Abstract
The authors aimed to test potential relations between osteoarthritis (OA) features, disability and health-related quality of life (HR-QoL) at different body locations. Outpatients consulting for pain associated to self-reported OA at varied healthcare settings were evaluated in a 3-month observational non-controlled follow-up study. Socio-demographic/anthropometric and medical data were collected at three time points. Lequesne’s indices, quick-disabilities of arm, shoulder and hand (DASH) and Oswestry questionnaires provided measures of physical function and disability. HR-QoL measures were obtained with EuroQol-5 Dimensions. Multivariate analyses were used to evaluate the differences of pain severity across body regions and the correlates of disability and HR-QoL. Six thousand patients were evaluated. Pain lasted 2 years or more in 3995 patients. The mean pain severity at baseline was moderate (6.4 points). On average, patients had pain in 1.9 joints/areas. The pain was more severe when OA involved the spine or all body regions. Pain severity explained much of the variance in disability and HR-QoL; this association was less relevant in patients with OA in the upper limbs. There were considerable improvements at follow up. Pain severity improved as did disability, which showed particularly strong associations with HR-QoL improvements. Pain severity is associated with functional limitations, disability and poor HR-QoL in patients with self-reported OA. Functional limitations might have particular relevance when OA affects the upper limbs. Improvements are feasible in many patients who consult because of their pain.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Traditionally, musculoskeletal conditions have received less epidemiologic attention than have other chronic diseases because they are non-fatal. Recently, this notion has begun to change, in part because musculoskeletal conditions—and osteoarthritis (OA) in particular—are long-lasting, highly prevalent and disabling [1, 2]. It has been suggested that in general, the disability associated with potentially fatal conditions (such as ischemic heart disease, diabetes mellitus or cancer) is decreasing, while the disability associated with OA or other musculoskeletal conditions is increasing [3]. According to the Global Burden of Disease study 2010, hip or knee OA is one of the leading causes of global disability [4] and low-back pain was shown to cause more years lived with disability than do any other condition [5]. Furthermore, OA [6] and other musculoskeletal disorders [7] have also been shown to be associated with increased mortality.
Pain and disability are considered to be the most important domains in order to assess the health impact on individuals with OA [4, 7]. Chronic joint pain can produce fatigue and disability and reduce the health-related quality of life (HR-QoL) of patients with OA [8, 9]. Because OA pain is chronic, it has profound effects on physical and psychological functioning. Cognitive, psychosocial factors and coping strategies are major determinants of functional outcomes in patients with chronic pain [10, 11]. Current measures of HR-QoL that provide a comprehensive, multidimensional subjective evaluation of patients’ perspective of their health status constitute a good complement to functional measures for assessing the burden associated with chronic OA pain [12].
Many cross-sectional and some longitudinal studies have evaluated how chronic OA pain associates with physical function limitations and disability. However, most studies of OA pain and disability have focused mainly on specific conditions, particularly knee and hip OA [13], and they neither provide an overall view of OA nor permit comparisons between different OA locations. The current conceptual view of OA is that of an aggregate of related conditions that share a common pathology resulting from a reaction of synovial joints to injury, but with varying clinical manifestations, chiefly pain, joint stiffness, loss of function and outcomes [7]. There is great variability in the importance of risk factors, clinical presentation and outcomes both between patients and at different joint sites [2]; yet, to the knowledge of authors, no adequately powered study has compared the burden of OA between body regions to date.
The use of self-reported OA can be a less costly but suitable alternative to clinical or radiographic OA to evaluate OA outcomes in large community and epidemiologic studies [14]. In this study, the authors recruited patients based on their pain and self-reported OA, but a set of objective criteria was used to increase the certainty that the most likely cause of pain was OA. The primary aim was to test potential relationships of patients and OA features such as age, gender, comorbidities, site of OA, time since pain onset, pain severity and interference with disability and HR-QoL in patients suffering pain associated with OA at any location. Secondarily, pain severity was compared across different OA locations. For these purposes, a large sample of patients with painful OA in the spine or the extremities was recruited from outpatient facilities in a variety of medical specialties.
Materials and methods
Design and patients
This was a non-controlled observational follow-up study. The source population consisted of all individuals consulting for chronic (three or more months since onset) moderate to severe pain (≥4 on a 0–10 numerical rating scale on pain severity) of probable osteoarthritic origin at outpatient facilities in Spain. The study period spanned from January to August 2013. An invitation to participate was sent to a convenience sample of specialists from pain clinics, anaesthesiology, orthopaedic surgery, rehabilitation, rheumatology, neurology, neurosurgery, internal medicine, geriatrics or primary care settings to cover as much of the medical settings that provide care for OA as possible. They were instructed to systematically propose participation to consecutive eligible patients (see below).
To qualify as osteoarthritic, pain had to be non-traumatic, affect either hands, elbows, shoulders, hips, knees, feet or spine, it also had to be persistent, worsen with use and for non-spinal pain, be accompanied by transient (≤30 min) morning stiffness or stiffness after prolonged rest. Spinal conditions of infectious, metabolic or neoplastic origin were discarded. The presence of crepitus, bone swelling or radiological anomalies was not required, yet patients had to report an OA diagnosis in the past. Another requirement was that the current encounter was the first time the patient approached the investigator’s desk, and the reason had to be osteoarthritic pain. Patients with any surgery scheduled within the next 3 months were excluded.
Assessments and procedures
Sociodemographic and anthropometric data, including gender, age, weight, height, nationality and professional status was collected. The referring physician, the treating physician, level of physical activity (none/light/moderate/vigorous), smoking status and the presence of some common chronic medical comorbidities (hypertension, cardiovascular conditions, diabetes mellitus, depression/anxiety, hyperthyroidism, hypothyroidism, respiratory diseases, prostatic conditions, osteoporosis, other) were also recorded. Clinical data pertaining to OA included the age band at diagnosis (<45 years, 45–54 years, 55–64 years, 65–74 years and >75 years), the time since pain onset, the region of the body affected (upper limbs, lower limbs, spine), the joint(s) with the most severe pain (by questioning patients) and, based on filed medical data, the OA aetiology (primary/idiopathic or secondary).
Validated clinical tools were used to obtain measures of pain severity and interference, physical function, OA-related disability and HR-QoL during face-to-face interviews. The Brief Pain Inventory (BPI) [15], which has been validated in non-cancer patients in Spain [16], was used to obtain measures of pain severity and interference with daily activities. HR-QoL measures were obtained with the EuroQol-5 Dimensions (EQ-5D) with three levels of response [17, 18], a generic, multi-attribute and preference-based instrument. It provides one measure based on relative utility weights, [19] regarded here as the EQ-5D index, and one global measure of well-being elicited directly from the patient over a visual analogue scale (VAS). OA-specific instruments for measuring physical function and disability (understood as the ability to perform certain tasks and roles) were used as well. These included the abridged version of the Disabilities of Arm, Shoulder and Hand (quick-DASH) [20], the algo-functional Lequesne’s Indices [21, 22] and the Oswestry Disability Questionnaire [23] (version 2.0, replacing miles with kilometres), which were administered to patients with OA in the upper limbs, lower limbs and spine, respectively.
Patients were assessed again 1 and 3 months after the initial visit. The BPI, EQ-5D and the OA-specific tools for measuring functioning and disability were administered again, together with scales reporting patients’ satisfaction and expectations. These assessments were made during routine follow-up clinical visits. Thus, a low drop-out rate was expected.
Analysis of data
All analyses were done over available data; missing data were not imputed. Descriptive methods were used to summarize all data. Three non-mutually exclusive subgroups were defined, comprising patients who had at least one painful joint in any of the following major body regions: upper limbs, lower limbs and spine. Because each of these subgroups had a specific score on disability, separate descriptions and inferences were done for each of them. To assess whether pain severity was different across body regions or whether it varied depending on the number of symptomatic regions, the scores of pain severity were regressed linearly over weighted effect-coded variables that indicated the region or regions affected. Hierarchical linear regression was used to evaluate the contribution of pain severity to disability and that of pain severity and disability to HR-QoL measures. In each model, pain severity was entered after socio-demographic and anthropometric data (age, sex and body mass index) and clinical data (time since pain onset, number of joints/areas affected and the number of comorbid medical conditions). For HR-QoL, disability was entered also as a control variable after pain severity. HR-QoL at Month 3 was also evaluated with analogous models replacing the initial status of pain severity and disability for their changes from baseline. To check whether using non-mutually exclusive subgroups in the analyses blurred the results, sensitivity analyses were performed after excluding patients who had pain in more than one major body region (n = 1829).
The size of the sample was not formally calculated. It was anticipated that many patients would be available. The recruitment target was arbitrarily set at 6000 patients. This target was intentionally high to ensure representation of many OA locations and facilitate the participation of many specialists.
All analyses were done with the statistical package SPSS version 17.
Results
Disposition and characteristics of patients
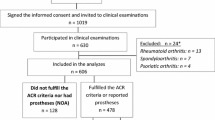
A total of 352 specialists provided data from 6003 patients. The first patient was recruited on 2 January 2013 and the last follow-up visit took place on 28 November 2013. Three were excluded because their pain intensity score at baseline was <4; thus, 6000 were used in the analyses. Of these, 5807 and 5645, respectively, came for the follow-up assessments 1 and 3 months after the initial visit. Patients were referred mostly from the primary care setting (3194, 53.2 %) but received more specialized care in this study since only 852 (14.2 %) received the study evaluations by primary care physicians. Other specialists involved in the study were orthopaedic surgeons/traumatologists (1599 patients, 26.7 %), pain clinicians (1401, 23.4 %), rehabilitators (725, 12.1 %), rheumatologists (553, 9.2 %), geriatricians (176, 2.9 %) and internists (49, 0.8 %). The specialty of the investigator was not reported for the remaining 645 patients.
The patients’ characteristics are summarised on Table 1. Two-thirds (4000 patients) were women. The mean (standard deviation, SD) age was 66.3 (11.8) years. Most patients were retired and did not perform regular physical activity. More than four-fifths (81.9 %) had at least one chronic medical condition comorbid with OA, chiefly hypertension (55.7 %), depression or anxiety (24.9 %), diabetes (20.1 %), prostatic disorders (18.5 % of men) and cardiovascular disorders (17.8 %). Patients (4171) (69.5 %) had pain in only one of the three major body regions; 1230 (20.5 %) had pain in two regions, mostly the spine and lower limbs and 599 (10.0 %) in all three.
Features of osteoarthritis, pain and differences across body regions
OA was diagnosed between 55 and 74 years of age in most patients (55–64 1992 patients, 33.2 %; 65–74 1725, 28.8 %). The time since pain onset was longer than 2 years in two thirds of patients; it lasted for 5 years or longer in more than one third. The most severe osteoarthritic pain was in the lumbosacral spine in 2229 patients (37.2 %), the knees in 1623 (27.1 %), the hips in 732 (12.2 %), the shoulders in 480 (8.0 %) and the cervical spine in 452 (7.5 %). Other joint sites (hands, dorsal spine, feet, sacroiliac joints and elbows) were noted in less than 5 % of patients. Patients (3401) (56.7 %) had pain in a single joint/area, 1084 (18.1 %) in two, 759 (12.7 %) in three and 375 (6.3 %) in four; 381 (6.4 %) had pain in five or more joints/areas. On average, patients had pain in 1.9 joints/areas. The time since pain onset was slightly shorter among patients who had OA in the upper limbs than in the other groups (Table 1). The pain at its worst in the last 24 h was on average within the severe range (mean 7.7 over 10), and within the moderate range, it was at its least (mean 4.8 over 10). There were no apparent differences among the three major body regions. Regression analyses revealed that when OA involved the spine or affected three body regions, the pain, particularly at its worst, was more severe than in the average of patients evaluated (Table 2).
Physical function limitations, disability and HR-QoL at baseline
The scores of the tools used to measure physical function limitations and disability were high at baseline (Table 1). The average Lequesne’s index was in the ‘extremely severe’ range [21] and the Oswestry score in the third over five categories of severity noted for this tool [23]. Quick-DASH scores were higher than Oswestry scores, suggesting that patients with OA in the upper limbs experienced more disability than patients with OA in the spine (Table 1). The results of the multivariate modelling are provided on Table 3. Socio-demographic/anthropometric characteristics accounted for 3, 11 and 4 % of the variance in quick-DASH, Lequesne’s index and Oswestry scores, respectively. The time since pain onset, the number of joints/areas affected and the number of comorbid conditions accounted for an additional 3, 6 and 3 %, respectively. Pain severity accounted for much more additional variability: 38 % in quick-DASH, 19 % in Lequesne’s index and 33 % in Oswestry scores. Only pain severity reached statistical significance in all three models, although the magnitude of the coefficients was lower in patients with OA in the upper limbs than in the remaining patients. Male gender (vs. female) and a shorter time since pain onset were significantly associated with lower quick-DASH and Lequesne’s indices scores, but not with Oswestry scores. The number of comorbid medical conditions was significantly associated with higher Lequesne’s index and Oswestry scores. Interestingly, the body mass index (BMI) only had significant associations with the Lequesne’s indices scores.
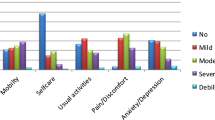
The measures of HR-QoL were low in all groups (Table 1). There were no apparent differences among them. Table 4 provides the results of the multivariate modelling. As with the measures of disability, the socio-demographic/anthropometric data, the time since pain onset, the number of joints/areas affected by OA and the number of comorbid medical conditions explained a small portion of total variance (Table 4). Conversely, both pain severity and disability scores had considerable proportions of variance. The models had good predictive ability, because they explained 50 % or more of total variance. Among the socio-demographic/anthropometric variables, male gender was associated with better HR-QoL in patients with OA in the limbs but not in the spine. Of the medical variables, the number of joints/sites affected by OA and of comorbid medical conditions was associated with HR-QoL in all models, as was the time since pain onset only in patients with OA in the lower limbs and spine. Pain severity at its worst was significantly associated with HR-QoL in all models. Achieving periods with low or very low pain severity seems to be of particular relevance for patients with OA in the lower limbs, as pain at its least was significantly associated with HR-QoL only in these patients. Disability scores showed a significant strong negative association with HR-QoL as observed in the relative magnitude of the regression coefficients.
Status after 3 months and changes from baseline
Three-month data is summarised in Table 5. Pain severity, pain interference, physical function limitations, disability and HR-QoL measures showed a substantial improvement since the initial visit. Pain at its worst became moderate and the average pain became mild (both scores fell 3 points, 30.0 % of the possible range of scores). Disability scores were reduced by at least 20.0 % of their full-scale ranges. The improvements of EQ-5D index and VAS scores represented 27.0 and 21.5 % of their respective scale breadths. Patients (67.3 %) reported a satisfaction score greater than 6 over 10 concerning both, pain relief and current HR-QoL. Two thirds of patients reported to being more or much more satisfied with the control of their pain than what they had expected at the initial visit.
The multivariate modelling of the changes from baseline of HR-QoL is reported on Table 6. Demographic and medical characteristics at baseline accounted for a minimal variance share in all the models. In opposition, changes of pain severity and disability scores accounted for relevant additional proportions of variance in HR-QoL changes, which ranged from 31 to 37 % and from 10 to 14 % for pain severity and disability scores, respectively. Improvements of pain severity and particularly disability showed strong associations with HR-QoL improvements. Greater age was associated with lesser improvements of HR-QoL in patients with OA in the spine or the lower limbs, but not in the upper limbs. The number of joints/areas affected by OA and the number of comorbid medical conditions were positively associated with HR-QoL improvements. There was also a paradoxical positive association between the time since pain onset and HR-QoL improvements in patients with OA in the lower limbs. This association was negative in patients with OA in the spine.
Sensitivity analyses
Patients with OA in only one of the three major body regions (n = 4171) were younger, had shorter time since pain onset, lesser comorbidities, lower interference and disability scores and better HR-QoL scores. The associations found between pain severity, disability and HR-QoL in this subgroup were similar to the ones found in the whole sample (data available on request).
Discussion
Comments on the main findings and comparison with existing literature
This observational study that examined a large group of patients with osteoarthritic pain in diverse body regions seeking treatment for their pain has shown that pain severity, particularly at its worst, is an important key to understanding physical function limitations, disability and HR-QoL in these patients. The associations between socio-demographic factors and disability in OA have been well known for some time [24, 25] yet, consistently with our results, more recent research has also shown that pain may contribute to most of the impairments caused by OA [26, 27].
Previous research has identified two distinct types of pain in OA: one that is intermittent but generally severe and another that is persistent and may have different qualities, such as burning, aching or stabbing [8, 27]. Interestingly, the more intense pain that occurs sporadically, particularly when unpredictable, was found to have a greater impact on HR-QoL than continuous pain [8, 28]. Thus, it is not surprising that pain at its worst severity was the single factor most consistently associated with disability and HR-QoL in this study. Furthermore, intermittent pain may lead to avoidant behaviours, since patients tend to avoid triggering, resulting in significant avoidance of social and recreational activities [28]. In turn, avoidant behaviours have been associated with greater levels of physical and psychological disability in patients with chronic pain [11].
In general terms, the differences between the groups of this study were small. Thus, one can conclude that the impact of OA location on disability and HR-QoL is lower than that of pain severity. However, there were subtle disparities that deserve comment. Patients with OA in the upper limbs produced higher scores of disability than patients with OA in the spine, despite the latter having higher pain severity than the average of patients. Also, the coefficients of pain severity in the multivariate model of disability at baseline, albeit significant, were lower in magnitude in patients with OA in the upper limbs compared to other patients, suggesting a milder association. Consistently, it was shown that OA in the hands is associated with relevant functional limitations [29] and, although the symptoms are often less limiting than when the knee or hip joints are involved, it can have an important effect on the performance of normal daily living activities [30] and HR-QoL [31]. As shoulder OA was more frequent than hand OA in this study, its results suggest that functional limitations derived from shoulder OA might be as determining for disability as those derived from hand OA. A finding that underscores the specific consequences that OA of the upper limbs may have is that it was only in these patients that age and the number of comorbidities was not associated with disability. One possible interpretation of these findings is that hip, knee or spinal OA are diseases that would typically worsen with age and thus cause progressive disability, while OA in the upper limbs would have the potential to cause disability earlier, as soon as functional limitations arise. Obesity has been related to the development and progression of OA [30]. This study has shown that obesity may also be relevant for explaining disability in patients with OA in the lower limbs but not in patients with OA in other locations, because only in the former group was BMI associated with disability. Pain severity at its least was associated with HR-QoL only in patients with OA in the lower limbs. It is possible that attaining periods in which pain is mild or even absent could be important for these patients.
The authors do not have a suitable explanation for the positive association between the time since pain onset and HR-QoL found in spine OA (the longer the time was, the better the HR-QoL). Speculatively, these patients might have grown accustomed to their pain so that they were able to resume some activities that they had originally begun to avoid following the onset of symptoms. Pain temporal features, triggering factors, changes of severity over time, cognitive or behavioural factors that may be specific to these patients might explain such a habituation effect.
Although 3 months is too short a term to evaluate the progression of OA, it sufficed to assess changes of pain severity, disability and HR-QoL measures. According to the literature on treatment outcomes, there was a ‘moderately important’ improvement of pain severity [32]. Improvements of disability scores were twice the difference that was used to delineate clinical response in a review about the course of functional status in OA, and improvements of HR-QoL were about threefold which was considered to be a minimally important clinical difference in cancer patients [33]. Because patients were evaluated in this study after a referral, these results suggest that outcomes can improve in many patients with OA who attend healthcare services by adequately referring them and optimizing the available therapies. Alternatively, training primary physicians to better recognize and treat OA pain could also help to reduce the burden caused by OA.
Clinical implications
Given the strong association between disability and HR-QoL, reducing disability would translate into improvements of HR-QoL. Pain at its worst severity was found to be consistently related to disability and HR-QoL. This may have important clinical implications, because considerable improvements in disability and HR-QoL might be attained by just reducing or suppressing pain outbursts, a much more realistic goal than achieving complete relief from pain. Multidisciplinary treatment should also focus on activity accommodations to prevent the downward spiral of activity avoidance, physical deconditioning and disability [10] in patients suffering important pain exacerbations. The influence of pain severity on disability was smaller in patients with OA in the upper limbs. It is therefore possible that patients with OA in the upper limbs may obtain particular benefits from rehabilitative therapies to regain functional ability. BMI was associated with disability measures in patients with OA in the lower limbs; weight loss may help to reduce disability in obese patients with hip or knee OA.
Limitations
The diagnosis of OA in this study was self-reported. Patients with joint pain who met certain characteristics were included as an OA population. This approach gives priority to symptomatic and functional rather than structural consequences of OA, which could explain the strong correlation found between pain severity, function limitation and HR-QoL. Although radiographic severity was found to have little association with pain and disability [34, 35], the influence of other features of OA, such as reduced joint mobility and muscle weakness, might have not been adequately captured in this research. There could be other factors linking OA to disability that were not addressed in this study, in particular, psychosocial factors such as activity limitation, self-efficacy or social isolation. The physicians who participated were a convenience, not a random sample of all specialists who treat OA outpatients in Spain; this limits the study representativeness. The correlational nature of this research precluded us from drawing causal attributions. Further research should delve into the clinical relevance of the differences reported and look into the causal relationships between physical dysfunction, disability and HR-QoL in OA patients. Data on therapeutic interventions was not collected, so that their effectiveness could not be assessed.
Conclusion
Pain severity is strongly associated with disability in patients with self-reported OA. This association is less important when OA affects the upper limbs. Together with pain severity, disability was also robustly related to HR-QoL. The associations were particularly consistent for pain severity at its worst, suggesting that pain exacerbations pose a relevant impact on disability and HR-QoL. Many patients with self-reported OA who consult for pain could obtain further benefits from referral to appropriate specialists and the optimization of available therapies.
References
Palazzo C, Ravaud JF, Papelard A, Ravaud P, Poiraudeau S (2014) The burden of musculoskeletal conditions. PLoS One 9(3):e90633. doi:10.1371/journal.pone.0090633
National Collaborating Centre for Chronic Conditions (2008) Osteoarthritis: national clinical guideline for care and management in adults. Royal College of Physicians, London
Puts MT, Deeg DJ, Hoeymans N, Nusselder WJ, Schellevis FG (2008) Changes in the prevalence of chronic disease and the association with disability in the older Dutch population between 1987 and 2001. Age Ageing 37(2):187–193. doi:10.1093/ageing/afm185
Cross M, Smith E, Hoy D, Nolte S, Ackerman I, Fransen M, Bridgett L, Williams S, Guillemin F, Hill CL, Laslett LL, Jones G, Cicuttini F, Osborne R, Vos T, Buchbinder R, Woolf A, March L (2014) The global burden of hip and knee osteoarthritis: estimates from the global burden of disease 2010 study. Ann Rheum Dis 73(7):1323–1330. doi:10.1136/annrheumdis-2013-204763
Hoy D, March L, Brooks P, Blyth F, Woolf A, Bain C, Williams G, Smith E, Vos T, Barendregt J, Murray C, Burstein R, Buchbinder R (2014) The global burden of low back pain: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis 73(6):968–974. doi:10.1136/annrheumdis-2013-204428
Nuesch E, Dieppe P, Reichenbach S, Williams S, Iff S, Juni P (2011) All cause and disease specific mortality in patients with knee or hip osteoarthritis: population based cohort study. BMJ 342:d1165. doi:10.1136/bmj.d1165
WHO Scientific Groups (2003) The burden of musculoskeletal conditions at the start of the new millennium, WHO Technical Report Series, vol 919. World Health Organization (WHO), Geneva
Hawker GA (2009) Experiencing painful osteoarthritis: what have we learned from listening? Curr Opin Rheumatol 21(5):507–512. doi:10.1097/BOR.0b013e32832e99d7
Song J, Chang RW, Dunlop DD (2006) Population impact of arthritis on disability in older adults. Arthritis Rheum 55(2):248–255. doi:10.1002/art.21842
Gatchel RJ, Peng YB, Peters ML, Fuchs PN, Turk DC (2007) The biopsychosocial approach to chronic pain: scientific advances and future directions. Psychol Bull 133(4):581–624. doi:10.1037/0033-2909.133.4.581
Keefe FJ, Rumble ME, Scipio CD, Giordano LA, Perri LM (2004) Psychological aspects of persistent pain: current state of the science. J Pain 5(4):195–211. doi:10.1016/j.jpain.2004.02.576
Gatchel RJ, Theodore BR (2008) Evidence-based outcomes in pain research and clinical practice. Pain Pract 8(6):452–460. doi:10.1111/j.1533-2500.2008.00239.x
Hoy DG, Smith E, Cross M, Sanchez-Riera L, Blyth FM, Buchbinder R, Woolf AD, Driscoll T, Brooks P, March LM (2015) Reflecting on the global burden of musculoskeletal conditions: lessons learnt from the Global Burden of Disease 2010 Study and the next steps forward. Ann Rheum Dis 74(1):4–7. doi:10.1136/annrheumdis-2014-205393
Edwards MH, van der Pas S, Denkinger MD, Parsons C, Jameson KA, Schaap L, Zambon S, Castell MV, Herbolsheimer F, Nasell H, Sanchez-Martinez M, Otero A, Nikolaus T, van Schoor NM, Pedersen NL, Maggi S, Deeg DJ, Cooper C, Dennison E (2014) Relationships between physical performance and knee and hip osteoarthritis: findings from the European Project on Osteoarthritis (EPOSA). Age Ageing 43(6):806–813. doi:10.1093/ageing/afu068
Cleeland CS, Ryan KM (1994) Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singapore 23(2):129–138
Ares JD, Prado LM, Verdecho MA, Villanueva LP, Hoyos MD, Herdman M, Lugilde ST, Rivera IV (2015) Validation of the short form of the Brief Pain Inventory (BPI-SF) in Spanish patients with non-cancer-related pain. Pain Pract 15(7):643–653. doi:10.1111/papr.12219
Herdman M, Badia X, Berra S (2001) EuroQol-5D: a simple alternative for measuring health-related quality of life in primary care. Aten Primaria 28(6):425–430
Rabin R, de Charro F (2001) EQ-5D: a measure of health status from the EuroQol Group. Ann Med 33(5):337–343
Feeny DH (2005) The roles for preference-based measures in support of cancer research and policy. In: Lipscomb J, Gotay CC, Snyder C (eds) Outcomes assessment in cancer. Cambridge University Press, Cambridge, UK, pp 69–92
Beaton DE, Wright JG, Katz JN (2005) Development of the QuickDASH: comparison of three item-reduction approaches. J Bone Joint Surg Am 87(5):1038–1046. doi:10.2106/JBJS.D.02060
Lequesne MG (1997) The algofunctional indices for hip and knee osteoarthritis. J Rheumatol 24(4):779–781
Lequesne MG, Mery C, Samson M, Gerard P (1987) Indexes of severity for osteoarthritis of the hip and knee. Validation—value in comparison with other assessment tests. Scand J Rheumatol Suppl 65:85–89
Fairbank JC, Pynsent PB (2000) The Oswestry Disability Index. Spine (Phila Pa 1976) 25(22):2940–2952, discussion 2952
Felson DT (1993) The course of osteoarthritis and factors that affect it. Rheum Dis Clin North Am 19(3):607–615
Creamer P, Lethbridge-Cejku M, Hochberg MC (2000) Factors associated with functional impairment in symptomatic knee osteoarthritis. Rheumatology (Oxford) 39(5):490–496. doi:10.1093/rheumatology/39.5.490
Corti MC, Rigon C (2003) Epidemiology of osteoarthritis: prevalence, risk factors and functional impact. Aging Clin Exp Res 15(5):359–363
Neogi T (2013) The epidemiology and impact of pain in osteoarthritis. Osteoarthritis Cartilage 21(9):1145–1153. doi:10.1016/j.joca.2013.03.018
Hawker GA, Stewart L, French MR, Cibere J, Jordan JM, March L, Suarez-Almazor M, Gooberman-Hill R (2008) Understanding the pain experience in hip and knee osteoarthritis—an OARSI/OMERACT initiative. Osteoarthritis Cartilage 16(4):415–422. doi:10.1016/j.joca.2007.12.017
Dillon CF, Hirsch R, Rasch EK, Gu Q (2007) Symptomatic hand osteoarthritis in the United States: prevalence and functional impairment estimates from the third U.S. National Health and Nutrition Examination Survey, 1991–1994. Am J Phys Med Rehabil 86(1):12–21. doi:10.1097/PHM.0b013e31802ba28e
Litwic A, Edwards MH, Dennison EM, Cooper C (2013) Epidemiology and burden of osteoarthritis. Br Med Bull 105:185–199. doi:10.1093/bmb/lds038
Michon M, Maheu E, Berenbaum F (2011) Assessing health-related quality of life in hand osteoarthritis: a literature review. Ann Rheum Dis 70(6):921–928. doi:10.1136/ard.2010.131151
Dworkin RH, Turk DC, Wyrwich KW, Beaton D, Cleeland CS, Farrar JT, Haythornthwaite JA, Jensen MP, Kerns RD, Ader DN, Brandenburg N, Burke LB, Cella D, Chandler J, Cowan P, Dimitrova R, Dionne R, Hertz S, Jadad AR, Katz NP, Kehlet H, Kramer LD, Manning DC, McCormick C, McDermott MP, McQuay HJ, Patel S, Porter L, Quessy S, Rappaport BA, Rauschkolb C, Revicki DA, Rothman M, Schmader KE, Stacey BR, Stauffer JW, von Stein T, White RE, Witter J, Zavisic S (2008) Interpreting the clinical importance of treatment outcomes in chronic pain clinical trials: IMMPACT recommendations. J Pain 9(2):105–121. doi:10.1016/j.jpain.2007.09.005
Osoba S (2005) The clinical value and meaning of health-related quality-of-life outcomes in oncology. In: Lipscomb J, Gotay CC, Snyder C (eds) Outcomes assessment in cancer. Cambridge University Press, Cambridge, UK, pp 386–405
Bedson J, Croft PR (2008) The discordance between clinical and radiographic knee osteoarthritis: a systematic search and summary of the literature. BMC Musculoskelet Disord 9:116. doi:10.1186/1471-2474-9-116
Dieppe PA (2004) Relationship between symptoms and structural change in osteoarthritis. What are the important targets for osteoarthritis therapy? J Rheumatol Suppl 70:50–53
Acknowledgements
Authors are grateful for the interest and time of clinical investigators and patients who voluntarily contributed their data for this research. The authors also wish to acknowledge STAR study investigators: A Coruña (Dr. Alhendi, Dra. Antelo, Dr. Blanco, Dr. Carceller, Dra. de la Iglesia, Dr. Díaz, Dr. García, Dr. Freire, Dr. Pérez, Dra. Rivas, Dr. Sines); Álava (Dra. Ayala, Dra. Cabello, Dra. Fernández); Albacete (Dr. Arcas, Dr. Carteleanu, Dr. García, Dr. Hernández, Dr. Jiménez, Dr. Júdez); Alicante (Dr. Escuder, Dr. González, Dr. Juan, Dr. Llanos, Dr. Moreno, Dr. Parrondo, Dr. Pérez, Dr. Tafalla, Dr. Torres, Dr. Tovar); Asturias (Dr. Acebal); Ávila (Dra. Contreras, Dr. Gil, Dr. Pinto); Badajoz (Dr. Domínguez, Dr. Lozano, Dr. Llera, Dr. Soler); Barcelona (Dra. Acosta, Dr. Amat, Dr. Ballart, Dr. Barberán, Dra. Barcelo, Dr. Benalcazar, Dra. Calahorrano, Dr. Casals, Dr. de Córdoba, Dr. de Sanctis, Dr. Echevarría, Dr. Fabo, Dr. Fernández, Dra. Ferreras, Dr. Folch, Dr. F González, Dr. J González, Dr. Guevara, Dra. Landaluze, Dr. Lopez, Dra. Magallares, Dr. Malouff, Dra. Martí, Dra. Martínez, Dr. Mayoral, Dr. Moreno, Dra. Nadal, Dr. Payan, Dr. Pellejero, Dra. Ribera, Dra. Roca, Dr. Romero, Dr. Samper, Dr. Serrano, Dra. Sintes, Dr. Sole, Dr. Solsona, Dr. Suarez, Dr. Vázquez, Dr. Vélez, Dra. Vidal); Cáceres (Dr. Leal, Dr. Abello); Cádiz (Dr. Alvarado, Dra. Álvarez, Dr. Armario, Dr. Aragón, Dr. Benítez, Dr. Calderón, Dra. del Pino, Dr. F García, Dr. S García, Dr. Gómez, Dr. F Martínez, Dr. J Martínez, Dr. MA Martínez, Dr. Menor, Dr. Morales, Dra. Moreno, Dr. Ramírez, Dr. Revenga, Dr. Sánchez de las Matas, Dra. Solís, Dr. Ventura); Cantabria (Dr. Agudo, Dra. Expósito, Dra. Martínez, Dra. Ortega, Dr. Rueda, Dra. Santillán, Dr. Sarabia); Castellón (Dra. Gil, Dr. Gómez, Dr. Mercado, Dr. Palomar, Dr. Tirado, Dr. Vicent, Dr. Vila); Ceuta (Dr. El Hmindi); Ciudad Real (Dra. Acal, Dr. Ariza, Dr. Jiménez, Dra. Monge, Dr. Molina, Dr. Paulino); Córdoba (Dra. Arroyo, Dr. Bretones, Dr. Carmona, Dr. Gómez, Dr. Jiménez, Dr. Quevedo, Dr. Vega); Girona (Dr. Beltrán, Dra. Charry, Dr. Galán, Dra. Mariñansky, Dr. Matamoros, Dr. Medina, Dr. Morales, Dr. Paredes, Dra. Ruiz); Granada (Dr. Almazán, Dr. Eugenio, Dr. Morales, Dr. Muñoz, Dra. Pozuelo, Dr. Velázquez, Dr. Villazán); Guadalajara (Dr. Pérez); Guipúzcoa (Dr. Etxebarría, Dra. Madariaga); Huelva (Dra. Llanes, Dr. Pérez); Huesca (Dr. Alarcón, Dra. Casas, Dr. Carrión, Dr. Manuel, Dr. Narro, Dr. Labad, Dr. Pina, Dr. Sánchez); Islas Baleares (Dr. Llabrés, Dr. Mirasol, Dr. Moya, Dra. Peláez, Dr. Salazar, Dr. Verd); Jaén (Dr. Esqueta, Dr. García, Dra. Gil, Dra. Granados, Dr. Martínez, Dr. Martos, Dr. Moreno); La Rioja (Dr. Malillos); Las Palmas (Dr. García, Dra. Martín, Dra. Medina, Dr. Sánchez); León (Dr. Bronte, Dr. Gutiérrez, Dra. Medina); Lleida (Dr. Charlez, Dra. Martínez, Dra. Matute, Dr. Puertas); Lugo (Dra. Albores, Dr. Miguéns); Madrid (Dra. Acedo, Dr. Alonso, Dra. Alonso, Dra. Aranda, Dra. Arconada, Dr. Bachiller, Dra. Balmisa, Dra. Bedmar, Dr. de la Gala, Dra. de Miguel, Dra. Díaz, Dr. Elices, Dr. Esparragoza, Dr. Estrada, Dra. MC Fernández, Dra. R Fernández, Dr. Gago, Dr. JA García, Dr. MA García, Dra. González, Dra. Infante, Dr. Leal, Dra. Llaurado, Dra. López, Dr. Miranda, Dr. Moreno, Dr. Molero, Dra. Nieto, Dra. Ortiz, Dra. Palomino, Dra. Peralta, Dr. Ruiz, Dra. Sánchez, Dra. Sanz, Dra. Spottorno, Dra. Vaquerizo); Málaga (Dr. Aldaya, Dra. Belmonte, Dr. Cara, Dra. Coret, Dr. González, Dr. de Linares, Dra. del Valle, Dr. Esteban, Dr. A Fernández, Dr. JA Fernández, Dr. M Fernández, Dr. García, Dra. Panero, Dr. Ponce, Dr. Rosón, Dr. Sánchez); Murcia (Dr. Aguilar, Dra. Agulló, Dra. Cirera, Dr. García, Dr. García-Giralda, Dr. Giménez, Dr. Gómez, Dr. Leal, Dr. Marras, Dra. Oliva, Dr. Ortega); Navarra (Dr. Ceberio, Dr. Gutiérrez, Dr. Sainz de Murieta); Ourense (Dra. Cánovas, Dr. Fernández, Dr. Fórmigo); Palencia (Dr. Álvarez, Dra. Páez); Pontevedra (Dra. Balsa, Dra. Mayo, Dra. Pampín, Dra. Romo); Salamanca (Dr. García, Dr. Moreno, Dr. Santos); Santa Cruz de Tenerife (Dr. Calvo, Dr. Cornejo, Dr. de la Paz, Dr. de Santiago, Dr. Maffiotte, Dra. Mencías, Dr. Muñoz, Dr. Ojeda, Dr. Santos, Dr. Vargas); Sevilla (Dr. Ballesteros, Dr. Baturone, Dr. Bordás, Dra. Bravo, Dra. León, Dra. Llanes, Dr. Méndez, Dr. Periáñez, Dr. Román, Dr. Rubio); Tarragona (Dra. Bella, Dra. Ferre, Dr. Fos, Dr. Fuentes, Dra. Gómez, Dra. Padrol, Dra. Roca); Teruel (Dra. Escartín, Dr. Giner), Toledo (Dr. Cabañas, Dr. Parrón); Valencia (Dr. Alcañiz, Dr. Alegre, Dr. Alfonso, Dr. Arriete, Dr. Asensio, Dr. Baeza, Dra. Bonond, Dra. Cabanes, Dra. Candel, Dra. Canos, Dra. Chumillas, Dr. Colomer, Dra. Domínguez, Dr. Fabregat, Dr. Fenollosa, Dr. Garijo, Dr. Gómez, Dr. Gomis, Dr. Gorgues, Dra. Izquierdo, Dr. Martín, Dra. Martín, Dr. Moreno, Dra. Navarro, Dr. Osca, Dr. Sánchez, Dr. Santamaría, Dra. Serrano, Dra. Tejero, Dr. Vidal, Dr. Villanueva, Dr. Villazala); Valladolid (Dra. Cebrián, Dr. R García, Dr. S García, Dr. González, Dr. Hernández, Dr. León, Dr. Sierra, Dr. Vaca); Vizcaya (Dr. Álava, Dra. Callejo, Dra. Fernández, Dr. García, Dra. Gómez, Dra. Latorre, Dra. López, Dra. Mozas, Dra. Muñoz, Dr. Ortíz, Dra. Ortiz, Dr. Reoyo, Dr. Saez, Dra. Torralba, Dr. Torre, Dra. Urtusagasti, Dr. Zugazabeitia); Zaragoza (Dra. Acín, Dr. Beltrán, Dr. Domingo, Dra. Lamban, Dr. Navarro, Dr. Panisello, Dr. Pons, Dra. Seral, Dra. Soriano). The authors also wish to thank Susana Traseira (Mundipharma) and Jesús Villoria (Medicxact) for their contribution during study design, data analysis and medical writing; Alfonso Casado, Ana Tabuenca for their assistance during statistical analysis.
Funding information
This research has been funded by Mundipharma, S.L. Mundipharma; S.L. did not have any direct corporate role in the design, analysis, and interpretation of results and preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
AM, J-FM, CT and JG declare no competing interests to declare. MS has a full-time job at Mundipharma Pharmaceuticals, S.L.
Ethical standards
The accredited ethics committee of the University Hospital Arnau de Vilanova in Lleida reviewed and approved the study protocol. All patients provided their written informed consent to participate and the use of their personal data for the purposes of the study. The study complied with the ethical standards of the updated Declaration of Helsinki.
Rights and permissions
About this article
Cite this article
Montero, A., Mulero, JF., Tornero, C. et al. Pain, disability and health-related quality of life in osteoarthritis—joint matters: an observational, multi-specialty trans-national follow-up study. Clin Rheumatol 35, 2293–2305 (2016). https://doi.org/10.1007/s10067-016-3248-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-016-3248-3