Abstract
This study was conducted to assess ultrasound (US) and clinical changes of Baker’s cyst (BC) of patients with knee osteoarthritis (OA) after steroid injection. Patients with knee OA complicated with symptomatic BC (40) were treated with US-guided direct (posterior) aspiration. The injection of 40 mg triamcynolone acetonide was in 20 patients direct into the BC and in other 20 subjects intra-articular (anterior). BC diameters (longitudinal, transverse, and thickness) were measured and followed up with US at baseline, 2, 4, and 8 weeks after injection. Swelling, pain, and range motion were scored at clinical examination with Rauschning and Lindgren classification (RLC, since 0 normal to 3 maximal signs). All US measures of BC and RLC significantly decreased after treatment, in comparison to baseline (p < 0.001) and during the follow-up, did not change through the time (no significant difference between 2, 4, and 8 weeks). At 4 and 8 weeks, diameters measured at US are lower when BC is directly infiltrated in comparison to intra-articular injection (p < 0.01). US steroid direct injection reduces US measures and clinics of BC in knee OA, in particular, when steroid is directly infiltrated into BC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Popliteal synovial cyst was originally described by Adams [1] and associated to intra-articular disease by Baker [2], as an enlarged gastrocnemius–semimembranosus bursa situated beneath the inner head of gastrocnemius, with valve connection to knee. Baker’s cyst (BC) is difficult to recognize with clinical examination and may be confused with fat tissue, popliteal artery aneurysms, thrombophlebitis, or tumors [3].
Usually, BC complicates knee osteoarthritis (OA) [4], rheumatoid arthritis [5, 6], and athletic traumatic injuries [7]. Intra-articular steroid injection improves clinics of BC and might avoid consequences, such as rupture, pseudotrombophlebitis, and posterior tibial nerve entrapment [8, 9], while surgical excision is followed by relapses or persistence of symptoms [10] and arthroscopy cannot completely remove BC [11].
Ultrasound (US) allows the identification and differential diagnosis of BC [9, 12, 13], correlating with arthrography [14] and magnetic resonance (100% of accuracy) [15]. US is used to assist needle positioning within the selected target area and to facilitate aspiration of synovial fluid and intra-articular treatments [16] and is more rapid, not invasive, and low-cost procedure than the arthrography previously employed for guide injections [17], while without guide, an inaccurate replacement of steroid has shown in more than 50% of cases [18] with significant consequences on the outcome of the procedure [19]. US might be useful also in BC aspiration and infiltration, even if, until now, no other studies on BC injection under US guidance were conducted.
The aim of this prospective study was to evaluate the efficacy of steroid injection in BC of OA patients, with US and clinical examination. As secondary item, we compared the direct injection into BC and intra-articular infiltration of steroids.
Patients and methods
Since October to December 2009, 200 consecutive patients, attending our outpatient clinic of Division of Rheumatology, with clinical and radiographic criteria of the American College of Rheumatology for knee OA [20], symptomatic and not responsive to nonsteroidal anti-inflammatory drugs (NSAIDs) and analgesic treatment, were examined with US of popliteal fossa to evaluate the presence of BC. Ethical local committee approval was obtained.
Patients affected by other rheumatologic disorders, in particular, with rheumatoid arthritis, spondiloarthritis, and crystal-associated arthritis, or systemic active infective disorders or tumors, or treated with knee surgery intervention or with other steroid injection (in the last 6 months) have been excluded. Systemic steroid treatment and NSAIDS were washed out 2 weeks before the injection. Except for local application of ice, no other treatments (steroids, NSAIDs, and joint injections) were employed during follow-up.
At US, BC were measured in mm of maximal longitudinal diameter (in longitudinal scan), thickness and transversal diameter (both in transversal scan) and classified according to morphological classification (beak, X, grape, slit-shaped) [21] and to US content.
In 48 patients, BC was found at US but 8/48 have not been included in the study (two, one, and three for co-morbidity with rheumatoid-, psoriatic, and crystal-associated arthritis, respectively, and two for previous surgery intervention).
Patients (40) were enrolled, signed informed consensus and treated with aspiration of BC fluid, under US guidance of needle course in soft tissue and in aseptic conditions (sterile swab, US gel, and film on US probe), and injection of 40 mg triamcynolone acetonide in 20 patients (Group 1) directly into BC (posterior) and in 20 subjects (Group 2) inside the joint (anterior). The two groups had similar demographic characteristics (Group 1: 64 ± 9 years old, 11 female, 9 male, BMI BMI 21 ± 2; Group 2: 61 ± 10 years old, 10 female, 10 male, BMI 22 ± 2.7). The radiological score was evaluated with Kellgren e Lawrence score (KL) [22]. Knee effusion was also evacuated.
Major (death, hospitalization, systemic infection, syncope) and minor adverse events (local skin reaction or hematoma, ice burn, resistant pain over 24 h after injection, sickness, dizziness) were registered during follow-up.
US (Logic 5 General Electric US 7.5–12 MHz linear probe) and clinical examination of the affected knee were carried out by two rheumatologists (FB, RF) at baseline and at follow-up (2, 4, and 8 weeks).
Interobserver reliability was established in all US independent and consecutive BC measures of patients made by the two sonographers (F.B. and R.F.), unaware of previous examination. Patients did not look at US screen, during examination. For assessing the intra-observer variability, all patients and controls were examined twice by the first observer.
At clinical examination, patients were scored with Rauschning and Lindgren classification (RLC), as previously showed in other studies for BC [10, 11]:
-
0 score: No pain in the popliteal fossa and swelling, normal range motion (measured with goniometer)
-
1: Swelling and pain after hard exercise with minimal reduction of range motion
-
2: Swelling and pain after soft exercise with reduction of range motion < 20°
-
3: Swelling and pain at rest with reduction of range motion > 20°
We measured also pain with visual analogical scale (VAS 0–10), at baseline and at 8 weeks.
Power statistic and statistical analysis
The primary objective of the study was to verify with US the efficacy of steroid injection in BC of OA patients. On the basis of a previous work of Acebes that evaluated efficacy of steroid intra-articular injection (without aspirating directly the BC) in 30 patients with BC at 4 weeks [23], we considered the number of 40 patients appropriate for this study, with a statistical Power of 50% (with an estimated alpha error of 7.5%).
As the primary outcome, the differences in clinical and US parameters between the baseline and the follow-up at 2, 4, and 8 weeks were evaluated using the Friedman not parametric test.
As secondary item, we examined the discrepancies between the two groups (direct into BC vs. intra-articular injection of steroid) without parametric Mann–Whitney test.
The interobserver and intra-observer variability was measured using the intra-class correlation coefficient (ICC).
Results
The 40 patients enrolled (62 ± 10 years old: range 43–82, 21 women, and 19 men; BMI 22.2 ± 2.6, 37 KL2, and 3 KL3 radiological scores) were successfully injected, without any major or minor adverse events defined in methods.
All BC were positioned in medial popliteal area, between deep fascia and medial head of gastrocnemius muscle and only in one case, between soleus and medial head of gastrocnemius.
In all patients and all times, the intra-reader (mean ICC = 0.98, with confidence interval [95%] = 0.92–0.99) and inter-reader (mean ICC 0.98 with confidence interval [95%] = 0.91–0.99) variability of BC measures resulted low.
Clinical and US follow-up after injection
All patients were evaluated clinically and with US after injection at 2, 4, and 8 weeks, without any interruption at follow--up (Table 1).
At baseline, the BC US morphology was shaped like: beak (34/40), grape (4/40), and slit (2/40). The content of BC was homogeneously anechoic in 35/40 patients; only, in 3/40 and 2/40 patients showed minimal hyperechoic elements and synovial hypertrophy, respectively. The amount of fluid aspirated from BC was 5 ± 4 (range 2–10) ml.
Synovial fluid analysis excluded the presence of monourate and calcium pyrophosphate crystals and revealed a cell count lower than 2000 cells/mm3 in all patients enrolled. No other analysis on fluid were performed.
The communication between cyst and joint was found in all cases. No power Doppler signal was found inside the cyst and the Doppler analysis excluded vein (tromboflebitis) and artery (stenosis) disease-associated.
The US and clinical BC measures significantly decreased in all times at follow-up after injection when compared to baseline (p < 0.001). Also, pain VAS was significantly reduced from baseline (5.8 ± 3.1) to 8 weeks of follow-up (1.5 ± 1) (p < 0.001).
At week 2, we observed the maximal reduction of US BC size and change of morphology (slit shaped in 27/40 patients). At weeks 4 and 8, US and clinical parameters remained stable without significant difference in comparison to week 2. Only morphology parameters changed: slit-shaped BC decreased (at weeks 4 and 8, 19/40 and 17/40 patients, respectively) and beak increased (at weeks 4 and 8, 21/40 and 23/40 patients, respectively), while grape BC did not rebind. The very limited number of grape-slit BC (4/40 at baseline) did not permit them to be a morphology predictive for positive outcome.
Comparison between the two groups
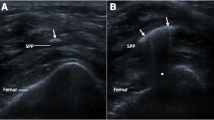
At week 2, clinical and US findings were similar between the two groups, but, successively at follow-up, RLC and BC transverse diameter and thickness (p < 0.01) were significantly lower when BC were directly injected (Group 1) than in intra-articular infiltration (Group 2; Fig. 1).
Discussion
Our data clearly show that the US-guided BC aspiration and the steroid injection are useful, and safe treatments for BC in knee OA, overall, when BC is directly infiltrated. Previous studies support the beneficial effects of intra-articular corticosteroid injections in OA, providing significant pain relief and improving of joint function, especially during inflammatory flares [24–26].
The only previous analogue issue evaluated the efficacy of traditional intra-articular injection of steroids and showed similar results in terms of improvement of BC US and clinical parameters [23], but with a lower significance of decrease of US measures after treatment in comparison to our results. Intra-articular injections of steroids improve symptoms associated to BC by reducing intra-cavitary pressure that is the principal cause of its growth, and the authors of this study also hypothesized that the distribution of the drug from the cavity was facilitated by the same valvular mechanism which might let the drug achieve a higher concentration within the cyst.
Our work confirmed these data and demonstrated that a significant improvement in knee pain, swelling, and range of motion accompanied by a decrease in BC dimensions might be obtained by steroid injections. Otherwise, we demonstrated that the direct BC infiltration was more effective than traditional intra-articular treatment, probably because with this technique, steroid reached a higher amount inside the cyst, more rapidly.
Furthermore, US guidance might guarantee a higher precision in the injection. In fact, it improves routinely the correctness of positioning of the needle tip, with 96%–100% accuracy in comparison with 50%–60% of unintended extra-articular injection rates of traditional palpation-guided method [19, 27].
Probably, the difference of clinical and US efficacy between these two alternative infiltrative methods might be deeper evaluated in the future, with a higher number of patients, even if it’s difficult to select an homogeneous population to make a sure comparison.
Furthermore, we evaluated BC for a more extensive period of follow-up than Acebes study [23] and US neither clinical examination showed a relapse until 8 weeks; probably a longer-term follow-up might be estimate in other future studies.
In this study, we concluded that US-guided aspiration and steroid injection is an useful and safe treatment of BC in OA patients and that direct steroid injection into BC is more effective than traditional intra-articular infiltration.
Abbreviations
- US:
-
Ultrasound
- BC:
-
Baker’s cyst
- OA:
-
Osteoarthritis
- RLC:
-
Rauschning and Lindgren classification
- KL:
-
Kellgren e Lawrence score
References
Adams R (1840) Arthritis, chronic rheumatic, of the knee joint. Dublin J Med Sci 17:520–522
Baker WM (1877) On the formation of synovial cysts in the leg in connection with disease of the knee joint. St Bartholomew’s Hosp Rep 13:245–261
Moore CP, Sarti DA, Louie JS (1975) Ultrasonic demonstration of popliteal cysts in rheumatoid arthritis. Arthritis Rheum 18:577–580
Fam AD, Wilson SR, Holmberg S (1982) Ultrasound evaluation of popliteal cysts in osteoarthritis of the knee. J Rheumatol 9:428–434
Andonopoulos AP, Yarmenitis SY, Sfountouris H et al (1995) Baker’s cyst in rheumatoid arthritis: an ultrasonographic study with a high resolution technique. Clin Exp Rheumatol 13:633–636
Szer IS, Klein-Gitelman MK, DeNardo BA et al (1992) Ultrasonography in the study of prevalence and clinical evolution of popliteal cysts in children with knee effusions. J Rheumatol 19:458–462
Maffulli N, Regine R, Carrillo F, Minelli S et al (1992) Ultrasonographic scan in knee pain in athlete. Br J Sports Med 26:93–96
Katz RS, Zizic TM, Arnold WP et al (1977) The pseudothrombophlebitis syndrome. Medicine 56:151–164
Handy JR (2001) Popliteal cyst in adults: a review. Semin Arthritis Rheum 31:108–118
Rauschning W, Lindgren PG (1979) Popliteal cysts (Baker’s cysts) in adults, clinical and roentgenological results of operative excision. Acta Orthop Scand 50:583–591
Balconi G, Sansone V, De Ponti A (2001) Popliteal cysts: sonography evaluation after arthroscopic treatment. Radiol Med 101:255–259
Torregiani WC, Al-Isamil K, Munk PL et al (2002) The imaging spectrum of Baker’s cyst. Clin Radiol 57:681–691
Levitin PM (1976) Diagnosis of Baker cyst. JAMA 236:253
Gompels BM, Darlington LG (1982) Evaluation of popliteal cysts and painful calves with ultrasonography: comparison with arthrography. Ann Rheum Dis 41:355–359
Ward EE, Jacobson JA, Fessell DP et al (2001) Sonographic detection of Baker’s cysts: comparison with MR imaging. AJR 176:373–380
Grassi W, Farina A, Filippucci E et al (2001) Sonographically guided procedures in rheumatology. Semin Arthritis Rheum 30:347–353
Bliddal H (1999) Placement of intra-articular injections verified by mini air-arthrography. Ann Rheum Dis 58:641–643
Jones A, Regan M, Ledingham J et al (1993) Importance of placement of intra articular steroid injection. BMJ 307:1329–1330
Eustace JA, Brophy DP, Gibney RP et al (1997) Comparison of the accuracy of steroid placement with clinical outcome in patients with shoulder symptoms. Ann Rheum Dis 56:59–63
Altman R, Asch E, Bloch D et al (1986) Development of criteria for the classification and reporting of osteoarthritis: classification of osteoarthritis of the knee. Arthritis Rheum 29:1039–1049
Helbich TH, Breitenseher M, Trattnig S et al (1998) Sonomorphologic variants of popliteal cysts. J Clin Ultrasound 26:171–176
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteo-arthritis. Ann Rheum Dis 16:494–502
Acebes JC, Sanchez-Pernaute O, Diaz-Oca A et al (2006) Ultrasonography assessment of Baker’s cyst after intra-articular corticosteroid injection in knee osteoarthritis. J Clin Ultrasound 34:113–117
Gaffney K, Ledingham J, Perry JD (1995) Intra-articular triamcynolone hexacetonide in knee osteoarthritis: factors influencing the clinical response. Ann Rheum Dis 54:379–381
Jones A, Doherty M (1996) Intra-articular corticosteroids are effective in osteoarthritis but there are no clinical predictors of response. Ann Rheum Dis 55:829–832
Friedman DM, Moore ME (1980) The efficacy of intraarticular steroids in osteoarthritis: a double blind study. J Rheumatol 7:850–856
Sibbitt WL, Peisajovich A, Michael AA et al (2009) Does sonographic needle guidance affect the clinical outcome of intraarticular injections? J Rheumatol 36:1892–1902
Acknowledgment
We thank Dr. Patrizia Cerboni and Dr. Angela Del Rosso for generous free technical writing assistance. The study was conducted without any funding source public or private, and all authors had not any conflict of interest. Manuscript and all images are original, not previously referred by other editors or published.
Disclosures
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bandinelli, F., Fedi, R., Generini, S. et al. Longitudinal ultrasound and clinical follow-up of Baker’s cysts injection with steroids in knee osteoarthritis. Clin Rheumatol 31, 727–731 (2012). https://doi.org/10.1007/s10067-011-1909-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-011-1909-9