Abstract
Routine Assessment of Patient Index Data 3 (RAPID3) is a composite index, very useful for assessment of disease activity of various rheumatic diseases including RA. If RAPID3 can also reliably measure disease activity in axial spondyloarthritis (axSpA), it may prove to be a practical and effective quantitative assessment tool in busy practices. We studied the association of RAPID3 with Bath Ankylosing Spondylitis Disease Activity Index (BASDAI). Patients with Ankylosing Spondylitis (AS) seen from 2007 to 2012 were classified as having AS or non-radiographic axial spondyloarthritis (nr-axSpA) using modified New York criteria and Assessment of SpondyloArthritis International Society criteria, respectively. Patients with simultaneous BASDAI and RAPID3 scores were enrolled (N = 112; 105 with AS, seven with nr-axSpA). Multiple regression and nonparametric receiver operating characteristics were used. Baseline mean (SD) BASDAI and RAPID3 were 4.2 (2.5) and 3.8 (2.3), respectively. Multiple linear regressions modeled a quadratic relationship between BASDAI and RAPID3 for 321 observations in 112 patients with axSpA (1) cross-sectionally: BASDAI predicted by RAPID3 (β = 1.171; s.e. = 0.113, p < 0.001) and RAPID32 (β = −0.037; s.e. = 0.014, p = 0.011) with an adjusted R 2 of 0.676; and (2) longitudinally: BASDAI predicted by RAPID3 (β = 1.196; s.e. = 0.111, p < 0.001), RAPID32 (β = −0.042; s.e. = 0.014, p = 0.004), and visit number (β = −0.142; s.e. = 0.038, p < 0.001) with an adjusted R 2 of 0.689. RAPID3 (correctly classified) corresponded to BASDAI scores of 2, 4, and 6: 1.40 (85.8 %), 3.33 (81.9 %), and 5.43 (87.1 %), respectively. RAPID3 correlates well with BASDAI in monitoring axSpA patients (including AS) in cross-sectional and longitudinal follow-up. Since it also correlates with measures of disease activity of other rheumatic diseases including RA, RAPID3 could be an attractive measure for assessing and monitoring disease activity of several conditions seen in busy rheumatology practices.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
It is accepted that treatment informed by quantitative data assessments results in better patient outcomes than usual care without guidance [1–3]. Assessment of rheumatic diseases in daily clinical practice can be challenging as no single measure (clinical examination finding, laboratory test, or imaging) provides adequate information about disease activity and progression of disease. Various composite indices have been developed for assessing disease activity for different rheumatic diseases, for example, Disease Activity Score (DAS28) for RA, Systemic Lupus Erythematosus Disease Activity Index (SLEDAI) for SLE, Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) for AS, etc. The disease-specific indices measure some or all of the core set domains of that particular rheumatic disease, but may not give information about overall health. They can be laborious, time consuming, and thus not easy to administer particularly in busy clinical practices. Disease-specific indices that measure patient reported outcomes (PRO) have gained widespread attention and acceptance in rheumatology.
Axial spondyloarthritis (axSpA) is a chronic inflammatory disease of the axial skeleton manifested by back pain and progressive stiffness of the spine. It can also involve the hips, shoulders, peripheral joints, and extra-articular organs. It mainly affects young individuals in the second or third decade and can lead to significant loss of function, work disability, and impaired quality of life [4]. Assessment of disease activity and monitoring progression of axSpA is difficult due to paucity of objective clinical findings and its slowly progressive nature. Recent “treat-to-target” recommendations for spondyloarthritides suggest adapting therapy based on disease activity measures [5]. Two indices are used for the assessment of disease activity in AS which have been used in axSpA as well, namely the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) and the Ankylosing Spondylitis Disease Activity Score (ASDAS).
BASDAI includes six “patient reported” items measuring fatigue, back, neck or hip pain, peripheral joint pain and swelling, localized tenderness, and the duration and severity of morning stiffness [6]. It is easier to administer than ASDAS and is more widely used. Scoring BASDAI takes less than 1 min [7]. BASDAI scores greater than 4 suggest active disease, and these patients are candidates for change in medical therapy according to treatment guidelines [7].
RAPID3 (Routine Assessment of Patient Index Data 3) is a composite index of physical function, pain, and patient global estimate computed from Multidimensional Health Assessment Questionnaire (MDHAQ) questionnaire [8, 9]. It is also “patient reported” and takes only 5 to 10 s to calculate. RAPID3 has been shown to correlate significantly with DAS28 and CDAI in RA clinical trials and clinical practice [10]. RAPID3 has also been used in several other rheumatic diseases like OA, SLE, and gout where it provided consistent and quantitative information to support clinical assessment [11].
If RAPID3 can accurately measure the disease activity in axSpA, it may save time in a busy practice and also costs since a single tool could be used for assessment of several rheumatic conditions. In addition to core domains for axSpA, RAPID3 can provide information about patient function and overall health status. We conducted this study to evaluate the agreement between RAPID3 and BASDAI in patients with axSpA including AS.
Methods
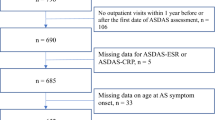
Using ICD-9 (International Classification of Diseases, 9th edition, Clinical Modification) code 720.0, patients with diagnosis of ankylosing spondylitis (AS) following at our university rheumatology clinic were identified from the electronic medical records (EMR) for the period from 2007 to 2012. We reviewed each patient’s records including chart notes, laboratory tests, and imaging findings and classified them as AS if they fulfilled modified New York (mNY) Criteria [12] and as non-radiographic axial spondyloarthritis (nr-axSpA) if they fulfilled the Assessment of SpondyloArthritis International Society (ASAS) criteria, but not the mNY criteria [13]. Patients whose diagnosis was not clear after a detailed review and those deceased were excluded from the study.
All patients attending our clinic complete Multidimensional Health Assessment Questionnaire (MDHAQ) at every visit. The RAPID3 score has three components: a 0–10 VAS pain sub-score, a 0–10 VAS global-assessment sub-score, and a function sub-score obtained from the MDHAQ. The maximum score can be 30 and is divided by three to obtain the total RAPID3 score [14, 15]. Patients with one or more sets of simultaneous BASDAI and RAPID3 scores were enrolled in the study. Their serial BASDAI and RAPID3 scores as well as demographic and clinical information were summarized.
Statistical analysis
Pearson’s correlation was plotted between individual items of BASDAI and RAPID3. Both pain and function are captured by RAPID3, but BASDAI measures predominantly pain without function. Given that function can itself be driven in part by pain, we examined the possibility of a nonlinear association between BASDAI and RAPID3 using nonparametric smoothing regressions to explore the association between total BASDAI and total RAPID3 scores without imposing an a priori constraint that such association be linear. The results informed the structure of the subsequent multiple linear regression models predicting BASDAI using RAPID3 and RAPID32, both without visit number (model 1) and controlling for visit number (model 2). Because model 2 allows that patients who were observed serially might respond differently to both BASDAI and RAPID3, for example, because of differential change in pain and change in function as the disease progressed, similar results for both models can affirm our conclusions about association between RAPID3 and BASDAI. Linear regression estimates for BASDAI over time and RAPID3 over visit number were overlaid with nonparametric estimates of trend for BASDAI and RAPID3 to confirm the fit of our parametric model to the data. We used nonparametric receiver operating characteristic (ROC) determined cutoffs of RAPID3 corresponding to BASDAI scores of 2, 4, and 6. All analyses were conducted using Stata version 12.1.
Results
Of 172 total patients identified, 14 patients did not have a clear diagnosis after reviewing their records, labs and imaging studies, and one patient was deceased. These 15 patients were excluded from the study. A total of 157 patients had axSpA; 139 had AS and 18 had nr-axSpA. Simultaneous measures of BASDAI and RAPID3 scores were available for 112 of these 157 patients. Of these 112 patients, 105 had AS and seven had nr-axSpA. Thirty-nine patients had only one visit with simultaneously available BASDAI and RAPID3 scores, and 73 patients had more than one serial measurement of BASDAI and RAPID3 scores.
Baseline characteristics
Demographic data, including clinical information about co-morbidities like smoking, obesity, depression, fibromyalgia, uveitis, inflammatory bowel disease, and psoriasis, are summarized in Table 1.
Results for axSpA
Association between BASDAI and RAPID3
Using multiple linear regression, we explained variation in BASDAI in terms of RAPID3 (β = 1.171; s.e. = 0.113, p < 0.001) and the square of RAPID3 (β = −0.037; s.e. = 0.014, p = 0.011) in a cross-sectional regression model for 321 observations in 112 patients with an adjusted R 2 of 0.676. We regressed BASDAI onto RAPID3 (β = 1.196; s.e. = 0.111, p < 0.001) and RAPID32 (β = −0.042; s.e. β = 0.014, p = 0.004) while controlling for visit number (β = −0.142; s.e. = 0.038, p < 0.001), for observations and patient with an adjusted R 2 of 0.689. These results are presented in Table 2 and in Fig. 1.
A nonparametric smoothing regression (black line; 95 % confidence band, thin dashed lines) suggested a quadratic relationship between BASDAI and RAPID3 for patients with axSpA, so a multiple least squares regression model of BASDAI as a quadratic function of RAPID3 and a linear function of period was fit (gray line). The same model was fit while accounting for within-patient clustering of observations and produced nearly identical results (dashed light gray line)
Correlation between BASDAI and RAPID3 longitudinally over visits
Figure 2 presents BASDAI and RAPID3 data plotted over time, with nonparametric and linear estimation of trends over time overlaid for patients with axSpA.
Individual BASDAI scores (light blue) and RAPID3 scores (pink) are plotted over the order of patient visits for patients with axSpA. Linear regression estimates for BASDAI over time (blue line) and RAPID3 over time (red line), along with nonparametric estimates of trend for BASDAI (blue dots) and RAPID3 (red dots), are overlaid. Both sets of estimates agree closely, with divergence only for very high visit numbers (i.e., sparse data)
Correlation among the individual items of BASDAI and RAPID3
The five individual BASDAI items—(1) fatigue, (2) neck, back, or hip pain, (3) other joint pain, (4) tender areas, and (5) stiffness (mean of duration and severity of morning stiffness)—and three individual RAPID3 items—(1) function, (2) pain, and (3) patient global health status—are all moderately to strongly correlated with one another (Fig. 3).
Cutoff scores by nonparametric ROC curves
Nonparametric ROC results are presented in Table 3 for patients with axSpA; correct classification exceeded 80 % for all three cutoffs, with decreasing sensitivity and increasing specificity as BASDAI increased.
Results for AS
Results for correlation between BASDAI and RAPID3, correlation between BASDAI and RAPID3 longitudinally over visits, correlation among the individual items of BASDAI and RAPID3, and cutoff scores by nonparametric ROC curves were very similar to those with axSpA; they have been presented in the Appendix.
Discussion
In this study, we found a moderately strong quadratic correlation between RAPID3 scores and BASDAI in the assessment and monitoring of disease activity in patients with axSpA and AS, as shown by adjusted R 2 of 0.68 and 0.69 in models 1 and 2, and also by the correct classification >80 % for BASDAI ≥ 2, BASDAI ≥ 4, and BASDAI ≥ 6. The quadratic relationship between BASDAI and RAPID3 means that RAPID3 scores are disproportionately worse at higher level of BASDAI, indicating worse patient function.
A composite index for disease activity for a disease should be able to measure the core data set domains of that particular disease. Core set domains for AS include patient global assessment, spinal pain, spinal stiffness, spinal mobility, physical function, peripheral joint and entheses, and acute phase reactants [16]. BASDAI measures spinal pain, pain from peripheral joints and entheses, and spinal stiffness. RAPID3 measures overall pain, patient global assessment, and physical function, which are included in the core set measures, thus making it a possible index for assessment of disease activity of AS.
BASDAI score of 4 or more suggests active disease and is used as one of the indications for change in treatment of AS. The RAPID3 cutoff score corresponding to BASDAI of 4 was 3.33 for both axSpA as well as AS. Also recently, it has been proposed that BASDAI of >2, >4, and >6 represent mildly active, active, and very active disease, respectively. Corresponding cutoffs for RAPID3 are 1.40, 3.33, and 5.43, respectively.
ASDAS has enhanced discriminative capacity and improved sensitivity to change as compared to BASDAI [17, 18], and hence it is appropriate to use in research studies. However, it may not be practical in clinics that care for large number of patients with a wide mix of rheumatologic diagnoses as it can be laborious and needs a blood test (ESR or CRP).
Studies have shown that RAPID3 has correlated significantly with DAS28 and CDAI in clinical trials and clinical care of RA [10, 19]. RAPID3 was comparable to DAS28 and CDAI in distinguishing active from inactive disease in clinical trials of leflunomide [20], methotrexate [20], adalimumab [21], abatacept [9], and certolizumab [22]. RAPID3 has been found to correlate with Fibromyalgia Impact Questionnaire (FIQ), revised Fibromyalgia Impact Questionnaire (FIQR), and FM symptom severity scale in follow-up of fibromyalgia patients [23]. RAPID3 has been also used in various other rheumatic diseases like OA, SLE, AS, and gout where it provided consistent and quantitative information to support clinical assessment [11]. Our investigation shows that RAPID3 may be a suitable measure of assessment and monitoring disease activity in axSpA including AS. Along with other rheumatic diseases like RA, gout, OA, and fibromyalgia, RAPID3 may be a single, simple, and effective tool to be used in busy clinical practices where disease-specific indices are difficult to measure due to time constraints while still allowing quantitative assessment of the disease activity. RAPID3 gives additional information about the patient function and overall health in addition to the disease activity for the specific disease.
Our study has several limitations. This was an observational study based on chart review, and it would be worthwhile to evaluate whether RAPID3 scores correlate with ASDAS and BASFI. We also have not assessed the discriminatory power of RAPID3 compared to BASDAI for differentiating patients with different levels of disease activity and patients with different levels of change. There were too few patients with nr-axSpA in our study to assess the performance characteristics of RAPID3 in that population, and this population remains to be studied.
Conclusion
RAPID 3 scores are quadratically associated well with BASDAI in assessing disease activity and monitoring progression in patients with axSpA and AS. Along with other rheumatic diseases like RA, gout, OA, and fibromyalgia, RAPID3 may be a single, simple, and effective tool to be used for various rheumatic diseases especially in busy clinical practices.
References
Goekoop-Ruiterman YPM, Vries-Bouwstra JK, Allaart CF, van Zeben D, Kerstens PJSM, Hazes JMW et al (2007) Comparison of treatment strategies in early rheumatoid arthritis: a randomized trial. Ann Intern Med 146:406–415
Grigor C, Capell H, Stirling A, McMahon AD, Lock P, Vallance R et al (2004) Effect of a treatment strategy of tight control for rheumatoid arthritis (the TICORA study): a single-blind randomised controlled trial. Lancet 364:263–269
Puolakka K, Kautiainen H, Möttönen T, Hannonen P, Korpela M, Hakala M et al (2005) Early suppression of disease activity is essential for maintenance of work capacity in patients with recent-onset rheumatoid arthritis: five-year experience from the FIN-RACo trial. Arthritis Rheum 52:36–41
Boonen A, Chorus A, Miedema H, van der Heijde D, van der Tempel H, van der Linden SJ (2001) Employment, work disability, and work days lost in patients with ankylosing spondylitis: a cross sectional study of Dutch patients. Ann Rheum Dis 60:353–358
Smolen JS, Braun J, Dougados M, Emery P, FitzGerald O, Helliwell P et al (2014) Treating spondyloarthritis, including ankylosing spondylitis and psoriatic arthritis, to target: recommendations of an international task force. Ann Rheum Dis 73:6–16
Garrett S, Jenkinson T, Kennedy LG, Whitelock H, Gaisford P, Calin A (1994) A new approach to defining disease status in ankylosing spondylitis: the Bath Ankylosing Spondylitis Disease Activity Index. J Rheumatol 21:2286–2291
Zochling J (2011) Measures of symptoms and disease status in ankylosing spondylitis: Ankylosing Spondylitis Disease Activity Score (ASDAS), Ankylosing Spondylitis Quality of Life Scale (ASQoL), Bath Ankylosing Spondylitis Disease Activity Index (BASDAI), Bath Ankylosing Spondylitis Functional Index (BASFI), Bath Ankylosing Spondylitis Global Score (BAS-G), Bath Ankylosing Spondylitis Metrology Index (BASMI), Dougados Functional Index (DFI), and Health Assessment Questionnaire for the Spondylarthropathies (HAQ-S). Arthritis Care Res 63(Suppl 11):47–58
Pincus T, Yazici Y, Bergman M, Maclean R, Harrington T (2007) A proposed continuous quality improvement approach to assessment and management of patients with rheumatoid arthritis without formal joint counts, based on quantitative routine assessment of patient index data (RAPID) scores on a multidimensional health assessment questionnaire (MDHAQ). Best Pract Res Clin Rheumatol 21:789–804
Pincus T, Bergman MJ, Yazici Y, Hines P, Raghupathi K, Maclean R (2008) An index of only patient-reported outcome measures, routine assessment of patient index data 3 (RAPID3), in two abatacept clinical trials: similar results to disease activity score (DAS28) and other RAPID indices that include physician-reported measures. Rheumatology (Oxford) 47:345–349
Pincus T, Swearingen CJ, Bergman M, Yazici Y (2008) RAPID3 (Routine Assessment of Patient Index Data 3), a rheumatoid arthritis index without formal joint counts for routine care: proposed severity categories compared to disease activity score and clinical disease activity index categories. J Rheumatol 35:2136–2147
Castrejón I, Bergman MJ, Pincus T (2013) MDHAQ/RAPID3 to recognize improvement over 2 months in usual care of patients with osteoarthritis, systemic lupus erythematosus, spondyloarthropathy, and gout, as well as rheumatoid arthritis. J Clin Rheumatol 19:169–174
van der Linden SM, Valkenburg HA, Cats A (1984) Evaluation of diagnostic criteria for ankylosing spondylitis. Evaluation of diagnostic criteria for ankylosing spondylitis. A proposal for modification of the New York criteria. Arthritis Rheum 27:361–368
Rudwaleit M, van der Heijde D, Landewé R, Akkoc N, Brandt J, Chou CT et al (2011) The Assessment of SpondyloArthritis International Society classification criteria for peripheral spondyloarthritis and for spondyloarthritis in general. Ann Rheum Dis 70:25–31
Pincus T, Swearingen C, Wolfe F (1999) Toward a multidimensional Health Assessment Questionnaire (MDHAQ): assessment of advanced activities of daily living and psychological status in the patient-friendly health assessment questionnaire format. Arthritis Rheum 42:2220–2230
Pincus T, Sokka T, Kautiainen H (2005) Further development of a physical function scale on a multidimensional health assessment questionnaire for standard care of patients with rheumatic diseases. J Rheumatol 32:1432–1439
van der Heijde DMFM, Bellamy N, Calin A, Dougados M, Khan MA, van der Linden SJEF (1997) Preliminary core sets for endpoints in ankylosing spondylitis. Assessments in Ankylosing Spondylitis Working Group. J Rheumatol 24:2225–2229
Lukas C, Landewé R, Sieper J et al (2009) Development of an ASAS-endorsed disease activity score (ASDAS) in patients with ankylosing spondylitis. Ann Rheum Dis 68:18–24
van der Heijde D, Lie E, Kvien TK et al (2009) ASDAS, a highly discriminatory ASAS-endorsed disease activity score in patients with ankylosing spondylitis. Ann Rheum Dis 68:1811–1818
Pincus T, Swearingen CJ, Bergman MJ, Colglazier CL, Kaell AT, Kunath AM et al (2010) RAPID3 on an MDHAQ is correlated significantly with activity levels of DAS28 and CDAI, but scored in 5 versus more than 90 seconds. Arthritis Care Res 62:181–189
Pincus T, Strand V, Koch G, Amara I, Crawford B, Wolfe F et al (2003) An index of the three core data set patient questionnaire measures distinguishes efficacy of active treatment from that of placebo as effectively as the American College of Rheumatology 20 % response criteria (ACR20) or the Disease Activity Score (DAS) in a rheumatoid arthritis clinical trial. Arthritis Rheum 48:625–630
Pincus T, Chung C, Segurado OG, Amara I, Koch GG (2006) An index of patient reported outcomes (PRO-Index) discriminates effectively between active and control treatment in 4 clinical trials of adalimumab in rheumatoid arthritis. J Rheumatol 33:2146–2152
Pincus T, Furer V, Keystone E, Yazici Y, Bergman MJ, Luijtens K (2011) RAPID3 (Routine Assessment of Patient Index Data 3) severity categories and response criteria: similar results to DAS28 (Disease Activity Score) and CDAI (Clinical Disease Activity Index) in the RAPID 1 (Rheumatoid Arthritis Prevention of Structural Damage) clinical trial of certolizumab pegol. Arthritis Care Res 63:1142–1149
Kaptanoglu E, Sahin O, Durmaz Y, Cengiz AK, Hizmetli S (2013) Routine Assessment of Patient Index Data 3 in fibromyalgia: a rapid and reliable instrument for evaluating disease severity? Arthritis Rheum 65(Suppl 10):48
Source and grants
None
Disclosures
None
Author information
Authors and Affiliations
Corresponding author
Additional information
Final manuscript has been approved by all the authors and they confirm the integrity of the work.
Appendix (results for ankylosing spondylitis)
Appendix (results for ankylosing spondylitis)
The following figures present results for analyses of patients with ankylosing spondylitis paralleling those in the main text for patients with axial spondyloarthritis.
Correlation between BASDAI and RAPID3
Ankylosing spondylitis
Using multiple regression, we explained variation in BASDAI in terms of RAPID3 (β = 1.176; s.e. = 0.116, p < 0.001) and the square of RAPID3 (β = −0.038; s.e. = 0.015, p = 0.011) in a cross-sectional regression model, for 303 observations in 105 patients with an adjusted R 2 of 0.678. We regressed BASDAI onto RAPID3 (β = 1.213; s.e. = 0.114, p < 0.001) and the square of RAPID3 (β = −0.044; s.e. = 0.015, p = 0.003) while controlling for visit number (β = −0.156; s.e. = 0.042, p < 0.001), for observations and patient with an adjusted R 2 of 0.691. These results are presented in Table 4 and in Fig. 4.
A nonparametric smoothing regression (black line; 95 % confidence band, thin dashed lines) suggested a quadratic relationship between BASDAI and RAPID3 for patients with ankylosing spondylitis, so a multiple least squares regression model of BASDAI as a quadratic function of RAPID3 and a linear function of period was fit (blue line). The same model was fit while accounting for within-patient clustering of observations and produced nearly identical results (red line)
Correlation between BASDAI and RAPID3 longitudinally over visits
Individual BASDAI scores (light blue) and RAPID3 scores (pink) are plotted over the order of patient visits for patients with ankylosing spondylitis. Linear regression estimates for BASDAI over time (blue line) and RAPID3 over time (red line), along with nonparametric estimates of trend for BASDAI (blue dots) and RAPID3 (red dots), are overlaid. Both sets of estimates agree closely, with divergence only for very high visit numbers (i.e., sparse data)
Correlation among the individual items of BASDAI and RAPID 3
Cutoff scores by nonparametric ROC curves
Rights and permissions
About this article
Cite this article
Danve, A., Reddy, A., Vakil-Gilani, K. et al. Routine Assessment of Patient Index Data 3 score (RAPID3) correlates well with Bath Ankylosing Spondylitis Disease Activity index (BASDAI) in the assessment of disease activity and monitoring progression of axial spondyloarthritis. Clin Rheumatol 34, 117–124 (2015). https://doi.org/10.1007/s10067-014-2827-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-014-2827-4