Abstract
Multiple studies of patients in Western countries with rheumatoid arthritis (RA) and ankylosing spondylitis (AS) have indicated increased risk for active tuberculosis (TB) and other infections among these individuals. It has also been consistently reported that patients receiving tumor necrosis factor (TNF) inhibitors for these conditions have higher rates of active TB and other infections than RA or AS patients not receiving these medications. These issues have been studied less extensively in the Asia and Africa–Middle East regions, and information from these regions is important because of higher rates of TB in the general population. This paper reviews studies of RA and AS patients from Asia, Africa, and the Middle East who received TNF inhibitors. A literature search was conducted using http://www.ncbi.nlm.nih.gov/pubmed to collect and report these data. The years included in the PubMed literature search ranged from January 2000 to October 2011. Additionally, information from the China Hospital Knowledge Database was used to report data from Chinese patients with RA and AS treated with TNF inhibitors. Results from these studies indicate that the risk for active TB and other infections in AS and RA patients from Asia, Africa, and the Middle East are increased in patients receiving TNF inhibitors and that the risk is higher among those treated with monoclonal antibodies versus soluble TNF receptor.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rheumatoid arthritis (RA) is a common chronic inflammatory condition that has been estimated to affect about 1 to 2 % of individuals worldwide [1]. In China, the prevalence of RA ranges from 0.2 to 0.93 %, with the highest rate being reported from an urban area in Taiwan [2]. The prevalence of RA in Japan and Singapore is 0.31 % in men and 0.80 % in women. The combined values for the incidence of RA in Indonesia, Thailand, the Philippines, and Malaysia are 0.11 and 0.26 % for men and women, respectively. Values for India and Pakistan combined are 0.16 and 0.38 % for men and women. In the Middle East and Africa, the combined prevalence in Egypt and Morocco of patients with RA in men and women is 0.14 % and 0.38 % and those for Jordan, Saudi Arabia, and Tunisia combined is 0.16 % and 0.37 % for men and women, respectively [3]. The prevalence of RA in Iraq has been reported to be 1 % in a sample of 6,999 subjects ≥16 years old [4]. Results from the Sultanate of Oman indicated a 0.84 % [5].
Ankylosing spondylitis (AS) is a less common condition that occurs in about 0.1 % of the population with regional differences that mirror the prevalence of human leukocyte antigen (HLA)-B27 seropositivity [6]. The estimated incidence of all types of spondyloarthropathies in the Japanese population is 0.48 per 100,000 patient-years [7]. Interestingly, AS has been reported as being virtually nonexistent in several African populations which could be reflective of the low prevalence of HLA-B27 in this region [8, 9]. However, in the Algerian and Moroccan populations where AS does occur, there is a weaker association between AS and HLA-B27 than reported for European patients (63 and 67 % in Algeria and Morocco, respectively, versus 80 to 90 % in Europe). These data suggest a possible influence of other genetic/environmental determinants in the studied population [10, 11].
Treatment with tumor necrosis factor (TNF) inhibitors has been repeatedly shown to slow radiologically demonstrable disease progression and decrease symptom severity and disability in patients with RA [12]. These agents have also been used effectively in the treatment of patients with AS [13]. Analysis of clinical trial results has also indicated that TNF inhibitors have safety risks, including an increased frequency of infections. Patients with autoimmune diseases, such as RA, are generally considered to have a compromised immune system, which makes them more susceptible to infections [14]. These patients also often suffer from comorbidities, such as diabetes, which also affect immune function [14]. These factors, in combination with the immunosuppressant effects of TNF inhibitors and corticosteroids, increase the risk for infection. Additionally, results from observational studies have also indicated significantly increased risk for serious infections, including tuberculosis (TB), in patients being treated with TNF inhibitors [15].
Safety assessments in controlled clinical trials may underestimate the frequency of uncommon adverse events [16]. Most clinical trials are not powered sufficiently to assess risk for rare events, and entry criteria may exclude high-risk patients likely to receive treatment in clinical practice. Most clinical studies also have short durations of follow-up [16]. Safety information obtained from patients who have been enrolled in registries is an important complement to those from clinical trials [16]. Registry studies accurately reflect the use of treatments both in the clinical setting and over the long-term. Registries can reveal the patterns and the relevance of serious infections, such as TB, resulting from TNF inhibitor use in a variety of patient populations (e.g., patients with particular background risks, patients with specific genetic backgrounds) [16–18]. The long-term safety data obtained from registries may allow physicians to better assess their treatment options to manage patients.
It is also important to note that risk of serious infection, notably TB as a result of treatment for RA or AS, may vary as a function of the prevalence of the disease in the population, which varies greatly from one region to another. In the USA, UK, France, and Germany, the 2009 prevalence of TB is 4.5, 15.0, 7.3, and 5.9 per 100,000 in the population, respectively. In China, Hong Kong, Korea, and the Philippines, the respective values are 138.0, 98.0, 114.0, and 520.0 per 100,000, respectively. In Algeria, Egypt, Jordan, and Morocco, they are 67.0, 30.0, 6.2, and 109.0 per 100,000, respectively [19].
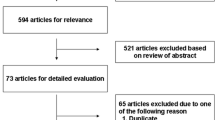
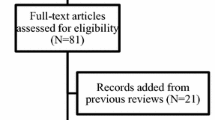
This paper reviews the risk for serious infections in patients with either RA or AS who have been or are being treated with TNF inhibitors from Asia, Africa, and the Middle East. To report these data, a literature search was conducted using http://www.ncbi.nlm.nih.gov/pubmed (years included ranged from January 2000 to October 2011). Additionally, information from the China Hospital Database was used to collect and report data from Chinese patients with RA and AS treated with TNF inhibitors. These data, summarized in Table 1, are important for rheumatologists and other physicians who prescribe biologic therapies because these areas have a high background incidence of TB and other infections.
Risk of TB and serious infection in RA and AS patients
The Asia Pacific Region
Japan
Postmarketing surveillance for 5,000 RA patients receiving infliximab with ≥6 months of follow-up indicated that 0.3 % developed TB [20]. In this study, 64 % of the patients were female and had no history of TB, and comorbidities were present more frequently in those who developed TB versus those who did not. A second study from Japan compared the infection risk for RA patients receiving TNF inhibitors versus nonbiologic agents [21]. The analysis included 1,144 patients, 646 of whom were treated with either infliximab or etanercept and were followed for up to 1 year. In patients not exposed to TNF inhibitors, the incidence rate for serious infections was 2.64 per 100 patient-years. In those treated with TNF inhibitors, the rate for serious infections is 6.42 per 100 patient-years (p = 0.026) [21].
China and Hong Kong
The prevalence of TB is high in China. Results from a survey published in 2002 that included information from 365,097 individuals indicated that the prevalence of active pulmonary TB was 367 per 100,000, the prevalence of smear-positive pulmonary TB was 122 per 100,000, and the prevalence of bacteriological-positive pulmonary TB was 160 per 100,000 [22].
Results from a study of 101 Chinese patients with active RA who received a recombinant human TNF-Fc fusion protein (etanercept) indicated no cases of TB after 24 weeks of follow-up [23]. In another study, two cases of pneumonia and one case of lymphatic TB were recorded for 87 RA patients who received five infusions of infliximab [24]. There was one reported case of lymphatic TB in the RA cohort of 67 patients treated with infliximab from a Chinese registry [25]. A study of 242 Chinese patients who received adalimumab in a 24-week double-blind trial indicated three cases of TB over the follow-up period [26]. All of these results suggest there are fewer serious infections with etanercept than with the anti-TNF antibodies, infliximab, and adalimumab [17].
The prevalence of TB in Hong Kong has been reported to be 98 per 100,000 in the population [19]. A study carried out in Hong Kong assessed the risk for TB in patients with RA versus that in the general population over the period from 2004 to 2007. This record review included information from 2,441 RA patients from five different centers. The median follow-up was 6,616 patient-years for patients not receiving a TNF inhibitor and 185 patient-years for those who received anti-TNF agents. When results for these patients were compared with those from age- and sex-matched controls from the general population, the standardized incidence ratio (SIR) for active TB in TNF-inhibitor-naive RA patients was 2.35 times that for the controls (p = 0.013) and the SIR for TNF-treated RA patients was 34.92 that for controls (p < 0.001) [27].
Results for AS in patients from China are limited relative to RA, but are generally similar. Results from a small clinical trial indicated no cases of TB in 63 patients treated with infliximab and 70 who received etanercept [28]. Similarly, no TB cases were reported in the AS cohorts of 74 patients treated with infliximab and 95 patients treated with etanercept in a Chinese registry study [25].
Taiwan
Results from 35 Taiwanese RA patients who were treated for 12 weeks with adalimumab plus methotrexate indicated three serious infections (one case of TB, one case of pneumonia, and one case of sinusitis ) [29]. Results from a study that evaluated the QuantiFERON-TB Gold (QFT-G) assay and tuberculin skin test (TST) for latent TB infection (LTBI) in 43 RA patients being treated with adalimumab indicated that before starting this treatment, eight patients (18.6 %) had positive and 35 patients (81.4 %) had negative TST results. Results from this study also indicated that 37 % of 27 patients who completed 12 months of adalimumab therapy had TST conversion. One of these patients developed active TB. Of all 43 patients who received adalimumab therapy, 9.3 % developed active TB after starting this treatment [30]. The incidence of TB in this small patient sample is much higher than that reported for the entire population of Taiwan (0.075 %). Results from this study support previous reports which state that the application of TST for detecting LTBI is limited in RA patients receiving TNF inhibitor treatment. Combining the QFT-G assay with the TST may assist in detection of patients with LTBI who are receiving immunosuppressive treatments, such as adalimumab therapy [30].
Results from 242 RA patients who received anti-TNF therapy indicated that 31.0 % had a positive TST and 45 (18.6 %) had positive QFT-G results at baseline. Four patients (three with baseline QFT-G-positive results) developed TB within the first 3 months of anti-TNF therapy, and five patients with negative baseline TST and QFT-G results developed active TB after 20 to 24 months of anti-TNF therapy. Results from this study suggest that emergence of active TB follows a biphasic pattern and the presence of persistently high levels of released interferon-γ or QFT-G conversion indicate the development of active TB in patients undergoing long-term anti-TNF therapy [31].
Philippines
Results from a small-scale study of 64 patients in this country indicated that two (one with RA and one with AS) developed pneumonia during the course of treatment with infliximab [32].
Korea
A large-scale assessment of the incidence rate and relative risk of TB in patients with RA and in those treated with TNF inhibitors has been carried out in Korea [33]. This study included 1,285 patients with RA not exposed to TNF blockers and 90 and 103 patients with RA treated with infliximab or etanercept, respectively, between 2001 and 2005. The mean incidence rate of TB was 67.2 per 100,000 patient-years from 2001 to 2004. In the TNF-blocker-naïve RA cohort, nine cases of TB developed during 3497 patient-years of follow-up (257 per 100,000). In the infliximab-treated RA group, two cases of TB developed during 78.17 patient-years of follow-up (2,558 per 100,000 patient-years), and there were no cases of TB during 73.67 patient-years of follow-up in the etanercept-treated group [33].
Kim and colleagues carried out an assessment of the incidence and relative risk of new TB infections in Korean patients with AS and patients with AS undergoing treatment with TNF blockers [34]. This review included the medical records of 919 patients with AS not treated with TNF blockers and those of 354 patients with AS who received adalimumab (n = 66), infliximab (n = 78), or etanercept (n = 210) between 2002 and 2009. The mean incidence rate of TB was 69.8 per 100,000 patient-years in the general population, 308 per 100,000 patient-years in the TNF blocker-naive AS cohort, and 561 per 100,000 patient-years in the TNF blocker-exposed AS cohort. The incidence rate for TB in the infliximab-treated AS cohort (540 per 100,000 patient-years) was higher than that in the adalimumab-treated AS cohort (490 per 100,000 patient-years). No cases of TB occurred in the etanercept-treated AS cohort [34].
Thailand
A retrospective study carried out in Thailand reviewed all infections from 100 consecutive patients who were treated with either etanercept or infliximab (46 % for RA and 41 % for AS) [35]. Results from this analysis indicated two events of suspected active TB and suspected hepatitis-B virus reactivation in patients who received etanercept. Two out of 23 patients (8.7 %) who were initially treated with infliximab had herpes zoster skin infection. The overall incidences of infection post-anti-TNF treatment were 0.122 and 0.201 cases per patient-year in patients who started treatment with etanercept and infliximab, respectively (p < 0.0001) [35].
India
Results from one study carried out in India indicated that 10.6 % of patients with RA treated with infliximab had reactivation of TB versus 5 % of those receiving etanercept [36].
Africa and Middle East Region
Morocco
A retrospective review of medical records of 494 RA patients living in Morocco revealed the incidence rate for TB was 3,640 per 100,000 persons. No patients in this study were treated with anti-TNF agents [37]. A single-center, cross-sectional, descriptive study of AS in Moroccan tertiary referral rheumatology centers reports that all patients (n = 117) used non-steroidal anti-inflammatory drugs, only 2.6 % reported using anti-TNF therapy, and TB incidence was not reported [38]. The 3 year (2008 to 2010) average incidence rates of TB per 100,000 population, as reported by the World Health Organization, is as follows: 88 for Algeria, 64 for Iraq, 29 for Bahrain, 43 for Qatar, 29 for Turkey, 24 for Tunisia, 14 for Oman, 6 for Jordan, and 3 for the United Arab Emirates [39].
Comparison of results from Asia, Africa, and the Middle East with those from North America and Europe
Results from studies carried out in Asia, Africa, and the Middle East are generally similar to those from large-scale analyses carried out in Europe and the USA. A study of patients in the Research Axed on Tolerance of Biotherapies (RATIO) registry in France assessed all cases of opportunistic infection (OI) in patients receiving anti-TNF treatment for any indication. A case-control design was used with three controls per case that were matched for inflammatory disease and sex. A total of 45 cases of non-TB OIs were recorded in 43 patients. There were 29 infections with infliximab, ten with adalimumab, and four with etanercept. Opportunistic infections were bacterial (four listeriosis, four nocardiosis, four atypical mycobacteriosis, three non-typhoid salmonellosis), viral (eight severe herpes zoster, three varicella, three extensive herpes simplex, four disseminated cytomegalovirus infections), fungal (five pneumocystosis, three invasive aspergillosis, two cryptococcosis), or parasitic (two leishmaniasis). The risks for OIs with infliximab (p < 0.0001) or adalimumab (p = 0.002) were significantly higher than that for etanercept [40]. The RATIO registry was also used to carry out a case-controlled analysis to investigate the risk of newly diagnosed TB associated with the use of anti-TNF agents. A total of 69 cases of TB were identified. The sex- and age-adjusted incidence rate of TB was 116.7 per 100,000 patient-years. The SIR was 12.2 and was higher for therapy with infliximab (18.6) and adalimumab (29.3) than for therapy with etanercept (1.8). Exposure to infliximab or adalimumab versus etanercept was an independent risk factor for TB [odds ratio (OR) = 13.3, 95 % confidence interval (CI) 2.6 to 69.0 and OR = 17.1, 95 % CI 3.6 to 80.6, respectively].
The British Society for Rheumatology Biologics Register was used to assess the risk for infection in patients being treated with TNF inhibitors [41]. A total of 1,808 patients in this registry had at least one serious infection (1,512 for anti-TNFs and 296 for nonbiologic treatments). Incidence rates were 42 per 1,000 patient-years (p < 0.05, 95 % CI 40, 44) for anti-TNFs and 32 per 1,000 patient-years for nonbiologic treatments (p < 0.05, 95 % CI 28, 36); they were 38 per 1,000 patient-years for etanercept (p < 0.05, 95 % CI 35, 42), 46 per 1,000 patient-years for infliximab (p < 0.05, 95 % CI 42, 50), and 43 per 1,000 patient-years for adalimumab (p < 0.05, 95 % CI 39, 47). Assessment of TB from this registry indicated 40 cases, all in patients receiving TNF inhibitors. The rate of TB was higher for the monoclonal antibodies adalimumab (144 events per 100,000 patient-years) and infliximab (136 per 100,000 patient-years) than for etanercept (39 per 100,000 patient-years). After modification, the incidence rate ratio (IRR) compared with etanercept-treated patients was 3.1 (95 % CI 1.0, 9.5) for infliximab and 4.2 (95 % CI 1.4, 12.4) for adalimumab [42].
Results from the Consortium of Rheumatology Researchers of North America registry in the USA also indicated increased risk for infection in patients receiving TNF inhibitors [43]. Analysis of 7,971 patients with RA indicated that the adjusted rate of infections per 100 patient-years was increased among those who received methotrexate (30.9), TNF inhibitors (40.1), the combination of methotrexate plus a TNF inhibitor (37.1) versus patients who received nonbiologic agents other than methotrexate (24.5). Treatment with a TNF inhibitor was also associated with an increased risk for OI (IRR = 1.67) [43].
The Registro Español de Acontecimientos Adversos de Terapias Biológicas en Enfermedades Reumáticas registry in Spain was used to assess infection rates in 4,006 RA and 1,524 AS patients taking infliximab, etanercept, or adalimumab. The risks of infections for patients with RA taking infliximab, adalimumab, or etanercept were 5.87, 18.9, and 1.01 times those for controls, respectively. The risks of infections for patients with AS taking infliximab, adalimumab, or etanercept were 7.07, 12.71, and 1.74 times those for controls, respectively [44].
Discussion and conclusions
RA is a worldwide inflammatory joint disease with variable degrees of joint damage and extra-articular manifestations (EAMs) in different regions. Generally, RA is less severe and has fewer EAMs in Eastern Mediterranean countries in comparison with Northern Europe [45]. Several radiological studies of RA patients in Saudi Arabia showed the proportion with erosions is lower than data reported from Western European and North American populations [46]. In contrast, an evaluation of EAMs of Saudi Arabian RA patients showed that the frequency of EAMs was similar to the British population but higher than in North American populations [45]. These differences in disease progression and outcome are influenced by a multitude of factors including different expression of combinations of genes. The higher expression of HLA-DRB1 gene (DRB1*0401) in French RA patients was associated with high RA severity compared to Syrian patients who had lower expression DRB1 and less severe RA [47]. An exhaustive discussion of the genetics and other factors contributing to the different regional severity of RA is beyond the scope of this review.
While there are regional differences in RA disease severity, results from safety studies carried out in Asia, Africa, and the Middle East are generally similar to those from large-scale analyses carried out in Europe and the USA. Prescribing information for all TNF inhibitors contains the same boxed warning with respect to infections. It is noted that there is increased risk of serious infections leading to hospitalization or death, including TB, bacterial sepsis, invasive fungal infections (such as histoplasmosis), and infections due to other opportunistic pathogens and that the TNF inhibitor should be discontinued if a patient develops a serious infection or sepsis during treatment. It is also recommended that a test for latent TB be performed, and if positive, treatment for TB should be started prior to initiation of TNF inhibitor treatment. The TST is most frequently used to detect LTBI. However, due to known limitations of the TST, interferon-γ release assays (IGRAs), including QFT-G and T-SPOT.TB, have been developed. Unlike IGRAs, the TST may result in non-specific reactivity in patients exposed to non-tubercular mycobacteria (NTM) or in patients vaccinated with Bacille Calmette–Guérin (BCG). Thus, the use of IGRAs is particularly important in areas with a high-risk of TB, where BCG vaccination or NTM exposure is prevalent. Although there are no guidelines regarding how often TB screening should be repeated, periodic testing is recommended in areas with a high prevalence of TB, particularly prior to TNF inhibitor treatment. Additionally, repeated testing is especially important in immunosuppressed patients who may have been exposed to TB, but have had prior negative screening tests [48]. All patients should also be monitored for active TB during treatment [17]. Chest radiography is the method most often utilized to evaluate the possibility of active TB [48].
Results from the present review (summarized in Table 1) underscore the need of patient registries for assessment of the safety of medications used for the treatment of RA and AS. Evaluation of the results of such registries and clinical trials in Asia, Africa, the Middle East, as well as in North America and Europe indicates that RA and AS patients taking TNF inhibitors have an increased risk for serious infections versus similar patients not receiving these agents and that there are no substantial differences in risk for patients from different regions. These studies have also indicated that patients taking etanercept have lower risk for infections versus those receiving adalimumab or infliximab [17]. Several explanations have been put forward to explain this difference [48, 49]. It has been proposed that the monoclonal antibodies infliximab and adalimumab bind to membrane TNF with greater affinity and, more importantly, greater stability compared to TNF soluble receptors [49, 50]. More stable binding to membrane TNF induces a number of biological events in cells that express membrane TNF, such as apoptosis and loss of function via reverse signaling [49]. Membrane TNF expression plays a crucial role in granuloma development [49], and this difference in the mechanism of action explains the higher risk of TB and other OI with monoclonal antibodies. Regardless of the underlying mechanism, registries worldwide have suggested a difference in the risk for infection with etanercept versus anti-TNF monoclonal antibodies [17]. While there are limitations regarding safety information from patient registries, the consistency of results from around the world support this conclusion [17].
References
Lawrence RC, Felson DT, Helmick CG et al (2008) Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum 58:26–35
Zeng QY, Chen R, Daramawan J et al (2008) Rheumatic diseases in China. Arthritis Res Ther 10:R17
Symmons D, Mathers C, Pfleger B (2006) The global burden of rheumatoid arthritis in the year 2000. Working Paper, World Health Organization, Geneva www.who.int/healthinfo/statistics/bod_rheumatoidarthritis.pdf. Accessed 26 Apr 2012
Al-Rawi ZS, Alazzawi AJ, Alajili FM, Alwakil R (1978) Rheumatoid arthritis in population samples in Iraq. Ann Rheum Dis 37:73–75
Pountain G (1991) The prevalence of rheumatoid arthritis in the Sultanate of Oman. Br J Rheumatol 30:24–28
Gabriel SE, Michaud K (2009) Epidemiological studies in incidence, prevalence, mortality, and comorbidity of the rheumatic diseases. Arthritis Res Ther 11:229
Hukuda S, Minami M, Saito T et al (2001) Spondyloarthropathies in Japan: nationwide questionnaire survey performed by the Japan Ankylosing Spondylitis Society. J Rheumatol 28:554–559
Mijiyawa M, Oniankitan O, Khan MA (2000) Spondyloarthropathies in sub-Saharan Africa. Curr Opin Rheumatol 12:281–286
Brown MA, Jepson A, Young A, Whittle HC, Greenwood BM, Wordsworth BP (1997) Ankylosing spondylitis in West Africans—evidence for a non-HLA-B27 protective effect. Ann Rheum Dis 56:68–70
Amroun H, Djoudi H, Busson M et al (2005) Early-onset ankylosing spondylitis is associated with a functional MICA polymorphism. Hum Immunol 66:1057–1061
Younsi R, Azrib S, Aitouazar M, Hari WG, El Hassani S (2007) Evaluation de ’incidence du gène HLA-B27 chez le patient attaint de spondlyarthrite ankylosante au Maroc. Revue de Rhumatisme 74:1013
Alonso-Ruiz A, Pijoan JI, Ansuategui E, Urkaregi A, Calabozo M, Quintana A (2008) Tumor necrosis factor alpha drugs in rheumatoid arthritis: systematic review and metaanalysis of efficacy and safety. BMC Musculoskelet Disord 9:52
Braun J, van den Berg R, Baraliakos X et al (2011) 2010 update of the ASAS/EULAR recommendations for the management of ankylosing spondylitis. Ann Rheum Dis 70:896–904
Raychaudhuri SP, Nguyen CT, Raychaudhuri SK, Gershwin ME (2009) Incidence and nature of infectious disease in patients treated with anti-TNF agents. Autoimmun Rev 9:67–81
Bernatsky S, Habel Y, Rahme E (2010) Observational studies of infections in rheumatoid arthritis: a metaanalysis of tumor necrosis factor antagonists. J Rheumatol 37:928–931
Gliklich RE, Dreyer NA et al (2010) Registries for evaluating patient outcomes: a user’s guide. Agency for Healthcare Research and Quality (US), Rockville
Singh JA, Wells GA, Christensen R et al (2011) Adverse effects of biologics: a network meta-analysis and Cochrane overview. Cochrane Database Syst Rev: CD008794
Dixon WG, Symmons DPM, Lunt M et al (2007) Serious infection following anti-tumor necrosis factor α therapy in patients with rheumatoid arthritis: lessons from interpreting data from observational studies. Arthritis Rheum 56:2896–2904
United Nations (2009) Tuberculosis prevalence rate per 100,000 population (mid-point) http://data.un.org/Data.aspx?d=MDG&f=seriesRowID%3A617. Accessed 26 Apr 2012
Dabbous O, Gilmer K, Tatsuki Y et al (2007) Tuberculosis in Japanese patients with rheumatoid arthritis treated with infliximab: findings from the post marketing surveillance trial. 2007 Annual ACR Meeting
Komano Y, Tanaka M, Nanki T et al (2011) Incidence and risk factors for serious infection in patients with rheumatoid arthritis treated with tumor necrosis factor inhibitors: a report from the Registry of Japanese Rheumatoid Arthritis Patients for Longterm Safety. J Rheumatol 38:1258–1264
National Technic Steering Group of the Epidemiological Sampling Survey for Tuberculosis, Duanmu H (2002) [Report on fourth national epidemiological sampling survey of tuberculosis]. Zhonghua Jie He He Hu Xi Za Zhi 25:3–7
Hu DW, Bao CD, Chen SL et al (2005) Treatment of rheumatoid arthritis with a recombinant human tumor necrosis factor-Fc fusion protein: a multicenter, randomized, double blind, controlled trial. Chin J Rheumatol 9:664–668
Hou Y, Zhang FC, Huang F et al (2005) Infliximab versus placebo in rheumatoid arthritis receiving concomitant methotrexate: a randomized double blind phase III trial in China. Chin J Rheumatol 10:658–663
Huang F, Wang L, Zhang J, Deng X, Guo J, Zhang Y (2006) Risk of tuberculosis in a Chinese registry of rheumatoid arthritis and ankylosing spondylitis for tumour necrosis factor-α antagonists. APLAR J Rheumatol 9:170–174
Huang F, Zhang FC, Bao CD et al (2009) Adalimumab plus methotrexate for the treatment of rheumatoid arthritis: a multi-center randomized, double-blind, placebo-controlled clinical study. Zhonghua Nei Ke Za Zhi 48:916–921
Tam LS, Leung CC, Ying SK et al (2010) Risk of tuberculosis in patients with rheumatoid arthritis in Hong Kong—the role of TNF blockers in an area of high tuberculosis burden. Clin Exp Rheumatol 28:679–685
Wang LS, Huang F, Zhang JL et al (2007) A cohort analysis of safety tumor necrosis factor- antagonists in the treatment of Chinese patients with ankylosing spondylitis. Chin J New Drugs 16:556–561
Chen DY, Chou SJ, Hsieh TY et al (2009) Randomized, double-blind, placebo-controlled, comparative study of human anti-TNF antibody adalimumab in combination with methotrexate and methotrexate alone in Taiwanese patients with active rheumatoid arthritis. J Formos Med Assoc 108:310–319
Chen DY, Shen GH, Hsieh TY, Hsieh CW, Lan JL (2008) Effectiveness of the combination of a whole-blood interferon-gamma assay and the tuberculin skin test in detecting latent tuberculosis infection in rheumatoid arthritis patients receiving adalimumab therapy. Arthritis Rheum 59:800–806
Chen DY, Shen GH, Hsieh TY, Hsieh CW, Lan JL (2012) Biphasic emergence of active tuberculosis in rheumatoid arthritis patients receiving TNF{alpha} inhibitors: the utility of IFNγ assay. Ann Rheum Dis 71:231–237
Navarra S, Raso AA, Linchauco JJ, Tan P (2006) Clinical experience with infliximab among Filipino patients with rheumatic diseases. Int J Rheumatic Dis 9:150–156
Seong SS, Choi CB, Woo JH et al (2007) Incidence of tuberculosis in Korean patients with rheumatoid arthritis (RA): effects of RA itself and of tumor necrosis factor blockers. J Rheumatol 34:706–711
Kim EM, Uhm WS, Bae SC, Yoo DH, Kim TH (2011) Incidence of tuberculosis among Korean patients with ankylosing spondylitis who are taking tumor necrosis factor blockers. J Rheumatol 38:2218–2223
Suwannalai P, Auethavekiat P, Udomsubpayakul U, Janvitayanujit S (2009) The infectious profiles of anti-tumor necrosis factor agents in a Thai population: a retrospective study a the university-based hospital. Int J Rheum Dis 12:118–124
Kumar A (2006) Experience with anti-tumor necrosis factor-α therapy in India. APLAR J Rheumatol 9:141
Allali F, Rkain H, Faik A, El Hassani S, Hajjaj-Hassouni N (2005) Prevalence and clinical characteristics of tuberculosis in rheumatoid arthritis patients. Clin Rheumatol 24:656–657
El Mansouri L, Bahiri R, Abourazzak FE, Abouqal R, Hajjaj-Hassouni N (2009) Two distinct patterns of ankylosing spondylitis in Moroccan patients. Rheumatol Int 29:1423–1429
Public Health Agency of Canada (2011) International tuberculosis incidence rates. http://www.phac-aspc.gc.ca/tbpc-latb/itir-eng.php. Accessed 17 Jul 2012
Salmon-Ceron D, Tubach F, Lortholary O et al (2011) Drug-specific risk of non-tuberculosis opportunistic infections in patients receiving anti-TNF therapy reported to the 3-year prospective French RATIO registry. Ann Rheum Dis 70:616–623
Galloway JB, Hyrich KL, Mercer LK et al (2011) Anti-TNF therapy is associated with an increased risk of serious infections in patients with rheumatoid arthritis especially in the first 6 months of treatment: updated results from the British Society for Rheumatology Biologics Register with special emphasis on risks in the elderly. Rheumatol (Oxford) 50:124–131
Dixon WG, Hyrich KL, Watson KD et al (2010) Drug-specific risk of tuberculosis in patients with rheumatoid arthritis treated with anti-TNF therapy: results from the British Society for Rheumatology Biologics Register (BSRBR). Ann Rheum Dis 69:522–528
Greenberg JD, Reed G, Kremer JM et al (2010) Association of methotrexate and tumour necrosis factor antagonists with risk of infectious outcomes including opportunistic infections in the CORRONA registry. Ann Rheum Dis 69:380–386
Carmona L, Gómez-Reino JJ, BIOBADASER Group (2006) Survival of TNF antagonists in spondylarthritis is better than in rheumatoid arthritis. Data from the Spanish registry BIOBADASER. Arthritis Res Ther 8:R72
Al-Ghamdi A, Attar SM (2009) Extra-articular manifestations of rheumatoid arthritis: a hospital-based study. Ann Saudi Med 29:189–193
Attar SM, Al-Ghamdi A (2010) Radiological changes in rheumatoid arthritis patients at a teaching hospital in Saudi Arabia. East Mediterr Health J 16:953–957
Kazkaz L, Marotte H, Hamwi M et al (2007) Rheumatoid arthritis and genetic markers in Syrian and French populations: different effect of the shared epitope. Ann Rheum Dis 66:195–201
Winthrop KL (2010) The risk and prevention of tuberculosis: screening strategies to detect latent tuberculosis among rheumatoid arthritis patients who use biologic therapy. Int J Adv Rheumatol 8:43–52
Wallis RS, Ehlers S (2005) Tumor necrosis factor and granuloma biology: explaining the differential infection risk of etanercept and infliximab. Semin Arthritis Rheum 34:34–38
Tubach F, Salmon D, Ravaud P et al (2009) Risk of tuberculosis is higher with anti-tumor necrosis factor monoclonal antibody therapy than with soluble tumor necrosis factor receptor therapy: the three-year prospective French Research Axed on Tolerance of Biotherapies Registry. Arthritis Rheum 60:1884–1894
Acknowledgments
Editorial/medical writing support was provided by WC Hatch at ACUMED and was funded by Pfizer Inc. No financial support was provided to the authors for this work.
Disclosures
Abdurhman Alarfaj has consulted and received honorarium from Pfizer Inc. Mohammed Hammoudeh has consulted for Schering-Plough Corp and consulted and received honoraria from Abbott Laboratories, Pfizer Inc, Roche Pharmaceuticals, and Wyeth Pharmaceuticals. He has received grant/research support from Pfizer Inc, Roche Pharmaceuticals, Schering-Plough Corp, and Wyeth Pharmaceuticals. Ehab Youseif is a Senior Regional Director, Medical Affairs for Pfizer Latin America. Der-Yuan Chen, Hachemi Djoudi, and Jian Zhu declare no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hammoudeh, M., Alarfaj, A., Chen, DY. et al. Safety of tumor necrosis factor inhibitors use for rheumatoid arthritis and ankylosing spondylitis in Africa, the Middle East, and Asia: focus on severe infections and tuberculosis. Clin Rheumatol 32, 293–300 (2013). https://doi.org/10.1007/s10067-012-2137-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-012-2137-7