis Rheum 66S:2492
Gottenberg JE, Courvoisier DS, Hernandez MV, Iannone F, Lie E, Canhão H et al. (2016) Rheumatoid factor and anti-citrullinated protein antibody positivity are associated with a better effectiveness of abatacept: results from the Pan-European registry analysis. Arthritis Rheumatol
De Keyser F, Hoffman I, Durez P, Kaiser MJ, Westhovens R, MIRA Study Group (2014) Longterm followup of rituximab therapy in patients with rheumatoid arthritis: results from the Belgian MabThera in rheumatoid arthritis registry. J Rheumatol 41:1761–1765
Ottaviani S, Gardette A, Roy C, Tubach F, Gill G, Palazzo E et al (2015) Body mass index and response to rituximab in rheumatoid arthritis. Joint Bone Spine 82:432–436
Pers YM, Godfrin-Valnet M, Lambert J, Fortunet C, Constant E, Mura T et al (2015) Response to tocilizumab in rheumatoid arthritis is not influenced by the body mass index of the patient. J Rheumatol 42:580–584
Gardette A, Ottaviani S, Sellam J, Berenbaum F, Lioté F, Meyer A et al. (2016) Body mass index and response to tocilizumab in rheumatoid arthritis: a real life study. Clin Rheumatol
D'Agostino MA, Le Bars M, Taylor M, Chou B, Zhu J, Ranganath VK (2015) In patients with rheumatoid arthritis and an inadequate response to methotrexate, does body mass index influence the efficacy of abatacept on inflammation when measured by power doppler ultrasonography? Results from the APPRAISE study. Ann Rheum Dis 74S2:231
Gardette A, Ottaviani S, Sellam J, Berenbaum F, Lioté F, Fautrel B et al. (2016) Body mass index and response to abatacept in rheumatoid arthritis. Eur J Clin Invest
Corbo, Valencia, Raymond, Agrawal, Townsend, Zhou et al (2009) Subcutaneous administration of abatacept in patients with rheumatoid arthritis: pharmacokinetics, safety and immunogenicity. Ann Rheum Dis 68(S3):574
Roy A, Mould DR, Wang XF, Tay L, Raymond R, Pfister M (2007) Modeling and simulation of abatacept exposure and interleukin-6 response in support of recommended doses for rheumatoid arthritis. J Clin Pharmacol 47:1408–1420
Alten R, Nublein HG, Galeazzi M, Lorenz H-M, Mariette X, Cantagrel A et al (2015) Body mass index does not influence the efficacy of abatacept in patients with RA who are biologic Naïve: 6-month results from a real-world, international, prospective study. Arthritis Rheum 67S:553
Smolen JS, Landewé R, Breedveld FC, Buch M, Burmester G, Dougados M et al (2014) EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2013 update. Ann Rheum Dis 73:492–509
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
None.
Funding
The study was supported by an unrestricted research grant from Bristol–Myers Squibb (BMS). BMS had no role in the interpretation of the data nor in the decision to publish or not the results.
Rights and permissions
About this article
Cite this article
Iannone, F., Courvoisier, D.S., Gottenberg, J.E. et al. Body mass does not impact the clinical response to intravenous abatacept in patients with rheumatoid arthritis. Analysis from the “pan-European registry collaboration for abatacept (PANABA). Clin Rheumatol 36, 773–779 (2017). https://doi.org/10.1007/s10067-016-3505-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-016-3505-5