Abstract
Type B insulin resistance syndrome is characterized by the formation of autoantibodies against insulin receptors, which can cause severe hyperglycemia and insulin resistance. Systemic lupus erythematosus is the most common underlying diseases of the syndrome. This report details our study of a case involving a Chinese female with type B insulin resistance syndrome as well as systemic lupus erythematosus who completely recovered after undergoing immunosuppressive therapy, specifically pulse therapy utilizing intravenous immunoglobulin. We also conducted search in MEDLINE and Chinese BioMedicine database to identify relevant literatures published in the past 46 years. From our searches, six case reports in Chinese, 15 case reports, and a 28-year perspective article in English met our criteria; a total of 67 cases were included in our report. The mean age of subjects at presentation for groups A, B, and C were 42.95, 44.10, and 41.68 years, respectively, yielding no significant difference between these groups. African Americans were the most susceptible group to type B insulin resistance syndrome, followed by Asians representing 20.90 % of all cases. Comparisons between the three main racial groups surveyed indicated that the mean age of subjects at presentation were very contiguous for African Americans and Asians, and mean age of white people was remarkably higher than either of the first two groups. The syndrome appeared most common among Asian males, and white males were relatively less likely to suffer from type B insulin resistance syndrome. Hypoglycemia was most commonly observed in white people than in other racial groups. Hypoalbuminemia, elevated serum immunoglobulin G, and elevated sedimentation rates were more common in African Americans; Asian cases were more likely to show low serum C3 or C4 and nephritis. Two cases received intravenous immunoglobulin therapy, which has a remarkably rapid effect on insulin resistance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Type B insulin resistance syndrome is an autoimmune phenomenon caused by polyclonal immunoglobulin G antibodies that exhibit antagonist activity directed against insulin receptors. A series of autoimmune diseases can induce these autoantibodies and cause type B insulin resistance syndrome [1]. Systemic lupus erythematosus (SLE) is a representative type of systemic autoimmune disease characterized by loss of immunologic self-tolerance and by subsequent development of autoantibodies. A subset of autoantibodies directed against cell surface receptors can cause phenotypic manifestations of the receptor blockade. The best-known examples of these autoantibodies are those to the receptors for acetylcholine (myasthenia gravis) [2], for gonadotropin (ovarian failure) [3], and for insulin (type B insulin resistance). Formation of insulin receptor autoantibodies can cause severe hyperglycemia and insulin resistance, which is known as type B insulin resistance syndrome. Although type B insulin resistance syndrome usually causes hyperglycemia refractory to massive doses of insulin, occasionally, the receptor autoantibodies can have an insulin-like effect, which can bring about life-threatening hypoglycemia [1, 4, 5].
In 2002, Arioglu et al. reported a 28-year perspective of 24 cases with type B insulin resistance syndrome and reviewed 21 similar cases reported [1], which made great progress in understanding type B insulin resistance syndrome. However, the study contained 45 cases that mostly involved African Americans and white people; only one Asian case was studied. Until now, including our case, seven cases of type B insulin resistance syndrome have been reported among Chinese people. Meanwhile, 15 similar cases have been reported worldwide within the last decade. Therefore, it is necessary to carry out a systematic review to ascertain whether any differences exist between Asian cases and African American cases, and whether immunosuppressive therapy is the first choice for all patients. We also wonder if there are any characteristics that could aid in predicting hypoglycemia because of the potentially life-threatening nature of hypoglycemia. We begin with a report on one Chinese case that resulted in a very positive responds to pulse therapy of intravenous immunoglobulin.
Materials and methods
Strategy for literature search
We searched the electronic database MEDLINE (1966 to June 2011), using the Medical Subject Headings terms (MESH) “type B insulin resistance syndrome” or “type B insulin resistance”. We also performed a manual search of major journals and reviewed the reference lists from the articles retrieved. Only those that were published in English as full-length articles were considered. In addition, the Chinese BioMedicine database (1985 to June 2011) was also searched for Chinese articles using the above terms during the same period.
Inclusion and exclusion criteria
For inclusion, studies had to fulfill the following criteria: (1) a type B insulin resistance diagnosis must have been established for every case and (2) the reports included did not have race restriction. Studies were excluded if: (1) cases from reports were published in neither English nor Chinese and (2) review articles. Twenty-one case reports published before 2001 were excluded because the 28-year perspective article had reviewed these cases.
Statistical analysis
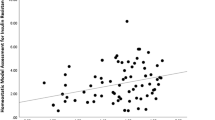
SPSS 17.0 was used for data analysis. Independent samples t test was used for sample comparisons and considered significant at P ≤ 0.05. GraphPad Prism 5 was used for drawing figures.
Study selection and data abstraction
All articles’ abstracts found from electronic database were checked independently by two investigators to select potentially relevant articles based on the inclusion and exclusion criteria. To ensure that all relevant articles would be identified, any article that appeared to be relevant was initially included. Two authors then determined whether articles were eligible for inclusion. We developed a standardized data abstraction form that included relevant information for the studies: country of origin, year of publication, authors, patient demographics, study design, medicine, dosage, duration of treatment, length of follow-up, outcomes, and adverse events.
Case report
A 46-year-old Chinese woman presented and was admitted to our hospital with a 3-month history of general fatigue, decreasing in food appetite, Raynaud phenomenon, and edema in face and extremities. On admission to our hospital, she was afebrile and normotensive and the physical examination revealed facial edema, a dull sound below the seventh rib on the left scapular line, heart limit toward bilateral enlargement, and severe trace edema on lower extremities. The admission laboratory tests were remarkable for the following values: platelet count of 57 × 109/L, plasma albumin of 24.6 g/L, plasma globulin of 37.8 g/L, fasting blood glucose of 14.5 mmol/L, postprandial blood glucose of 26.5 mmol/L, erythrocyte sedimentation rate of 51 mm/h, C-reactive protein of 2.89 mg/L↑, C3 of 0.138 g/L↓, C4 of <0.0147 g/L↓, endogenous creatinine clearance rate of 57.27 ml/min, and quantitation of 24 h proteinuria of 1.15 g. Urine ketones and urine occult blood were positive. Antinuclear antibody, antinuclear ribonuclear protein antibody, and anti-SM were positive. Anti-insulin antibody was negative, anti-insulin receptor antibody was not tested because of technical limitations.
Based on clinical presentation and laboratory findings, SLE was easily diagnosed. Pulse therapies with intravenous cyclophosphamide (CYC) and intravenous methylprednisolone were administered due to high disease activity. Meanwhile, insulin therapy was initiated and increasingly added to the doses of 600 unit/day (Fig. 1). The patient presented severe resistance to insulin therapy and her unique response was urine ketones becoming negative. As last choice, pulse therapies with intravenous immunoglobulin were added. The severe insulin resistance disappeared suddenly and hyperglycemia could be controlled with a normal dose of insulin within 1 week after intravenous immunoglobulin treatments. She completely recovered from the syndrome in 6 weeks after intravenous immunoglobulin treatments. If no contraindication occurred, a pulse therapy with intravenous CYC (800 mg) would be administrated monthly a total of six times. Thereafter, leflunomide would be administered as maintenance therapy. Abnormal laboratory findings gradually became normal in 7 months from initiation of treatment. Hyperglycemia and hypoglycemia never recurred during this 2-year follow-up period.
Hyperglycemia significantly correlating with SLE activity and dramatically responding to intravenous immunoglobulin indicated that the insulin resistance syndrome was related to autoimmunity. The minimal response to insulin therapy was not accordant with features of latent autoimmune diabetes in adults, which have characteristics of both type 1 (autoimmune in nature) and type 2 diabetes (initial response to oral hypoglycemic agents) [6]. Insulin autoimmune syndrome and type B insulin resistance syndrome are both autoimmune-mediated insulin resistances. Opposed to type B insulin resistance syndrome, insulin autoimmune syndrome is diagnosed by the presence of antibodies to insulin and hyperglycemia caused by these antibodies [7]. In our case, the autoantibodies against insulin were negative. Moreover, treated with a huge amount of insulin, there must be huge amounts of autoantibodies to bind exogenous insulin and when the amount of exogenous insulin overwhelmed the autoantibodies, the insulin resistance should disappear. Therefore, we could confirm that the insulin resistance did not result from insulin autoimmune syndrome but type B insulin resistance syndrome, although tests were not performed on insulin receptor antibodies.
Results
Results of search strategy
In the end, six case reports in Chinese, 15 case reports, and a 28-year perspective article in English met our criteria; a total of 67 cases were included.
General information of cases and comparison between three groups
Three subsets of cases and up to 67 cases, including our case were included in this review. Of the two groups from the Arioglu et al.’s study, we arbitrarily named the perspectively monitored group “Group A” and the reviewed group “Group B”. The third group comprised reviewed cases during the past decade and was named “Group C”. Table 1 presented general information related to Group C and a comparison of the groups. The majority of patients were female in all three cohorts. The mean age of subjects at presentation for groups A, B, and C were 42.95, 44.10, and 41.68 years, respectively. There was no significant difference between these groups. In group A, acanthosis nigricans was more common than in other groups, and African Americans were the majority. Compared to group A, acanthosis nigricans was less observed, hypoglycemia was most common, and Asians were majority in group C. Amount of insulin used in group A was higher than in group C. For all three groups, SLE was main underlying disease and was more common in group A.
Constituent ratio of racial groups and comparison of three main racial groups involved in the syndrome
Table 2 indicated race and gender of all cases. African American was the most susceptible group to type B insulin resistance syndrome, followed by Asian representing 20.90 % of all cases. White people was in the third place and white males less likely suffered from the syndrome (nine of the cases were not categorized by race due to insufficient data). Comparisons between the three main racial groups indicated that the mean age of subjects at presentation was very contiguous for African Americans and Asians, and was remarkably higher in white people than in the other two groups. Asian males were more likely and white males were less likely involved in type B insulin resistance syndrome. Hypoglycemia was more common in white people than in other racial groups. The rates of complicating acanthosis nigricans were very similar among the three groups (Table 3).
Underlying diseases and systemic features of the syndrome
SLE was the most common underlying disease, which appeared in 62.9 % of all cases (Table 4). Underlying diseases for 10 of the cases (14.93 %) were unknown because of insufficient data. Surprisingly, one case had neither underlying disease nor acanthosis nigricans (Table 4). Nonspecific “autoimmune” features were common in almost all cases. Comparing Asian cases with group A (predominantly African American), hypoalbuminemia, elevated serum immunoglobulin G (IgG), and elevated sedimentation rate were more common in group A, but low serum C3 or C4 and nephritis were more likely observed in Asian cases. Group B was a mix of white people, African Americans, Asians, Hispanics and seven cases with unreported races. Leukopenia was less common in group B than in Asian cases and group A, elevated sedimentation rate and elevated serum IgG were more common in group B (Table 5).
Treatments with intravenous immunoglobulin
Including our case, two cases received intravenous immunoglobulin treatments. In our case, hyperglycemia could be controlled with normal doses of insulin within 1 week of intravenous immunoglobulin treatments (Fig. 1). In the other case, when treated with intravenous immunoglobulin 0.4 g/kg/day, the severe insulin resistance disappeared overnight followed by moderate hypoglycemia (Fig. 2).
Discussion
Type B insulin resistance syndrome is an extremely rare disease. Until now, only 67 cases have been reported worldwide. Most of them are case reports; only three articles try to use limited information to identify the clinical feature of the syndrome. The first one was the 28-year perspective of 24 cases with type B insulin resistance syndrome. As mentioned previously, this paper reported 24 cases and reviewed 21 similar cases reported before 2001 [1], indicating 88 % of the 24 cases were African American and 87.5 % of these cases suffered from acanthosis nigricans, which remarkably differed from our findings. The second one reported autoimmune forms of hypoglycemia [7] and compared type B insulin resistance syndrome with insulin autoimmune syndrome, indicating both the syndrome could cause hyperglycemia and hypoglycemia. However, hypoglycemia was less common in type B insulin resistance syndrome than in insulin autoimmune syndrome and insulin, C-peptide and proinsulin levels in insulin autoimmune syndrome were extremely high, much higher than in type B insulin resistance syndrome. Our case presented severe hyperglycemia and slight hypoglycemia. Insulin autoantibodies were negative, easily differing from insulin autoimmune syndrome. The third one focused on seven patients treated with an intensive combination protocol of rituximab, cyclophosphamide, and pulse corticosteroids [8] aimed at control of pathogenic autoantibody production. Remission was achieved on average in 8 months from initiation of treatment, which much longer than our case treated with pulse therapy of intravenous immunoglobulin.
Type B insulin resistance syndrome often onsets in adulthood, especially in fertile women, which is consistent with the features of systemic autoimmune diseases, but there is an exception that a 1-year old child was reported suffering [1]. Besides one case from Korea, remainders were largely accompanied with autoimmune diseases. SLE was the most commonly observed underlying diseases for all cases of various races, representing 62.69 % of all cases according to our findings. As a representative autoimmune disease, SLE is characterized by the production of autoantibodies to components of various cell nucleus and cell membrane proteins, which is related to diverse clinical manifestations encompassing almost all organ systems. In addition to SLE, other systemic autoimmune disorders such as Sjögren’s syndrome, dermatomyositis, and scleroderma, among others, could also induce autoantibodies against insulin receptors and result in type B insulin resistance syndrome [1]. Except for systemic autoimmune disease, autoimmune thyropathy (autoimmune thyroiditis, Graves’ disease, and primary hypothyroidism), Hodgkin disease, myeloma, HIV, and chronic active hepatitis are the less common underlying diseases [1]. Interestingly, an elderly Korean woman with neither a history of autoimmune disease nor the clinical features of acanthosis nigricans suffered from type B insulin resistance syndrome that manifested as diabetic ketoacidosis with autoantibodies against both insulin and insulin receptors [9]. Generally, these cases occurred when the underlying diseases such as SLE are at a high activity, but Coll et al. reported a woman with otherwise clinically quiescent SLE in whom euglycemia was restored after plasmapheresis and immunosuppressive therapies [10].
By comparing 22 cases of the last decade with two groups from the perspective study, it is clear that more Asian cases were reported, hypoglycemia were more common and acanthosis nigricans was less complicated in group C (mainly Asian). The average doses of insulin needed in group C was 3,542.67 units per day, which was lower than in group A (almost African American). The results may be biased by selected reporting of the cases and excluding articles written in languages other than English and Chinese. As shown in Table 1, African American females were the most susceptible to type B insulin resistance syndrome followed by Asian females and white females. We arbitrarily chose to study these three racial groups separately and compared them with each other to illuminate the differences between them. The average age of subjects at presentation in white people were obviously higher than in other two groups. Asian males were more likely and white males were less likely to develop type B insulin resistance syndrome. White people were most susceptible to hypoglycemia. The rates of complicating acanthosis nigricans were very similar among the three groups. These features should be considered when encountering this sort of cases during clinical practice.
Type B insulin resistance syndrome is characterized by the presence of circulating anti-insulin receptor antibodies and severe hyperglycemia. By preventing insulin from binding to insulin receptors, decreasing the number of insulin receptor and desensitizing insulin receptors, these autoantibodies downregulate insulin receptors to decreased insulin signal transduction through insulin receptors, in which case the autoantibodies can cause severe insulin resistance [1]. Insulin resistance can be so severe that amounts of up to 30,000 units of exogenous insulin per day may still be ineffective for controlling hyperglycemia [11]. Interestingly, besides hyperglycemia, insulin receptor antibodies can also cause hypoglycemia by acting as agonists of the insulin receptors [2, 5, 7]. Furthermore, immunosuppressive treatments reduce the number of anti-insulin receptor autoantibodies, making receptors available for large amounts of circulating insulin. If patients have a very quick responds to violent immunosuppressive treatments, patient may develop severe hypoglycemia, which can be life threatening. Our results indicate that 25.37 % of all cases experienced hypoglycemia, most of whom first experienced hyperglycemia and developed severe hypoglycemia later in the course of their illness. A few of these cases suffered from hypoglycemia without any notable incidence of hyperglycemia at first and developed hyperglycemia later.
The diagnosis of type B insulin resistance syndrome is based largely on the findings of hyperglycemia, underlying autoimmune diseases, hyperinsulinemia, and the presence of insulin receptor antibodies. In practice, type B insulin resistance is diagnosed mainly by evaluating clinical presentations and ruling out other causes of insulin resistance. Assays for antibodies against insulin receptor can confirm the diagnosis but are currently not commercially available. Insulin receptor antibody assays have technical limitations. Therefore, if insulin receptor antibodies are detected with one assay, the negative result does not rule out the possibility that the patient has clinically significant insulin receptor antibodies. In addition to the multiple clinical manifestations of underlying systemic diseases, the clinical course of patients with type B insulin resistance syndromes is variable. Some patients will experience a spontaneous remission but the duration of remission and probability of flare up are unpredictable. Some patients have a biphasic course, involving a phase of severe insulin resistance and hyperglycemia followed by a hypoglycemic phase [1, 7]. Therefore, diagnosis should be established by a comprehensive evaluation of the clinical presentation. Refractory hyperglycemia and hypoglycemia occurring without apparent reason are both possible indications of type B insulin resistance syndrome [7].
The initial goal when treating patients with type B insulin resistance syndrome is to manage their hyperglycemia and this generally requires large amounts of insulin. We suggest that insulin be given intravenously and generously (our recommendation is without limit) due to the fact that the half-life period of insulin is between 5 and 15 min and that large amounts of insulin can be decomposed quickly in the body with subsequent loss of its biological effect. In this review, 39 cases received insulin therapy and the mean amount of insulin was 4,501.02 units per day. However, when insulin antibodies are present, insulin should be administered very carefully to avoid inducing hypoglycemia [7]. Insulin antibodies can bind insulin and inhibit insulin clearance, thus causing large amounts of insulin to accumulate in the body. Occasionally, insulin antibodies releasing large amounts of insulin can cause severe hypoglycemia when violent immunosuppressive agents are administered.
Because type B insulin resistance syndrome associates with a series of diseases (usually connective tissue diseases), treatments are mainly aimed at the underlying disease. A variety of immunosuppressive agents—including glucocorticoids, cyclophosphamide, azathioprine, ciclosporin A, rituximab, leflunomide, mycophenolate mofetil, intravenous immunoglobulin, and plasmapheresis—are used to induce remission [1, 8]. In many cases, patients were treated with a combination of immunosuppressive therapies, making it difficult to identify which treatment was most effective. Treatment strategies should, therefore, be individualized and based on the requirements of the medical setting. Generally, glucocorticoids (oral or intravenous) are the fundamental treatment. For severe cases, intravenous methylprednisolone and cyclophosphamide are recommended. Plasmapheresis has been used in approximately 10 cases with various responses. For some cases, plasmapheresis had a rapid effect and was recommended for patients with very high titers of insulin receptor autoantibodies [1, 8, 11, 12]. However, plasmapheresis has poor long-term efficacy, so combining this treatment with other immunosuppressive agents is needed [1]. For patients who respond poorly to glucocorticoids and immunosuppressive agents, rituximab (an anti-CD 20 monoclonal antibody) is recommend in combination with cyclophosphamide and pulse corticosteroids to form a standardized treatment that remarkably reduced pathogenic autoantibody production and resulted in remission of the disease in seven cases [8, 13]. Intravenous immunoglobulin is extremely effective for rapidly reducing the amount of insulin and eliminating insulin resistance [14]. Although it was used only in two cases, its effect was remarkable (Figs. 1 and 2). Meanwhile, it is usually effective for some refractory systemic autoimmune diseases. Therefore, intravenous immunoglobulin with fewer contraindications is a strong candidate for a first-line drug in treating type B insulin resistance syndrome.
Conclusion
Type B insulin resistance syndrome is an autoimmune disorder. Presence of circulating anti-insulin receptor antibodies and severe hyperglycemia are both main characteristics. African American female predominance, often onset in adulthood, an association with other autoimmune diseases, and acanthosis nigricans are all clinical features. Asians are the second most likely racial group to suffer from the syndrome and Asian males are more likely to have the syndrome than other racial males. SLE is the most common underlying disease. Prognosis of type B insulin resistance syndrome largely depends on the underlying disease. Immunosuppressive therapy is the most commonly used treatment and is effective for most cases. As treatments, rituximab and plasmapheresis both have benefits and detriments. Intravenous immunoglobulin is strongly recommended for refractory patients in order to rapidly mitigate severe insulin resistance. We suggest that diagnosis of type B insulin resistance syndrome should be considered even if other features of active autoimmune processes are absent and autoantibodies against insulin receptors are undetected in the first assay when patients have severe insulin resistance. Successful treatment is possible for type B insulin resistance syndrome. Clinical physicians should note that exceptions exist: a patient can suffer from type B insulin resistance without any known related diseases accompanying the symptoms [9].
Limitations
(1) Report bias: as in all observational studies, the possibility of bias and confounding cannot be completely excluded. (2) Missing data from reports selected may decrease the accuracy of our results. (3) Only reported cases were included in our systematic analysis; therefore, publication bias may have occurred.
References
Arioglu E, Andewelt A, Diabo C, Bell M, Taylor SI, Gorden P (2002) Clinical course of the syndrome of autoantibodies to the insulin receptor (type B insulin resistance): a 28-year perspective. Medicine (Baltimore) 81(2):87–100
Gorden P, Collier E, Roach P (1993) Autoimmune mechanisms of insulin resistance and hypoglycemia. In: Moley DE (ed) Insulin resistance. Wiley, London, pp 123–142
Sluss PM, Schneyer AL (1992) Low molecular weight follicle-stimulating hormone receptor binding inhibitor in sera from premature ovarian failure patients. J Clin Endocrinol Metab 74:1242–1246
De Pirro R, Roth RA, Rossetti L, Goldfine ID (1984) Characterization of the serum from a patient with insulin resistance and hypoglycemia. Evidence for multiple populations of insulin receptor antibodies with different receptor binding and insulin-mimicking activities. Diabetes 33:301–304
Di Paolo S, Giorgino R (1991) Insulin resistance and hypoglycemia in a patient with systemic lupus erythematosus: description of antiinsulin receptor antibodies that enhance insulin binding and inhibit insulin action. J Clin Endocrinol Metab 73:650–657
Qi X, Sun J, Wang J, Wang PP, Xu Z, Murphy M, Jia J, Wang J, Xie Y, Xu W (2011) Prevalence and correlates of latent autoimmune diabetes in adults in Tianjin, China: a population-based cross-sectional study. Diabetes Care 34(1):66–70
Lupsa BC, Chong AY, Cochran EK, Soos MA, Semple RK, Gorden P (2009) Autoimmune forms of hypoglycemia. Medicine (Baltimore) 88(3):141–153
Malek R, Chong AY, Lupsa BC, Cochran EK, Soos MA, Semple RK, Balow JE, Gorden P (2010) Treatment of type B insulin resistance: a novel approach to reduce insulin receptor autoantibodies. J Clin Endocrinol Metab 95(8):3641–3647
Joung KH, Kim HJ, Ku BJ (2012) Type B insulin resistance syndrome with diabetic ketoacidosis. Acta Diabetol 49(1):81–82
Coll AP, Morganstein D, Jayne D, Soos MA, O’Rahilly S, Burke J (2005) Successful treatment of type B insulin resistance in a patient with otherwise quiescent systemic lupus erythematosus. Diabet Med 22(6):814–815
Page KA, Dejardin S, Kahn CR, Kulkarni RN, Herold KC, Inzucchi SE (2007) A patient with type B insulin resistance syndrome, responsive to immune therapy. Nat Clin Pract Endocrinol Metab 3(12):835–840
Eriksson JW, Bremell T, Eliasson B, Fowelin J, Fredriksson L, Yu ZW (1998) Successful treatment with plasmapheresis, cyclophosphamide, and cyclosporin A in type B syndrome of insulin resistance. Case report. Diabetes Care 21(8):1217–1220
Coll AP, Thomas S, Mufti GJ (2004) Rituximab therapy for the type B syndrome of severe insulin resistance. N Engl J Med 350(3):310–311
Tran HA, Reeves GE (2009) Treatment of type B insulin resistance with immunoglobulin: novel use of an old therapy. Med J Aust 190(3):168
Gehi A, Webb A, Nolte M, Davis J Jr (2003) Treatment of systemic lupus erythematosus-associated type B insulin resistance syndrome with cyclophosphamide and mycophenolate mofetil. Arthritis Rheum 48(4):1067–1070
Fareau GG, Maldonado M, Oral E, Balasubramanyam A (2007) Regression of acanthosis nigricans correlates with disappearance of anti-insulin receptor autoantibodies and achievement of euglycemia in type B insulin resistance syndrome. Metabolism 56(5):670–675
Nagayama Y, Morita H, Komukai D, Watanabe S, Yoshimura A (2008) Type B insulin resistance syndrome induced by increased activity of systemic lupus erythematosus in a hemodialysis patient. Clin Nephrol 69(2):130–134
Daniel AL, Houlihan JL, Blum JS, Walsh JP (2009) Type B insulin resistance developing during interferon-alpha therapy. Endocr Pract 15(2):153–157
Ostwal V, Oak J (2009) Type B insulin resistance in a systemic lupus erythematosus patient. Int J Rheum Dis 12(2):174–176
Jeong KH, Oh SJ, Chon S, Lee MH (2010) Generalized acanthosis nigricans related to type B insulin resistance syndrome: a case report. Cutis 86(6):299–302
Mohammedi K, Roussel R, El Dbouni O, Potier L, Abi Khalil C, Capel E, Vigouroux C, Caron-Debarle M, Capeau J, Marre M (2011) Type B insulin resistance syndrome associated with an immune reconstitution inflammatory syndrome in an HIV-infected woman. J Clin Endocrinol Metab 96(4):E653–E657
Sato N, Ohsawa I, Takagi M, Gohda T, Horikoshi S, Shirato I, Yamaguchi Y, Tomino Y (2010) Type B insulin resistance syndrome with systemic lupus erythematosus. Clin Nephrol 73(2):157–162
Kawashiri SY, Kawakami A, Fujikawa K, Iwamoto N, Aramaki T, Tamai M, Nakamura H, Origuchi T, Ida H, Eguchi K (2010) Type B insulin resistance complicated with systemic lupus erythematosus. Intern Med 49(5):487–490
Bao S, Root C, Jagasia S (2007) Type B insulin resistance syndrome associated with systemic lupus erythematosus. Endocr Pract 13(1):51–55
Disclosures
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhang, S., Wang, G. & Wang, J. Type B insulin resistance syndrome induced by systemic lupus erythematosus and successfully treated with intravenous immunoglobulin: case report and systematic review. Clin Rheumatol 32, 181–188 (2013). https://doi.org/10.1007/s10067-012-2098-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-012-2098-x