Abstract
Different causes of mortality have been described over different decades followed by description of pathogens identified from infective episodes that led to death. A retrospective review was performed in 3,831 hospitalized systemic lupus erythematosus (SLE) patients in Peking Union Medical College Hospital from January 1986 to April 2012. The primary causes of death were identified, and the constituent ratio of specific death causes during different periods was compared. Among 3,831 hospitalized SLE patients, 268 patients died, accounting for 7.0 %. No significant difference of death rate was found between men and women, P = 0.404. The three most frequent death causes according to decade were as follows: for 1986–1995, renal involvement, lupus encephalopathy, and infections; for 1996–2005, infections, lupus encephalopathy, and renal involvement; and for 2006–2012, infections, lupus encephalopathy, and pulmonary hypertension. Certain types of deaths, primarily related to lupus activity, have decreased over time, whereas infections, often attributed to the use of corticosteroid and immunosuppressant medications, have increased gradually and changed to the most frequent death causes of SLE. Early mortality (<3 years) occurred more commonly in lupus encephalopathy, while late death (>3 years) happened more frequently in renal involvement, pulmonary artery hypertension, cardiovascular events, and cancer. In SLE death cases mainly dying from infection, mixed infections were more frequent than single pathogen infection (60.5 vs. 39.5 %), including common bacteria, fungal infection, and cytomegalovirus. Aspergillus fumigatus and Pneumocystis carinii were the two most commonly infected pathogens, and Cytomegalovirus was a frequent pathogen of mixed infection. Aggressive therapy has effectively reduced the mortality related to disease activity but also was associated with life-threatening infections. Mixed and fungal infection should be considered when SLE patients have severe infection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Systemic lupus erythematosus (SLE) is a chronic multisystem autoimmune disease characterized by the presence of multiple autoantibodies and various clinical features, predominately affecting women. It has been reported that active SLE, infection, atherosclerotic cardiovascular disease, and malignancy are the most common death causes among SLE patients [1–5].
In the past decades, the survival rate of SLE patients has been greatly improved due to earlier diagnosis, inclusion of milder cases, and administration of high-dose glucocorticoid and other cytotoxic/immunosuppressive agents. With the more intensive schemes of treatment on SLE active disease manifestation, the causes of death observed in patients with SLE in recent years are different from those reported in the past. Currently, the most frequent causes of death in patients with SLE have changed to infections [1, 3–5].
The aim of this study was to investigate the major death causes change in SLE patients during the past 26 years. We especially focused our attention on the pathogens of life-threatening infection.
Patients and methods
Patients
A retrospective medical records review was performed in 3,831 lupus patients hospitalized in Peking Union Medical College Hospital from January 1986 to April 2012. The clinical data were systematically retrieved over these decades. All lupus patients satisfied the diagnostic criteria of the American College of Rheumatology in 1982 or 1999.
Death causes
Causes of death were ascertained by review of case records, by discussion with the attending physician and when available, postmortem examination, in which the number of deaths were 242 and 26 cases, respectively. The main clinical or pathological process resulting in death were recorded as the primary causes of death, which were directly responsible for death, including infections, lupus encephalopathy, renal involvement, severe pulmonary hypertension, and diffuse alveolar hemorrhage, etc. The primary death causes were grouped under the following categories: those resulting from SLE and/or treatment-related morbidity, such as infection, malignancies, cardiovascular complications, etc.; those related to SLE activity, such as respiratory causes, renal lesions, encephalopathy, intestinal vasculitis, etc.; and those from unrelated causes. If SLE patients did not have severe organ function damage related to SLE disease activity, and they died directly from severe infection, probably resulting from SLE treatment, their death causes were defined as infection.
Statistical methods
The categorical data were presented as numbers (in percent) and the continuous variables as mean and standard deviation (SD) or median and interquartile range, depending on the data distribution type. The chi-square test was used to analyze the categorical variables; a value of P < 0.05 was considered statistically significant. Statistics were performed using the SPSS statistical package version 16.0.
Results
Demographic characteristics
Among 3,831 hospitalized SLE patients in Peking Union Medical Hospital during the past 26 years, including 3,341 females and 490 males, 268 patients died, accounting for 7.0 %. In the 268 dead cases, 238 (88.8 %) were women, accounting for 7.2 % in the 3,341 female SLE patients and 30 (11.2 %) were men, accounting for 6.2 % in the 490 male SLE patients. There was no significant difference of death rate between men and women, P = 0.404. The mean age at onset of SLE were 31.4 ± 14.0(7 ∼ 70) years. The mean age at the time of death were 37.5 ± 14.5(10 ∼ 74) years. The mean duration of disease from disease onset to death were 6.01 ± 6.70(0.02 ∼ 34) years.
Major death causes of SLE
Table 1 shows the major cause of death according to the ICD-9 codes. The principal causes of death were, in descending order of frequency, infections (37.3 %), lupus encephalopathy (18.7 %), renal involvement (13.4 %), severe pulmonary hypertension (4.9 %), and diffuse alveolar hemorrhage (4.9 %) etc.
The final event was caused by active disease manifestations in 138 patients (51.5 %). There were 36 SLE patients dying from end-stage renal failure, including 19 cases of acute renal dysfunction and 17 cases with chronic renal failure. Hematological abnormality included three patients with bleeding caused by thrombocytopenia and severe infection and one patient caused by agranulocytosis. Three patients died from intestinal vasculitis, who developed intestinal obstruction, necrosis, or/and perforation, respectively.
Five patients who died of gastrointestinal bleeding had taken cortisone and NSAIDs for a long time, despite correct gastric protection.
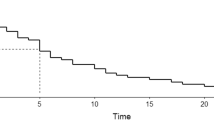
Constituent ratio of specific causes of death
Infections, lupus encephalopathy, and renal involvement were the most common causes of death among patients with SLE during the past 26 years, followed by severe pulmonary hypertension, and diffuse alveolar hemorrhage. However, there was a great change on constituent ratio of various causes of death across the different time periods (Table 2, Fig. 1).
From 1986 to 1990, renal involvement was the first common death cause, accounting for 31.4 % (11/35) in death cases and 4.0 % (11/274) in hospitalized SLE patients, whereas only three patients died from renal involvement during 2006 to 2012. Thus, the third common cause of SLE from 2006 to 2012 was severe pulmonary hypertension but not renal lesions, which accounted for 9.5 % (8/84) in death cases and 0.5 % (8/1,431) in hospitalized SLE patients. With the increase of severe infection in SLE patients, infections have changed to the first common death cause of SLE from 1996 to today.
The relationship between SLE death causes and other factors
Patient groups were characterized by the following: sex, age, or SLE duration. There was significant difference of death causes between male and female patients. Male accounted for 50.0 % of patients dying from cardiovascular events, whereas females were markedly more often seen than males in death cases of other causes, including infection, lupus encephalopathy, renal involvement, pulmonary hypertension, and diffuse alveolar hemorrhage etc., accounting for 87.6, 95.3, 80.6, 100, and 83.3 %, respectively.
The median of SLE duration from onset to death was 2 (quartile range 0.5 ∼ 6), 5 (quartile range 1.3 ∼ 13.5), 4.5 (quartile range 0.5 ∼ 10.5), and 5 years (quartile range 4 ∼ 10) for patients dying mainly from lupus encephalopathy, renal involvement, diffuse alveolar hemorrhage, and severe pulmonary hypertension, respectively, whereas the median of SLE duration was 3.8 (quartile range 0.8 ∼ 9.3), 4 (quartile range 2.0 ∼ 10.0), and 28.5 years (quartile range 24.0 ∼ 33.0) for patients dying from infection, acute cardiovascular events, and cancer. The causes of early death differed significantly from those that caused late death (shown in Table 3). Early death due to renal involvement or pulmonary artery hypertension is now rare, while death caused by lupus encephalopathy occurred more commonly in early stage (<3 years). Late death (>3 years) took place more frequently in patients dying from cardiovascular events and cancer (Table 3).
The median of age at death was 38.5 (quartile range 24.8 ∼ 46.0), 33.0 (quartile range 26.8 ∼ 47.3), 23.0 (quartile range 17.3 ∼ 47.3), and 29 years (quartile range 27 ∼ 39) for patients dying mainly from lupus encephalopathy, renal involvement, diffuse alveolar hemorrhage, and severe pulmonary hypertension, respectively, whereas the median of age at death was 40.0 (quartile range 26.0 ∼ 50.0), 59.0 (quartile range 49.0 ∼ 64.0), and 56.0 years (quartile range 53.0 ∼ 63.0) for patients dying from infection, acute cardiovascular events, and cancer.
Infection site of SLE death cases
In the present study, the most common infection site was lung, accounting for 64.9 % in death cases dying mainly from infections. In addition, sepsis, peritonitis, and meningitis were the frequent infection sites in death cases (Table 4).
Pathogens of pulmonary infection in SLE death cases
Among 66 cases dying from pulmonary infection during January 2006 to March 2012, there were 39 patients infected with definite pathogens, including 16 cases of single pathogen, and 23 cases of mixed infections, accounting for 39.5 and 60.5 %, respectively.
The most frequent causative pathogen of single pathogen infection was fungal infection (n = 10, 62.5 %), followed by common bacterial infection (n = 4, 25.0 %), and tuberculosis infection (n = 2, 12.5 %) (Table 5). Pneumocystis carinii and Aspergillus fumigates were the most common pathogens in single pathogen infection. Mixed infection included common bacteria, fungal infection, and cytomegalovirus (Table 6).
Pathogens of extrapulmonary infection in SLE death cases
Table 7 shows pathogens of extrapulmonary infection in SLE death cases. Pathogens diagnosis of disseminated fungal infection, blood stream infection, and tuberculous peritonitis were based on blood culture and clinical manifestations. Tubercular meningitis was proved by cerebrospinal fluid test and magnetic resonance imaging, while intracerebral abscess of Nocardiosis was confirmed by autopsy.
Discussion
The primary value of this study is its description of death causes change in lupus patients in a developing country. In previous studies, although aggressive therapy has effectively reduced the mortality related to disease activity, it has led to the occurrence of complications that can be related to disease itself or to almost unavoidable drug side effects, especially infections [1–8]. Iriya et al. reported that 58 % of Brazilian lupus patients had infections as the major cause of death after studying 113 autopsies [9].
Although a retrospective hospital based report on mortality remained inferior to a report of a cohort, the percentages reported in this study suggested that the death rate decreased gradually before 2005 (from 12.7 to 5.3 %), while it increased since then (from 5.3 to 5.7 %, P = 0.671). In addition, there was a great change of constituent ratio of specific death causes in SLE patients during the past 26 years. It seems clear that certain types of deaths, primarily related to lupus activity, have decreased over time, whereas infections, often attributed to the use of corticosteroid and immunosuppressant medications, have increased gradually and changed to the most frequent death causes of SLE. From 1986 to 1995, death of SLE patients was most commonly caused by severe nephritis, whereas there were only three SLE patients dying from renal involvement during 2006 to 2012. In addition to aggressive therapy which has effectively reduced the mortality related to disease activity, the significant decline of death rate in lupus nephritis also attributed to renal replacement therapy, which was widely applied on patients with end-stage renal disease after 1995. Besides, lupus nephritis, other events caused by SLE disease activity, have also decreased markedly.
It has been reported that consequent to the advent of effective immunosuppressive treatment and the prolongation of patient survival, cardiovascular disease had emerged as an important long-term complication. Previous work has shown a very high incidence of cardiac events (specifically, myocardial infarction and angina) in SLE patients compared with the general population [10–12]. The role that corticosteroid therapy plays in the development of clinical and subclinical atherosclerosis has become more evident [13]. In our study, we observed only ten death cases attributable to acute cardiovascular events caused by atherosclerosis, accounting for 3.7 % of death cases, despite the increasing frequency of cardiovascular events as cause of death in industrialized countries. It is worth noting that 50 % of the patients who died of cardiac events were males, whereas the female-to-male ratio for the death cases was 238:30.
In this study, half of deaths were the result of active disease manifestations, such as lupus encephalopathy, renal involvement, and diffuse alveolar hemorrhage, etc., including cases with low response to therapy or low compliance. Moreover, patients who died of active disease manifestations were much younger than those who died from infection, acute cardiovascular events, and cancer. Because SLE is a disease that commonly occurs before the age of 40 years, it is not surprising that the patients who died of active disease manifestations were young.
In previous report, early mortality, defined as a death occurring within 5 years of disease onset, is mainly related to disease activity or infections. Late mortality, occurring beyond 5 years disease duration, is frequently due to malignancy or cardiovascular disease [14, 15]. In our study, early death due to lupus encephalopathy occurred more commonly in early stage (<3 years), while late death (>3 years) happened more frequently in patients dying from cardiovascular events and cancer (Table 3).
Infections remained the most common immediate cause of death now. Escherichia coli and Staphylococcus aureus were the leading pathogens of bloodstream infections in SLE patients [16]. Invasive fungal disease is a life-threatening and opportunistic infection, usually occurring in the immunocompromised host [17]. In a previous study, Cryptococcus neoformans infection accounted for most fatalities in SLE patients with fungal infections [18]. It has also been reported that Aspergillus spp. infection is the most frequently indentified opportunistic invasive fungal infection in SLE patients, followed by Cryptococcus spp. and Candida spp. [19]. In the present study, we found that mixed infections were more frequent than single pathogen infection in SLE death cases (60.5 vs. 39.5 %). The most frequent causative pathogen of single pathogen infection was fungal infection, in which P. carinii was the most common pathogen, followed by A. fumigatus. Among 11 cases of fungal mixed with common bacterial infections, A. fumigatus and P. carinii were the two most commonly infected pathogens. Besides the common bacteria and fungi, cytomegalovirus was a frequent pathogen of mixed infection.
Consequently, adequate and prompt recognition and proper treatment of the infected patient are imperative, especially when patients receiving high doses of corticosteroids and immunosuppressive therapy. Early use of broad-spectrum antifungal therapy should be considered when SLE patients have severe infection.
References
Mok CC, Kwok CL, Ho LY et al (2011) Life expectancy, standardized mortality ratios, and causes of death in six rheumatic diseases in Hong Kong, China. Arthritis Rheum 63(5):1182–1189
Bernatsky S, Boivin JF, Joseph L et al (2006) Mortality in systemic lupus erythematosus. Arthritis Rheum 54(8):2550–2557
Wadee S, Tikly M, Hopley M (2007) Causes and predictors of death in South Africans with systemic lupus erythematosus. Rheumatology (Oxford) 46(9):1487–1491
Doria A, Iaccarino L, Ghirardello A et al (2006) Long-term prognosis and causes of death in systemic lupus erythematosus. Am J Med 119(8):700–706
Yap DY, Tang CS, Ma MK et al (2012) Survival analysis and causes of mortality in patients with lupus nephritis. Nephrol Dial Transplant 27(8):3248–3254
Teh C, Ling G (2013) Causes and predictors of mortality in hospitalized lupus patient in Sarawak General Hospital, Malaysia. Lupus 22(1):106–111
Kang KY, Kwok SK, Ju JH et al (2011) The causes of death in Korean patients with systemic lupus erythematosus over 11 years. Lupus 20(9):989–997
Souza DC, Santo AH, Sato EI (2012) Mortality profile related to systemic lupus erythematosus: a multiple cause-of-death analysis. J Rheumatol 39(3):496–503
Iriya SM, Capelozzi VL, Calich I et al (2001) Causes of death in patients with systemic lupus erythematosus in Sao Paulo, Brazil: a study of 113 autopsies. Arch Intern Med 161:1557
Bruce IN, Urowitz MB, Gladman DD et al (2003) Risk factors for coronary heart disease in women with systemic lupus erythematosus: The Toronto Risk Factor Study. Arthritis Rheum 48(11):3159–3167
Magder LS, Petri M (2012) Incidence of and risk factors for adverse cardiovascular events among patients with systemic lupus erythematosus. Am J Epidemiol 176(8):708–719
Gustafsson JT, Simard JF, Gunnarsson I et al (2012) Risk factors for cardiovascular mortality in patients with systemic lupus erythematosus, a prospective cohort study. Arthritis Res Ther 14(2):R46
Doria A, Shoenfeld Y, Wu R et al (2003) Risk factors for subclinical atherosclerosis in a prospective cohort of patients with systemic lupus erythematosus. Ann Rheum Dis 62:1071–1077
Moss KE, Ioannou Y, Sultan SM et al (2002) Outcome of a cohort of 300 patients with systemic lupus erythematosus attending a dedicated clinic for over two decades. Ann Rheum Dis 61:409–413
Abu-Shakra M, Urowitz MB, Gladman DD et al (1995) Mortality studies in systemic lupus erythematosus. Results from a single center.I. Causes of death. J Rheumatol 22:1259–1264
Marcos M, Fernandez C, Soriano A et al (2011) Epidemiology and clinical outcomes of bloodstream infections among lupus patients. Lupus 20(9):965–971
Weng CT, Lee NY, Liu MF et al (2010) A retrospective study of catastrophic invasive fungal infections in patients with systemic lupus erythematosus from southern Taiwan. Lupus 19(10):1204–1209
Chen HS, Tsai WP, Leu HS et al (2007) Invasive fungal infection in systemic lupus erythematosus: an analysis of 15 cases and a literature review. Rheumatology (Oxford) 46(3):539–544
Kim HJ, Park YJ, Kim WU et al (2009) Invasive fungal infections in patients with systemic lupus erythematosus: experience from affiliated hospitals of Catholic University of Korea. Lupus 18(7):661–666
Disclosures
None.
Funding
This work was supported by the National Key Technology Research and Development Program in the 11th 5 year Plan of China (nos. 2008BAI59B02 and 2008BAI59B03) and the National Natural Science Foundation of China (no. 81202360).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fei, Y., Shi, X., Gan, F. et al. Death causes and pathogens analysis of systemic lupus erythematosus during the past 26 years. Clin Rheumatol 33, 57–63 (2014). https://doi.org/10.1007/s10067-013-2383-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-013-2383-3