Abstract
Psoriatic arthritis (PsA) is an inflammatory arthropathy associated with skin and/or nail psoriasis. TNF-α, in addition to its pro-inflammatory role, is an essential cytokine for the host's defense, and its depletion by treatment may facilitate the risk of viral infections or their reactivation. The aim of this study was to evaluate the efficacy and safety of TNF-α blockers in PsA patients with concurrent hepatitis C virus (HCV) infection. This is a multicenter study carried out in four Italian centers specialized in the diagnosis and treatment of PsA. At baseline and after 6 (T6) and 12 months (T12) of therapy, data concerning PsA activity and liver tests were registered. A total of 15 PsA patients with concomitant HCV infection were included in the study. At baseline, 13 patients had low viral load, and liver enzyme tests were within the normal range. During the observation period, these values remained stable. On the other hand, at baseline, a high viral load with slightly increased values of AST and ALT was detected in one patient. At T6 and T12, these values decreased. The remaining patient, at baseline, had low viral load, but with slightly increased AST and ALT values that normalized during the observation period. This is the greatest sample size available in the literature on this topic. The data suggests that anti-TNF-α agents are effective and safe in PsA patients with concomitant HCV. We suggest that the use of anti-TNF-α agents, accompanied by close monitoring, could be a therapeutic option.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Psoriatic arthritis (PsA) is an inflammatory arthropathy associated with skin and/or nail psoriasis [1] and other possible systemic features [2, 3]. Its early detection and successful therapy significantly reduce the risk of clinical progression [4].
In the last decade, the introduction of tumor necrosis factors (TNF)-α blockers has opened new therapeutic horizons for patients and rheumatologists, these drugs being able to reduce the disease activity and block radiographic progression of joint damage [5]. TNF-α, in addition to its pro-inflammatory role, is an essential cytokine for the host defense against infective pathogens, playing an essential role in the control of viral infection and immune response by recruiting and activating macrophages, natural killer (NK) cells, T cells and antigen-presenting cells [6]. Consequently, the depletion of TNF-α by treatment may facilitate the risk of viral infections or their reactivation [6]. Therefore, patients eligible for therapy with anti-TNF-α need to be carefully investigated about possible infections, in particular, hepatitis C virus (HCV) infection.
HCV is an enveloped hepatotropic virus with a positive-sense RNA genome and is considered one of the most frequent blood-transmitted infectious diseases, with a prevalence in the Italian general population ranging from 2 to 4 % [7]. Despite established progresses in diagnosis and in treatment, HCV infection continues to be a leading cause of morbidity and mortality [7]. In HCV patients, several anti-rheumatic therapies, in particular methotrexate, sulfasalazine and leflunomide, increase the risk of hepatotoxicity, and the treatment of PsA patient with concomitant HCV remains difficult.
Data on the safety of anti-TNF-α in this kind of patients are very limited [8–12]. In addition, the available studies involve samples with extremely low sizes ranging from one to six patients studied. The aim of this study was to evaluate the efficacy and safety of TNF-α blockers in patients with PsA and concomitant HCV infection.
Patients and methods
Study design
This is a retrospective, observational, and multicenter study carried out in four Italian centers specialized in the diagnosis and treatment of PsA. Inclusion criteria were as follows: subjects >18 years old, PsA classified on the basis of CASPAR criteria, documented seropositivity for HCV and current therapy with anti-TNF-α for at least 12 months. Patients with concomitant HBsAg positivity were excluded from this study.
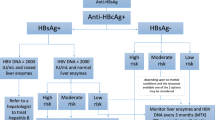
Before starting the biologic therapy, all patients underwent a medical history, clinical examination, laboratory standard tests, chest X-ray, tuberculin skin test or in vitro interferon-gamma release assays test, serological markers of hepatitis B virus and HCV in accordance with the recommendations of the Italian Society for Rheumatology for the use of biologic agents in PsA [13]. Information were collected on demographic data, PsA onset, anti-TNF-α use, disease-modifying anti-rheumatic drug (DMARD) use, concomitant comorbidities and treatments. At baseline and after 6 (T6) and 12 (T12) months of therapy, the following data concerning the PsA activity and liver tests were reported: tender joint count (68 joints), swollen joint count (66 joints), tender entheseal count, results of the Health Assessment Questionnaire, Psoriasis Area and Severity Index scores, patient pain Visual Analogical Score (VAS), patient global disease activity VAS, C-reactive protein, erythrocyte sedimentation rate, alanine aminotransferase (ALT), aspartate aminotransferase (AST), gamma-glutamyl transferase, total bilirubin and results of the quantitative HCV RNA test by polymerase chain reaction. Subject's written consent was obtained according to the Declaration of Helsinki.
Reactivation of HCV
In viremic patients, the reactivation of HCV was defined as a significant increase of HCV-RNA (at least 1 logarithm) with or without a concomitant increase of transaminases.
Results
On the basis of inclusion and exclusion criteria, a total of 15 PsA patients (nine females and six males; mean age 60.9 years, range 50–71 years; mean PsA duration 58.9 months, range 15–348 months) with concomitant HCV infection were identified and included in the study. All patients did not show other concomitant comorbidities or infectious diseases. Seven patients were on adalimumab (40 mg subcutaneously every 2 weeks) and eight on etanercept (four patients at a dosage of 50 mg subcutaneously once a week, and four patients of 25 mg subcutaneously twice a week) for a mean of 16 months of therapy (range 12–24 months). All patients were naïve for previous anti-TNF-α therapy, and no patient was on DMARD therapy. In addition, the patients had not received any specific therapy for HCV infection.
At baseline, all patients presented a high PsA activity status. After 12 months of anti-TNF-α therapy, all the variables tested improved, and all patients achieved the minimal disease activity criteria.
Regarding the HCV status, at baseline, 13 patients presented low viral load and normal liver enzyme tests. During the observation period, these values remained stable, and no patient showed reactivation of hepatitis. On the other hand, in one patient, at baseline, a high viral load (800.000 UI/mL) with slightly increased values of AST and ALT (respectively, 61 and 59 U/L) was detected. In this patient, at T6 and T12, the values of the viral load and transaminases decreased (T6 viral load 310.000 UI/mL, AST 36 U/L, ALT 30 U/L; T12 viral load 140.000 UI/mL, AST 32 U/L, ALT 29 U/L). The remaining patient, at baseline, had a viral load with low activity (14.922 UI/mL), but the AST and ALT values were slightly increased (respectively, 66 and 73 U/L). At T6 and T12, the value of the viral load was confirmed as low activity, and the AST and ALT values normalized.
Discussion
The present study evaluates the clinical course of HCV infection in PsA patients on anti-TNF-α therapy for a follow-up period of 12 months, showing that the therapy does not increase the viral load and values of liver enzyme tests. TNF-α is a pro-inflammatory cytokine with pleiotropic properties; in fact, it is not only involved in inflammatory responses and autoimmune diseases but also has a crucial role in the inflammatory processes of chronic hepatitis C [14]. It is mainly produced by monocytes and macrophages, as well as by hepatocytes [15]. Some studies have shown that serum TNF-α levels are increased in patients with chronic hepatitis C [16]. TNF-α seems to be involved in the pathogenesis of HCV through the mediation of apoptosis and the sustenance of inflammatory response [17]. In addition, it has been observed that high levels of TNF-α are associated with worse prognosis and low response to therapy with interferon [18]. On the other hand, it is known that TNF-α is an essential cytokine for the host's defense against infective pathogens, playing an essential role in the control of viral infection and immune response by recruiting and activating macrophages, NK cells, T cells and antigen-presenting cells [6]. Consequently, the depletion of TNF-α by treatment may facilitate the risk of viral infections or their reactivation [6]. Therefore, the use of TNF-α inhibitors in subjects with HCV infection requires caution, and further studies are urgently needed on this topic.
The concomitant presence of HCV infection is often encountered in PsA patients. Therapy with DMARDs could cause its reactivation, especially that methotrexate, sulfasalazine and leflunomide, in particular, have hepatotoxic potential [19]. Only cyclosporine has an anti-viral effect, inhibiting HCV replication [20].
Surprisingly enough, few data are available on the risk of HCV reactivation in patients with PsA receiving biologic therapy, and sample sizes are extremely low [8–12]. Cavazzana et al. [8] and Rokhsar et al. [9] both described one case of PsA with HCV treated with etanercept with no deterioration of viral load; likewise, Magliocco and Gottlieb who reported three cases [10]. Aslanidis et al. reported one case of PsA and chronic HCV infection on anti-TNF agents without any evidence of reactivation or flaring of hepatitis C infection [11].
The present study involved a sample of 15 PsA patients with concomitant HCV infection, followed for a period of 12 months. The results show that anti-TNF-α therapy does not modify the viral load and does not increase the values of the liver enzyme tests. In addition, in two patients, starting with increased laboratory values, the viral load and transaminases decreased and normalized from baseline to T12.
In conclusion, this study shows that anti-TNF-α agents are effective and safe in a sizeable sample of PsA patients with concomitant HCV. Therefore, we suggest that the use of anti-TNF-α agents, accompanied by close monitoring, could be safely considered among therapeutic options. In addition to the results of this study, the well-known involvement of TNF-α in the pathophysiology of HCV could also support this consideration. Prospective studies with longer follow-ups should further validate this hypothesis.
References
Moll JM, Wright V (1973) Psoriatic arthritis. Semin Arthritis Rheum 3:55–78
Scarpa R, Manguso F, D'Arienzo A, D'Armiento FP, Astarita C, Mazzacca G, Ayala F (2000) Microscopic inflammatory changes in colon of patients with both active psoriasis and psoriatic arthritis without bowel symptoms. J Rheumatol 27:1241–1246
Costa L, Caso F, D'Elia L, Atteno M, Peluso R, Del Puente A, Strazzullo P, Scarpa R (2012) Psoriatic arthritis is associated with increased arterial stiffness in the absence of known cardiovascular risk factors: a case control study. Clin Rheumatol 31:711–715
Scarpa R, Atteno M, Lubrano E, Provenzano G, D'Angelo S, Spadaro A, Costa L, Olivieri I (2011) The effectiveness and safety of TNF-alpha blockers in the treatment of early psoriatic arthritis: an Italian multicentre longitudinal observational pilot study. Clin Rheumatol 30:1063–1067
Punzi L, Podswiadek M, Sfriso P, Oliviero F, Fiocco U, Todesco S (2007) Pathogenetic and clinical rationale for TNF-blocking therapy in psoriatic arthritis. Autoimmun Rev 6:524–528
Modesti V, Ramonda R, Ortolan A, Lorenzin M, Lo Nigro A, Frallonardo P, Oliviero F, Campana C, Punzi L (2012) Infection relapse in spondyloarthritis treated with biological drugs: a single-centre study. Scand J Rheumatol 41:490–491
Fabris P, Baldo V, Baldovin T, Bellotto E, Rassu M, Trivello R, Tramarin A, Tositti G, Floreani A (2008) Changing epidemiology of HCV and HBV infections in Northern Italy: a survey in the general population. J Clin Gastroenterol 42:527–532
Cavazzana I, Ceribelli A, Cattaneo R, Franceschini F (2008) Treatment with etanercept in six patients with chronic hepatitis C infection and systemic autoimmune diseases. Autoimmun Rev 8:104–106
Rokhsar C, Rabhan N, Cohen SR (2006) Etanercept monotherapy for a patient with psoriasis, psoriatic arthritis, and concomitant hepatitis C infection. J Am Acad Dermatol 54:361–362
Magliocco MA, Gottlieb AB (2004) Etanercept therapy for patients with psoriatic arthritis and concurrent hepatitis C virus infection: report of 3 cases. J Am Acad Dermatol 51:580–584
Aslanidis S, Vassiliadis T, Pyrpasopoulou A, Douloumpakas I, Zamboulis C (2007) Inhibition of TNFalpha does not induce viral reactivation in patients with chronic hepatitis C infection: two cases. Clin Rheumatol 26:261–264
Calabrese LH, Zein N (2007) Biologic agents and liver toxicity: an added concern or therapeutic opportunity? Nat Clin Pract Rheumatol 3:422–423
Salvarani C, Olivieri I, Pipitone N, Cantini F, Marchesoni A, Punzi L, Scarpa R, Matucci-Cerinic M; Italian Society for Rheumatology (2011) Recommendations for the use of biologic therapy in the treatment of psoriatic arthritis: update from the Italian Society for Rheumatology. Clin Exp Rheumatol 29:S28–S41
Park J, Kang W, Ryu SW, Kim WI, Chang DY, Lee DH, do Park Y, Choi YH, Choi K, Shin EC, Choi C (2012) Hepatitis C virus infection enhances TNFα-induced cell death via suppression of NF-κB. Hepatology 56:831–840
Suryaprasad AG, Prindiville T (2003) The biology of TNF blockade. Autoimmun Rev 2:346–357
Tilg H, Wilmer A, Vogel W, Herold M, Nölchen B, Judmaier G, Huber C (1992) Serum levels of cytokines in chronic liver diseases. Gastroenterology 103:264–274
Freeman AJ, Marinos G, Ffrench RA, Lloyd AR (2001) Immunopathogenesis of hepatitis C virus infection. Immunol Cell Biol 79:515–536
Larrea E, Garcia N, Qian C, Civeira MP, Prieto J (1996) Tumor necrosis factor alpha gene expression and the response to interferon in chronic hepatitis C. Hepatology 23:210–217
Aletaha D, Kapral T, Smolen JS (2003) Toxicity profiles of traditional disease modifying antirheumatic drugs for rheumatoid arthritis. Ann Rheum Dis 62:482–486
Galeazzi M, Bellisai F, Giannitti C, Manganelli S, Morozzi G, Sebastiani GD (2007) Safety of cyclosporin A in HCV-infected patients: experience with cyclosporin A in patients affected by rheumatological disorders and concomitant HCV infection. Ann N Y Acad Sci 1110:544–549
Disclosures
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Luisa Costa and Francesco Caso equally contributed to this study.
Rights and permissions
About this article
Cite this article
Costa, L., Caso, F., Atteno, M. et al. Long-term safety of anti-TNF-α in PsA patients with concomitant HCV infection: a retrospective observational multicenter study on 15 patients. Clin Rheumatol 33, 273–276 (2014). https://doi.org/10.1007/s10067-013-2378-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-013-2378-0