Abstract
The clinical course of Behcet’s disease (BD) as a multisystemic disorder with a remitting-relapsing nature is insufficiently explored. As complete remission should be aimed in all inflammatory diseases, we investigated the frequency of complete remission in patients with BD followed in long-term, routine practice. In this retrospective study, 258 patients with BD who were regularly followed in outpatient clinics were assessed. The demographic and clinical data for active organ manifestations and treatment protocols were evaluated, and “complete remission” for this study was defined as no sign of any disease manifestation in the current visit and the preceding month. Two hundred fifty-eight patients with BD (F/M 130/128, mean age 41.1 ± 11.5 years) were included to the study. Mucocutaneous disease was present in 48.4 % (n = 125). Mean visit number was 6.8 ± 2.7, and mean follow-up duration was 45.8 ± 36.5 months. Patients were clinically active in 67.2 % (n = 1,182) of the total visits (n = 1,757), which increased to 75.6 % (68.1–90.3) when the month preceding the visit was also included. The most common active manifestation was oral ulcers (39.4–63.2 %) followed by other mucocutaneous manifestations and musculoskeletal involvement. When multivariate analysis was performed, oral ulcers, which are the main cause of the clinical activity, negatively correlated with immunosuppressive treatments (β = −0.356, p < 0.000) and age (β = −0.183, p = 0.04). It is fairly difficult to achieve complete remission in BD with current therapeutic regimens. The reluctance of the clinician to be aggressive for some BD manifestations with low morbidity, such as mucocutaneous lesions and arthritis, might be influencing the continuous, low-disease activity state, especially due to oral ulcers, in BD patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Behcet’s disease (BD) is a chronic, relapsing systemic inflammatory disease characterized by oral and urogenital aphthous ulcers and ocular, musculoskeletal, vascular, and central nervous system involvement [1]. Although the etiology is not well-defined, both genetic and environmental risk factors such as oral infections are implicated [2, 3].
In inflammatory rheumatological diseases such as rheumatoid arthritis “complete remission” (CR) is currently the ultimate goal [4]. “Treat-to-target” approach first developed for rheumatoid arthritis is currently explored also in other diseases such as systemic lupus erythematosus or vasculitides [5, 6]. However, CR in BD is investigated only in controlled studies or in open-label case series of severe disease manifestations such as uveitis, thrombosis, gastrointestinal, or central nervous system disease [7–10]. In our clinical experience, most patients in routine follow-up, even with major organ manifestations under immunosuppressive (IS) therapies, continue to have low-grade active disease due to oral ulcer (OU) presence. Course of both OU activity, the most common manifestation in clinical practice, and mucocutaneous disease as general, is insufficiently explored, and maintenance of CR in routine practice in BD is unknown. In this study, we investigated the frequency of CR and factors associated with active disease in routine follow-up of BD patients in a tertiary, referral center.
Materials and methods
We retrospectively investigated the charts of 690 patients who were consulted for possible BD in the multidisciplinary Behcet’s Outpatient Clinics of Marmara Medical Faculty Hospital. Study forms were filled only for patients followed in planned, routine visits regularly with intervals of at least 3–6 months for at least three consecutive visits. Patients with a final diagnosis other than BD, with less than three visits or irregular attendance, having unplanned visits due to disease flares, or without a follow-up visit during the last 5 years were excluded. A total of 258 patients who fulfilled the International Study Group Criteria for BD were included to the study [11]. The demographic and clinical data for active organ manifestations and treatment protocols were evaluated both for the current visit and in the last month before the visit. Complete remission for this study was defined as no sign of any organ manifestation attributed to Behcet’s disease during the visit or the preceding month, and patients having at least one of any BD manifestations were categorized as “active.”
Treatment protocols were categorized into three groups as IS agents (corticosteroids, methotrexate, azathioprine, cyclophosphamide, infliximab, or interferon-α), non-IS therapies (colchicine, nonsteroidal antiinflammatory drugs, antibiotics, or topical treatments), and no therapy. Study protocol was approved by Marmara University, School of Medicine Local Ethics Committee, and the study was performed according to the Declaration of Helsinki.
Statistical analysis
Statistical data were performed with Statistical Package for the Social Sciences 16.0 (SPSS, Chicago, IL, USA) program. The paired-samples t test, Kruskal-Wallis test, and chi-square test were used for comparisons of data. Pearson correlation test was used to analyze correlations. Linear regression analysis was performed to determine the effects of the disease manifestations or treatment protocols on disease manifestations and separately on oral ulcers.
Results
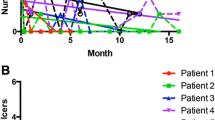
The study included 258 patients (F/M 130/128, mean age 41.1 ± 11.5 years) with BD. Mean visit number was 6.8 ± 2.7, and mean follow-up duration was 45.8 ± 36.5 months. Mucocutaneous disease was present in 125 patients (48.4 %), whereas 133 patients (51.6 %) had major organ involvement [ocular involvement (OI) 35.7 %, vascular involvement (VI) 31 %, neurological involvement (NI) 7 %, and gastrointestinal involvement 0.4 %). Patients were clinically active in 67.2 % (n = 1,182) of the total visits (n = 1,757). Frequency of active disease increased to 75.6 % (68.1–90.3) when the month before the visit was also included. When each visit was analyzed separately during the course, the major cause of activity was OU presence (39.4–63.2 %), with other mucocutaneous manifestations and musculoskeletal involvement (MI) less frequently observed (genital ulcer (GU) 3.5–27.1 %, erythema nodosum (EN) 8.2–22.5 %, papulopustular lesions (PPL) 18.2–33.7 %, MI 21.3–33.5 %) (Fig. 1). Major organ manifestations were less commonly present during routine follow-up (uveitis 0.5–8.5 % and vascular involvement 2.5–10.8 %). No difference was present between the frequency of active disease in the initial and the last visit (p = 0.41). However, oral and genital ulcers, papulopustular lesions, MI, and OI significantly decreased between the initial and the last visit.
When each visit was separately analyzed for all patients reaching to that visit number, in total 19.8–43.9 % of the patients were using IS, whereas 35.3–59.3 % was under non-IS therapies in consecutive visits. There was also a group of visits (6.4–45 %) without any treatment due to inefficacy, noncompliance, or side effects. When the distribution of the drug usage in ten visits were evaluated, 3.8–18.2 % of the patients were on corticosteroid therapy, 42.2–80.1 % were on colchicine, 0.4–14.3 % were on sulfasalazine, 1.6–6.3 % were on methotrexate, 0–8.9 % were on interferon-α, 7.8–24.2 % were on azathioprine, 0–2.3 % were on cyclophosphamide, and 0–2.5 % were on infliximab therapies.
Active disease correlated significantly with non-IS treatments (r = 0.258, p = 0.001). Similarly, oral ulcer presence showed a significant correlation with non-IS treatments (r = 0.423, p < 0.001). No differences were observed according to major organ involvement and age (>40 years). When multivariate analysis was performed, oral ulcers, which are the main cause of clinical activity, negatively correlated with IS treatments (β = −0.356, p < 0.000) and age (β = −0.183, p = 0.04). The frequency of active disease, oral ulcer presence, and non-IS therapies were significantly higher in women compared to men (p = 0.017, p = 0.002, p = 0.001, respectively), whereas vascular involvement and IS therapies were significantly higher in men (p < 0.0001 and p = 0.035, respectively) (Table 1).
Discussion
In the present study, we observed that the majority of Behcet’s disease patients are not in complete remission in the long-term, routine follow-up. The main cause of active disease was the presence of oral ulcers in all visits. Oral ulcers negatively correlated with IS treatments and age, suggesting that IS therapies may reduce OU and active disease may decrease with aging.
Colchicine is widely used (also in our clinic) without an evidence-based approach in OU, and our low rate of CR might explain the relative inefficiency of colchicine for oral manifestations. We also observed high clinical activity associated with papulopustular lesions and arthritis in our study. PPLs are shown to have bacterial presence similar to acne, and our antiinflammatory and IS treatments are possibly ineffective for most PPLs [12]. However, lack of morbidity other than cosmetic discomfort makes this manifestation of BD possibly the least treated, except in patients with antibacterial treatment for oral hygiene [13]. Inefficiency of our treatments to suppress musculoskeletal manifestations was also a surprising finding for us. Although arthritis was rare, arthralgia seemed to continue in a significant subset of the patients. Again, low morbidity due to joint involvement seems to limit our therapeutic approach in these patients.
Both clinical activity (especially oral ulcers) and non-IS therapies were significantly higher in females in our study. Female patients with BD were more frequently affected with major oral ulcers in some [14], but not in all studies [15]. In contrast, papulopustular eruptions and ocular, neurologic, and vascular involvement were more frequent in males [16]. The rate of vascular involvement and IS therapies were also significantly higher in males in our study, in accordance with the published reports.
The main limitation of our study is the selection bias of only patients coming to routine, follow-up visits. We might have missed the patients who got into CR and dropped from our clinical follow-up. However, our main aim was to observe the persistence of active disease in regularly followed patients, in whom the clinician is expected to treat more aggressively for remission during consecutive visits. Irregular or infrequent attendance may also be expected more in patients with only mucocutaneous disease, and inclusion of all BD patients might have biased our results differently. A prospective cohort study would be better to answer these biases.
In conclusion, majority of BD patients are not in complete remission in the long-term, routine follow-up, mainly due to oral ulcer presence. Negative effects of oral ulcers on oral health status and oral health-related quality of life are reported previously [17, 18]. However, the reluctance of the clinician to be aggressive for manifestations with low morbidity, such as mucocutaneous lesions and arthritis, might be causing a continuous, “low-disease activity” state in BD patients. Efficacious but also safer and practical therapies, especially for mucocutaneous lesions, are necessary for this “unmet need” in BD.
Abbreviations
- BD:
-
Behcet’s disease
- CR:
-
complete remission
- OU:
-
oral ulcers
- IS:
-
immunosuppressive
- OI:
-
ocular involvement
- VI:
-
vascular involvement
- NI:
-
neurological involvement
- MI:
-
musculoskeletal involvement
- V:
-
visit
- CA:
-
clinical activity
- GU:
-
genital ulcer
- EN:
-
erythema nodosum
- PPL:
-
papulopustular lesion
References
Sakane T, Takeno M, Suzuki N, Inaba G (1999) Behcet’s disease. N Engl 341:1284–1291
Hughes T, Coit P, Adler A, Yilmaz V, Aksu K, Düzgün N et al (2013) Identification of multiple independent susceptibility loci in the HLA region in Behçet's disease. Nat Genet 45(3):319–324. doi:10.1038/ng.2551
Mumcu G, Inanc N, Yavuz S, Direskeneli H (2007) The role of infectious agents in the pathogenesis, clinical manifestations and treatment strategies in Behçet's disease. Clin Exp Rheumatol 25(4 Suppl 45):S27–S33
Haraoui B, Smolen JS, Aletaha D, Breedveld FC, Burmester G, Codreanu C et al (2011) Treating rheumatoid arthritis to target: multinational recommendations assessment questionnaire. Ann Rheum Dis 70(11):1999–2002. doi:10.1136/ard.2011.154179
Mosca M, Boumpas DT, Bruce IN, Cervera R, Czirjak L, Dörner T et al (2012) Treat-to-target in systemic lupus erythematosus: where are we today? Clin Exp Rheumatol 30(4 Suppl 73):S112–S115
Luqmani RA (2012) Treat-to-target in vasculitis: is this a sensible approach? Clin Exp Rheumatol 30(4 Suppl 73):S149–S153
Jung YS, Hong SP, Kim TI, Kim WH, Cheon JH (2012) Long-term clinical outcomes and factors predictive of relapse after 5-aminosalicylate or sulfasalazine therapy in patients with intestinal Behcet disease. J Clin Gastroenterol 46(5):e38–e45. doi:10.1097/MCG.0b013e3182431d56
Handa T, Tsunekawa H, Yoneda M, Watanabe D, Mukai T, Yamamura M, Iwaki M, Zako M (2011) Long-term remission of ocular and extraocular manifestations in Behçet's disease using infliximab. Clin Exp Rheumatol 29(4 Suppl 67):S58–S63
Adler S, Baumgartner I, Villiger PM (2012) Behçet's disease: successful treatment with infliximab in 7 patients with severe vascular manifestations. A retrospective analysis. Arthritis Care Res (Hoboken) 64(4):607–611. doi:10.1002/acr.21557
Pipitone N, Olivieri I, Padula A, D’angelo S, Nigro A, Zuccoli G et al (2008) Infliximab for the treatment of Neuro-Behçet's disease: a case series and review of the literature. Arthritis Rheum 59(2):285–290. doi:10.1002/art.23345
International Study Group for Behçet’s Disease (1990) Criteria for diagnosis of Behçet’s disease. Lancet 335:1078–1080
Hatemi G, Bahar H, Uysal S, Mat C, Gogus F, Masatlioglu S, Altas K, Yazici H (2004) The pustular skin lesions in Behcet’s syndrome are not sterile. Ann Rheum Dis 63(11):1450–1452
Mumcu G, Ergun T, Elbir Y, Eksioglu-Demiralp E, Yavuz S, Atalay T, Direskeneli H (2005) Clinical and immunological effects of azithromycin in Behçet’s disease. J Oral Pathol Med 34(1):13–16
Cosgun S, Seyahi E, Mat C, Yazici H (2004) Female Behçet’s syndrome have more severe oral ulceration. XI. International Congress on Behçet’s Disease. Clin Exp Rheum 22:86
Mumcu G, Sur H, Inanc N, Karacayli U, Cimilli H, Sisman N, Ergun T, Direskeneli H (2009) A composite index for determining the impact of oral ulcer activity in Behcet’s disease and recurrent aphthous stomatitis. J Oral Pathol Med 38(10):785–791. doi:10.1111/j.1600-0714.2009.00803.x
Tursen U, Gurler A, Boyvat A (2003) Evaluation of clinical findings according to sex in 2313 Turkish patients with Behçet’s disease. Int J Dermatol 42(5):346–351
Mumcu G, Inanc N, Ergun T, Ikiz K, Gunes M, Islek U et al (2006) Oral health related quality of life is affected by disease activity in Behcet’s disease. Oral Dis 12:145–151
Mumcu G, Hayran O, Ozalp DO, Inanc N, Yavuz S, Ergun T, Direskeneli H et al (2007) The assessment of oral health related quality of life by factor analysis in patients with Behcet disease and recurrent apthous stomatitis. J Oral Pathol Med 36:147–152
Disclosures
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Alibaz-Oner, F., Mumcu, G., Kubilay, Z. et al. Unmet need in Behcet’s disease: most patients in routine follow-up continue to have oral ulcers. Clin Rheumatol 33, 1773–1776 (2014). https://doi.org/10.1007/s10067-014-2585-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-014-2585-3