Abstract
To clarify the impact of comorbidities on treatment strategies and outcomes in patients with rheumatoid arthritis (RA) using a large observational RA cohort, the presence of comorbidities was assessed using the Charlson Comorbidity Index (CCI). Changes in medication, disease activity by Disease Activity Score-28 joint count (DAS28) over 6 months, disability assessed by the Japanese version of the Health Assessment Questionnaire (J-HAQ), and quality of life by EuroQOL-5-Dimensions (EQ-5D) over 1 year in patients with high disease activity (DAS28 > 5.1) at baseline were assessed according to age-adjusted CCI (CCIA) and categorized into four groups (CCIA 0, 1–2, 3–4, and ≥5). Among 5,317 patients, 975 patients (18.3 %) had at least one comorbidity listed by CCI. DAS28, J-HAQ, and EQ-5D increased in severity with increased CCIA levels. Among patients with high disease activity (n = 267), treatment with methotrexate and/or biologics and improved DAS28 scores, shown by attenuated intensity, were associated with increased CCIA levels. J-HAQ improved from 1.29 ± 0.31 to 0.87 ± 0.37 in 1 year in the CCIA 0 group. The adjusted difference (standard error) in J-HAQ at 1 year in CCIA 1–2, 3–4, and ≥5 groups was worse than J-HAQ in the CCIA 0 group by 0.32 (0.09, p < 0.001), 0.45 (0.10, p < 0.001), and 0.45 (0.15, p < 0.01), respectively. The magnitude of improvement of EQ-5D was significantly attenuated with increasing CCIA levels. Thus, patients with comorbidities may not experience the same degree of benefit from recent RA treatments compared with patients without comorbidities in daily practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rheumatoid arthritis (RA) is a chronic inflammatory joint disease, and RA patients tend to have comorbidities unrelated to RA or its consequences [1–3]. When joint inflammation persists despite treatment, physical activity becomes impaired, quality of life is affected, and comorbidities related to RA and coincidental diseases not related to RA or treatments may develop. Furthermore, the mortality rate in patients with RA exceeds that in the general population [4–7]. Improvements in both therapeutic agents and treatment strategies proposed within the last decade [8–12] have gradually improved disease activity by regular daily treatment practice [13–15]. Intensive treatment and tight control represent the ideal strategy for the treatment of RA [12]; however, at present, RA patients with comorbidities might not be treated with the optimal treatment strategy. Some rheumatologists have suggested that the presence of comorbidities is a major issue preventing patients from receiving the stringent treatment regimens required for RA disease control. Currently, the “treating rheumatoid arthritis to target (T2T)” strategy is recommended [12]; however, a full investigation has not been conducted of how comorbidity influences treatment strategies and to what extent the strategies affect outcomes, such as disease activity, physical dysfunction, and quality of life, in patients with RA.
One of the most established validated instruments to assess comorbidity is the Charlson Comorbidity Index (CCI) [16], which was developed to predict 1- or 10-year risk for mortality by Charlson et al. in 1987. The CCI consists of 16 diseases or conditions that are each assigned a weight of 1–6. This index was confirmed as valuable when used with the International Classification of Diseases, Ninth Revision (ICD-9) [17]. Subsequently, the age-adjusted CCI index (CCIA) considered the effect of aging on mortality in addition to the 16 diseases in the CCI by assigning one extra point for each decade above 50 years [18]. Radner et al. used the CCIA to demonstrate that the presence of comorbidities is related to concomitant physical function and quality of life in patients with RA [19, 20]. However, whether comorbidity affects treatment strategy and subsequent outcomes with respect to disease activity, physical function, and quality of life has not yet been elucidated.
The aims of this study were to clarify what proportion of RA patients have comorbidities and how these comorbidities relate to present disease activity, physical function, and quality of life of patients at the start of this study and furthermore to clarify how comorbidities affected treatment strategies and subsequent outcomes, including disease activity, physical function, and quality of life, over a 1-year period in patients with high disease activity in a large, observational, Japanese RA cohort using the CCIA.
Patients and methods
Patients
The participants in this study were Japanese RA patients who were enrolled in the April 2010 survey of the Institute of Rheumatology, Rheumatoid Arthritis (IORRA) cohort study, conducted at the outpatient clinic of the Institute of Rheumatology, Tokyo Women’s Medical University. This IORRA observational study was approved by the ethics committee of Tokyo Women’s Medical University (#2952). The characteristics and methodology of the IORRA cohort are described below. All patients fulfilled the American College of Rheumatology revised criteria for RA [21]. At the outpatient clinic, patients with RA are seen regularly, usually every 1–2 months; thus, clinical parameters and laboratory variables are documented prospectively at the biannual IORRA surveys in April and October, which are accessible for 2 months (April to May and October to November). Patients who participated in the April 2010 IORRA survey were included in the present study.
IORRA cohort
The IORRA cohort is a single-institute-based, large, observational cohort of Japanese RA patients established in October 2000 at the Institute of Rheumatology, Tokyo Women’s Medical University, and the survey is conducted biannually (in April and October). Details about patient enrollment, data collection, and characteristics of this cohort were previously reported [6, 14, 15, 22, 23]. Briefly, all patients diagnosed with RA who visited our institute were registered in the IORRA cohort after informed consent was obtained. Each patient was asked to complete a questionnaire by the responsible physician and to submit the completed questionnaire by mail. Evaluated parameters included patient assessment of pain and global evaluation by the visual analog scale (VAS), disability measured by the Japanese version of the Health Assessment Questionnaire (J-HAQ), which was validated in 2003 [24], and quality of life measured by the European Quality of Life-5 dimensions (EQ-5D). Physicians also evaluated disease activity (swollen joints, tender joints, and physician’s assessment by VAS). The Disease Activity Score-28 joint count (DAS28) was calculated [25]. Data for erythrocyte sedimentation rate, C-reactive protein, rheumatoid factor, serum creatinine, and presence of uric protein, collected during daily practice, were also included. Patients self-reported the use of any medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids (frequency and dose converted into prednisolone), and disease-modifying antirheumatic drugs (DMARDs) including methotrexate (MTX) and its dose, and biologics. More than 5,000 patients with RA were involved in each phase of the survey, and over 98 % of patients submitted the completed questionnaires by prestamped mail.
Assessment of comorbidities
This study is based on patient reports; thus, the presence and severity of comorbidities covered are limited to those that were included in the questionnaires. The IORRA questionnaire sheets included a list of diseases, and patients indicated which diseases they suffered from. The listed diseases were myocardial infarction (infarction or angina), congestive heart failure, peripheral vascular disease, cerebrovascular disease (brain hemorrhage, infarction, or subarachnoid hemorrhage), chronic pulmonary disease (emphysema, chronic bronchitis, asthma, bronchiectasis, or interstitial lung disease), ulcer disease (gastric ulcer, duodenal ulcer, or gastrointestinal hemorrhage), liver diseases, diabetes mellitus (treated with insulin or the presence of complications), hemiplegia, renal diseases, and malignancies (with the affected organ chosen from the list provided). Some of these diseases are listed in the CCI, and other diseases that are thought to be important for capturing RA patients’ conditions were also listed. Patients with dementia were not included in the IORRA study as this was a self-reported survey. The presence of liver disease was counted as 1 irrespective of its severity (mild, moderate, or severe). Whether solid tumors were localized or had metastasized was not determined by the questionnaire; thus, the presence of a solid tumor was counted as 2 irrespective of metastasis status. Acquired immune deficiency syndrome (AIDS) was not included due to privacy issues in Japan. The presence of RA was not considered as a comorbidity in this study, as previously stated by Radner et al. [20]. Presence of renal disease was determined based on patient self-reports or laboratory data (proteinuria >2+ or serum creatinine >1.2 mg/dL). Thus, the maximum total CCI count in this study was 20. By adding the age burden, the maximum total CCIA count was 24.
Relation of the presence of comorbidities and concomitant RA conditions across patients (cross-sectional study)
We analyzed the presence of comorbidities that were self-reported by patients according to the CCI using the April 2010 IORRA data. Because the median age of participants in this study was 61 years, the CCIA was more appropriate for further analysis, so the distribution of CCIA is also described. Disease activity by DAS28, physical dysfunction by J-HAQ, quality of life by EQ-5D, and medications were divided into four patient groups according to the CCIA level (0, 1–2, 3–4, and ≥5), as previously described by Radner et al. [20].
Influence of comorbidities on treatment strategy and subsequent outcomes in RA patients with high disease activity (longitudinal study)
Enrolled patients with high disease activity (DAS28 ≥ 5.1) in April 2010 (baseline) were selected for further analysis. Changes in medications from baseline to October 2010 (6 months later) were described according to the CCIA level (0, 1–2, 3–4, and ≥5). Differences between changes in DAS28, J-HAQ, and EQ-5D obtained at 6 months (October 2010) and at 1 year (April 2011) across the CCIA levels were analyzed. Preexisting comorbidities and treatments prior to this observation period might have influenced disease activity at baseline and following treatment. The IORRA cohort study was not an inception cohort study. Thus, there was a lack of information regarding each patient’s complete treatment history and disease activity. To compensate for these shortcomings, we analyzed the difference in disease activity, physical dysfunction, and quality of life at 6 months and at 1 year across the CCIA groups by adjusting for patient background characteristics using multivariate analysis.
Statistical analysis
Baseline data for cross-sectional and longitudinal studies were summarized by median and interquartile range for continuous variables and by proportion for binary variables.
In the cross-sectional study, DAS28, J-HAQ, EQ-5D, and medications used in April 2010 were analyzed according to the four CCIA levels across patients. To test the trend in DAS28, J-HAQ, EQ-5D, and doses of MTX and prednisolone, the Jonckheere test was used. To test the trend in use of medication, the Cochran-Armitage test was used.
In the longitudinal study, changes in treatment, i.e., the use and dose of MTX, the use and dose of corticosteroids (equivalent to prednisolone), and the use of biologics, were analyzed by Exact McNemar’s test and Wilcoxon signed-rank test. The clinical outcomes in patients with high disease activity at baseline, DAS28, J-HAQ, and EQ-5D were evaluated longitudinally. The observed value of DAS28, J-HAQ, and EQ-5D in those patients at baseline, at 6 months, and at 1 year for each CCIA level was described as the mean and standard error (SE). To assess the adjusted difference across CCIA groups for each clinical outcome (DAS28, J-HAQ, and EQ-5D) at 6 months and at 1 year, a linear regression model was constructed with variables including CCIA group, gender, disease duration, treatments, and corresponding baseline value. The CCIA 0 group was used as a reference group. Note that there were three clinical outcomes; thus, three linear regression models were constructed. Missing data because of loss to follow-up were imputed by the last observation for each outcome. A sample size of 267 was sufficient to detect a DAS28 change of 0.7 with a standard deviation (SD) of 1.4 and power of 0.8.
The significance level was set at 0.05. All statistical analyses were performed by R 3.0.1 (http://cran.r-project.org/) and JMP 9.0 software packages (SAS Institute Inc., Cary, NC, USA).
Results
Presence of comorbidity among patients with RA in a daily practice cohort
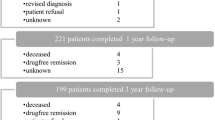
Of 5,856 patients, 5,768 patients consented to participate in the IORRA study in April 2010, and 88 patients who had participated at least once before refused to participate in this IORRA study. Of the 5,768 patients, 5,665 patients (98.2 %) submitted the questionnaire sheet. After excluding patients whose data were not adequate for this analysis, 5,317 patients (90.8 %) were analyzed.
Demographic characteristics are listed in Table 1. Women constituted 84.2 % of the population, the median age was 61.7 years, and the median disease duration was 11 years.
Comorbidities were present in 975 (18.3 %) patients, and specific diagnoses are shown in Table 2. The most frequent comorbidity in patients with RA according to the CCI was chronic pulmonary disease, which occurred in 5.6 % of patients; among these, interstitial lung disease was observed in 2.4 % of patients. Diabetes (4.2 %), ulcer disease (3.1 %), myocardial infarction (2.5 %), and malignancy (2.1 %) were also observed.
When age was considered using the CCIA, the percentages of patients in each category were 19.6 % in CCIA 0, 20.8 % in CCIA 1, 28.6 % in CCIA 2, 19.0 % in CCIA 3, 7.7 % in CCIA 4, and 4.4 % in CCIA ≥5. Thus, approximately 80 % of patients had a CCIA ≥1.
Presence of comorbidities related to concomitant RA conditions across patients (cross-sectional study)
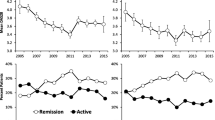
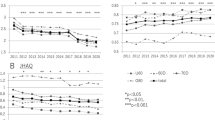
Table 3 shows the concomitant RA disease conditions and treatment according to CCIA category in all 5,317 patients in April 2010. Results of the test for trends are also indicated. Disease activity, physical dysfunction, and quality of life increasingly worsened as the CCIA increased. There was a trend in increased use of corticosteroids and dosage in association with increased CCIA levels (p < 0.0001, p < 0.0001, respectively). In contrast, there was a trend in decreased use of MTX and dosage with increased CCIA levels (p < 0.0001, p < 0.0001, respectively). The use of biologics was also attenuated with an increase in CCIA category: 20.4 % of patients in the CCIA 0 group versus 5.1 % of patients in the CCIA ≥5 used biologics (p < 0.0001).
Presence of comorbidities affected treatment strategy in RA patients with high disease activity
The right side of Table 1 shows the characteristics of 267 patients who had high disease activity (DAS28 > 5.1) in April 2010. The median J-HAQ was 1.63 and the median EQ-5D was 0.589. MTX, corticosteroids, and biologics were used in 66.3, 59.2, and 13.5 % of patients, respectively. The number of patients for each CCIA level was 38, 122, 88, and 19, respectively.
Table 4 shows changes in treatment with MTX, corticosteroids, and biologics used from baseline to 6 months by univariate analysis. Treatment with corticosteroids did not change at 6 months in any group of patients, regardless of CCIA level. The use of MTX and biologics increased among patients with fewer comorbidities, i.e., patients in the CCIA 0 and 1–2 groups, at 6 months.
Presence of comorbidities affected subsequent outcomes in RA patients with high disease activity at 6 months and at 1 year (longitudinal study)
The disease activity (indicated by the mean ± SD DAS28) of patients who had high disease activity at baseline improved from 5.70 ± 0.55 at baseline to 4.44 ± 1.33 after 6 months and to 4.38 ± 1.33 after 1 year overall. To elucidate whether the presence of comorbidities affected treatment strategies and outcomes after removing the effects of treatments administered before the observation period in this study, the adjusted difference in DAS28 in the CCIA 1–2, 3–4, and ≥5 groups compared with the CCIA 0 group as reference was analyzed at 6 months and at 1 year. As shown in Table 5, after adjustment, the DAS28 in the CCIA 1–2, 3–4, and ≥5 groups was higher by 0.22 (p = 0.397), 0.56 (p = 0.052), and 0.94 (p = 0.021), respectively, compared with DAS28 in the CCIA 0 group at 6 months. These results indicate that disease activity increased as CCIA levels increased at 6 months, and these differences had a trend toward significance. Thus, increases in CCIA levels might affect disease activity at 6 months. This phenomenon was reduced when evaluated at 1 year.
The mean (±SD) J-HAQ of patients with high disease activity at baseline changed from 1.59 ± 0.78 at baseline to 1.38 ± 0.87 after 6 months and to 1.40 ± 1.33 after 1 year overall. To elucidate whether the presence of comorbidities affected treatment strategies and outcomes after removing the effects of treatments administered before the observation period in this study, the adjusted difference in J-HAQ in the CCIA 1–2, 3–4, and ≥5 groups was analyzed using the CCIA 0 group as the reference at 6 months and at 1 year. As shown in Table 6, after adjustment, J-HAQ at 1 year in the CCIA 1–2, 3–4, and ≥5 groups was higher by 0.32 (p < 0.0001), 0.45 (p < 0.0001), and 0.45 (p = 0.003), respectively, compared with the CCIA 0 group. Thus, physical function was significantly affected in association with increased CCIA levels at 1 year.
The mean (±SD) EQ-5D of patients with high disease activity at baseline changed from 0.565 ± 0.148 at baseline to 0.572 ± 0.144 after 6 months and to 0.574 ± 0.145 after 1 year overall. To elucidate whether the presence of comorbidities affected quality of life after removing the effects of treatments administered before the observation period in this study, the adjusted difference in EQ-5D in the CCIA 1–2, 3–4, and ≥5 groups at 6 months and at 1 year was compared with that in the CCIA 0 group as reference. As shown in Table 7, after adjustment, EQ-5D at 1 year in the CCIA 1–2, 3–4, and ≥5 groups was significantly lower by 0.081 (p = 0.002), 0.086 (p = 0.004), 0.146 (p < 0.001) compared with the CCIA 0 group; thus, the presence of comorbidities significantly affected the quality of life at 1 year. These data suggest that the presence of comorbidities and age affects treatment strategies and subsequent outcomes in RA patients.
Discussion
In this study, we demonstrated that 18.3 % of patients with RA had at least one comorbidity defined using the CCI and that the presence of comorbidities greatly affected both the treatment strategy and subsequent outcomes, including disease activity, physical function, and quality of life, even when considering adjusted variable factors.
The frequency of comorbidity varies according to which comorbid conditions are considered, what types of patients are evaluated, and how the comorbidity information was obtained. About one fifth of patients had comorbidities in this study, which is relatively low compared with rates in other reports [1, 20]. Hyrich et al. reported that 58 % of RA patients in a biologics cohort had at least one comorbid condition [1] including hypertension, post-tuberculosis, asthma, and hypothyroidism. Hypertension, post-tuberculosis, asthma, and hypothyroidism are not listed in the CCI; thus, they were excluded as comorbidities in the present study. Radner et al. reported that 29.5 % of RA patients had comorbidities using the CCI [20]. The ~10 % discrepancy between their report and the present study might be because of how the comorbidity information was collected: Radner et al. collected information from physician reviews of medical charts, whereas the present study collected comorbidity data from patient self-reports. Furthermore, we did not include dementia or AIDS, and the present study only included patients who could visit the outpatient clinic to receive RA treatment and who completed the IORRA survey even after the onset of comorbidities. Therefore, patients with serious comorbidities that precluded their visiting our institute and completing the IORRA survey were omitted from evaluation. Thus, the frequency of comorbidity was relatively low in the present study.
Among the comorbidities in RA patients, chronic pulmonary disease was the most frequent comorbidity in the present study and the study by Radner et al. [20]. The precise types of chronic pulmonary disease were not addressed by Radner et al.; however, interstitial lung disease was the most frequent pulmonary comorbidity in the present study. The presence of chronic pulmonary disease, particularly interstitial lung disease and chronic bronchitis, may cause physicians to hesitate when administering intense treatment with MTX or biologics in daily practice. However, interstitial lung disease greatly affects the mortality of RA patients [6, 26]; thus, the appropriate management of RA patients with chronic pulmonary disease is crucial. The next frequent comorbidity was diabetes and peripheral vascular disease in the study by Radner et al. and diabetes and peptic ulcer disease in the current study. In both cohorts, the presence of diabetes is challenging. The frequency of diabetes is increasing globally, and diabetes is a crucial causative factor for infection and ischemic heart disease. Thus, diabetes must be prevented in patients with RA, preferably by decreasing the use of corticosteroids.
In the present study, patients with several comorbidities were revealed to be less intensively treated compared with patients with fewer comorbidities, even though their RA disease activity was high. This study also showed that disease activity at 6 months and physical function and quality of life had improved at 1 year; however, the magnitude of improvement decreased with increased comorbidity. The impact of comorbidity significantly affected disease activity at 6 months and significantly impacted both physical function and quality of life at 1 year. The time discrepancy between disease activity versus physical function and quality of life was not unexpected, as physical functions can improve after disease activity subsides, and patients experience improved quality of life when they realize that disease activity and physical function have improved. In this study, CCIA was demonstrated to be an appropriate discriminative index to estimate the subsequent outcomes of patients with RA.
The CCI was originally developed as a prognostic taxonomy for comorbid conditions that could singly or in combination prognosticate mortality. Thus, it may not be appropriate for evaluating disease activity, physical function, or quality of life in RA patients. However, the use of CCIA clearly stratified the treatment strategy and prognosticated the outcome in this study. Several previous studies assessed clinical comorbid risk in many diseases [27, 28]. In the field of rheumatology, only a few studies have demonstrated the concomitant clinical features of RA patients [19, 20]. The present study demonstrated that the CCIA is a good index for predicting future outcomes.
Irrespective of the different indication criteria among countries or insurers for the use of MTX, and particularly biologics, it is preferable to have precise indication criteria for their use in patients with comorbidities. Both patients with chronic pulmonary disease and older patients with RA have been reported as missing opportunities for treatment [29]. Furthermore, patients with many comorbidities, including age, have been less frequently treated with MTX and biologics and tend to exhibit corticosteroid dependency, resulting in worse physical function [30, 31].
The importance of each comorbidity varies depending on what type of outcome is analyzed. Michaud et al. proposed ranking the importance of the top five comorbid conditions (lung disease, myocardial infarction, fracture, stroke, and diabetes) for each specific outcome such as mortality, hospitalization, work disability, and physical disability in patients with RA [2]. Other indices have been proposed, such as the Elixhauser comorbidity index [32], but the CCI is the most established index [28], being proposed in 1987 by Charlson et al. [16]. Since then, some diseases have been newly recognized, and the characteristics and outcomes of some diseases have greatly changed owing to progress in treatment within the last quarter of a century. Recently, Ranganath et al. clearly demonstrated that comorbidities were associated with poorer outcomes in patients with RA in the community-based Consortium of Rheumatology Researchers of North America (CORRONA) registry [33]. In this study, 33 comorbid conditions were assessed; however, the types of diseases and conditions differ from those of the CCI. Thus, we need to re-ascertain what types of comorbidities are essential to make each index suitable for the prediction of each outcome in RA patients.
This study had some limitations. First, the study was based on self-reports of patients who visited our institute as there is no nationwide registry data in Japan. Second, a complete CCIA could not be performed because it is not customary to ask whether patients have AIDS, dementia, or metastatic tumors in this type of patient self-report study in Japanese daily practice. Third, the adjustment of only some background characteristics including gender, disease duration, and baseline treatment and outcomes might not have been sufficient.
In conclusion, this study demonstrated that patients with comorbidities had a poorer prognosis than patients without comorbidities. Thus, the appropriate management of patients with comorbidities is important to achieving preferred outcomes in the treatment of RA.
References
Hyrich K, Symmons D, Watson K, Silman A (2006) Baseline comorbidity levels in biologic and standard DMARD treated patients with rheumatoid arthritis: results from a national patient register. Ann Rheum Dis 65:895–898
Michaud K, Wolfe F (2007) Comorbidities in rheumatoid arthritis. Best Pract Res Clin Rheumatol 21:885–906
Gabriel SE, Michaud K (2009) Epidemiological studies in incidence, prevalence, mortality, and comorbidity of the rheumatic diseases. Arthritis Res Ther 11:229
Pincus T, Brooks RH, Callahan LF (1994) Prediction of long-term mortality in patients with rheumatoid arthritis according to simple questionnaire and joint count measures. Ann Intern Med 120:26–34
Sokka T, Abelson B, Pincus T (2008) Mortality in rheumatoid arthritis: 2008 update. Clin Exp Rheumatol 26:S35–S61
Nakajima A, Inoue E, Tanaka E et al (2010) Mortality and cause of death in Japanese patients with rheumatoid arthritis based on a large observational cohort, IORRA. Scand J Rheumatol 39:360–367
Gonzalez A, Maradit Kremers H, Crowson CS et al (2007) The widening mortality gap between rheumatoid arthritis patients and the general population. Arthritis Rheum 56:3583–3587
Aletaha D, Neogi T, Silman AJ et al (2010) 2010 Rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheum 62:2569–2581
Felson DT, Smolen JS, Wells G et al (2011) American College of Rheumatology/European League Against Rheumatism provisional definition of remission in rheumatoid arthritis for clinical trials. Arthritis Rheum 63:573–586
Smolen JS, Landewe R, Breedveld FC et al (2010) EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs. Ann Rheum Dis 69:964–975
Singh JA, Furst DE, Bharat A et al (2012) 2012 update of the 2008 American College of Rheumatology recommendations for the use of disease-modifying antirheumatic drugs and biologic agents in the treatment of rheumatoid arthritis. Arthritis Care Res (Hoboken) 64:625–639
Smolen JS, Aletaha D, Bijlsma JW et al (2010) Treating rheumatoid arthritis to target: recommendations of an international task force. Ann Rheum Dis 69:631–637
Welsing PM, Fransen J, van Riel PL (2005) Is the disease course of rheumatoid arthritis becoming milder? Time trends since 1985 in an inception cohort of early rheumatoid arthritis. Arthritis Rheum 52:2616–2624
Yamanaka H, Inoue E, Singh G et al (2007) Improvement of disease activity of rheumatoid arthritis patients from 2000 to 2006 in a large observational cohort study IORRA in Japan. Mod Rheumatol 17:283–289
Nakajima A, Inoue E, Shidara K et al (2011) Standard treatment in daily clinical practice for early rheumatoid arthritis improved disease activity from 2001 to 2006. Mod Rheumatol 21:594–597
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Deyo RA, Cherkin DC, Ciol MA (1992) Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol 45:613–619
Charlson M, Szatrowski TP, Peterson J, Gold J (1994) Validation of a combined comorbidity index. J Clin Epidemiol 47:1245–1251
Radner H, Smolen JS, Aletaha D (2011) Comorbidity affects all domains of physical function and quality of life in patients with rheumatoid arthritis. Rheumatology (Oxford) 50:381–388
Radner H, Smolen JS, Aletaha D (2010) Impact of comorbidity on physical function in patients with rheumatoid arthritis. Ann Rheum Dis 69:536–541
Arnett FC, Edworthy SM, Bloch DA et al (1988) The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum 31:315–324
Tanaka E, Hoshi D, Igarashi A et al (2013) Analysis of direct medical and nonmedical costs for care of rheumatoid arthritis patients using the large cohort database, IORRA. Mod Rheumatol 23:742–751
Yamanaka H, Seto Y, Tanaka E et al (2013) Management of rheumatoid arthritis: the 2012 perspective. Mod Rheumatol 23:1–7
Matsuda Y, Singh G, Yamanaka H et al (2003) Validation of a Japanese version of the Stanford Health Assessment Questionnaire in 3,763 patients with rheumatoid arthritis. Arthritis Rheum 49:784–788
Prevoo ML, Van't Hof MA, Kuper HH, van Leeuwen MA, van de Putte LB, van Riel PL (1995) Modified disease activity scores that include twenty-eight-joint counts. Development and validation in a prospective longitudinal study of patients with rheumatoid arthritis. Arthritis Rheum 38:44–48
Wolfe F, Caplan L, Michaud K (2007) Rheumatoid arthritis treatment and the risk of severe interstitial lung disease. Scand J Rheumatol 36:172–178
Lieffers JR, Baracos VE, Winget M, Fassbender K (2011) A comparison of Charlson and Elixhauser comorbidity measures to predict colorectal cancer survival using administrative health data. Cancer 117:1957–1965
de Groot V, Beckerman H, Lankhorst GJ, Bouter LM (2003) How to measure comorbidity. a critical review of available methods. J Clin Epidemiol 56:221–229
Radovits BJ, Fransen J, Eijsbouts A, van Riel PL, Laan RF (2009) Missed opportunities in the treatment of elderly patients with rheumatoid arthritis. Rheumatology (Oxford) 48:906–910
Iikuni N, Inoue E, Tanaka E et al (2008) Low disease activity state with corticosteroid may not represent ‘true’ low disease activity state in patients with rheumatoid arthritis. Rheumatology (Oxford) 47:519–521
Seto Y, Inoue E, Shidara K et al (2013) Functional disability can deteriorate despite suppression of disease activity in patients with rheumatoid arthritis: a large observational cohort study. Mod Rheumatol 23:1179–1185
Elixhauser A, Steiner C, Harris DR, Coffey RM (1998) Comorbidity measures for use with administrative data. Med Care 36:8–27
Ranganath VK, Maranian P, Elashoff DA et al (2013) Comorbidities are associated with poorer outcomes in community patients with rheumatoid arthritis. Rheumatology (Oxford) 52:1809–1817
Conflict of interests
Shigeki Momohara speaker fee from Abbvie, Astellas, Bristol-Myers Squibb, Chugai, Eisai, Mitsubishi Tanabe, Pfizer, and Takeda; Hisashi Yamanaka speaker fee from Abbvie, Astellas, Bristol-Myers Squibb, Chugai, Eisai, Jannsen, Mitsubishi Tanabe, Pfizer and Takeda; All other authors: None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nakajima, A., Inoue, E., Shimizu, Y. et al. Presence of comorbidity affects both treatment strategies and outcomes in disease activity, physical function, and quality of life in patients with rheumatoid arthritis. Clin Rheumatol 34, 441–449 (2015). https://doi.org/10.1007/s10067-014-2750-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-014-2750-8