Abstract
To determine serum interleukin-33 (IL-33) levels and their associations with clinical parameters in patients with systemic sclerosis (SSc). Serum IL-33 levels were examined by enzyme-linked immunosorbent assay in 69 patients with SSc and 30 healthy individuals. In a retrospective longitudinal study, sera from 14 patients with SSc were analyzed (follow-up, 1–7 years). Serum IL-33 levels were elevated in SSc patients (261.7 ± 141.9 pg/ml) compared with healthy individuals (174.9 ± 72.4 pg/ml; P < 0.001). Patients with diffuse cutaneous SSc had higher levels of IL-33 (287.5 ± 146.6 pg/ml) than those with limited cutaneous SSc (221.5 ± 126.5 pg/ml; P < 0.05). Pulmonary fibrosis and decreased forced vital capacity were more commonly found in patients with elevated IL-33 levels than in those with normal IL-33 levels. IL-33 levels correlated positively with the extent of skin sclerosis, and inversely with percent predicted forced vital capacity. IL-33 levels were increased in SSc patients and correlated with the extent of skin sclerosis and the severity of pulmonary fibrosis. Therefore, IL-33 possibly plays a role in cutaneous and pulmonary fibrosis in SSc patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Systemic sclerosis (SSc) is a generalized connective tissue disorder characterized by sclerotic changes in the skin and internal organs. In addition, SSc is generally regarded as an autoimmune disorder because of the presence of antinuclear antibodies. Although the pathogenesis of SSc remains unclear, previous studies have suggested that some cytokines or growth factors regulate SSc induction by stimulating the synthesis of extracellular matrix components, injuring the endothelial cells, and modulating the function of leukocytes [1]. These cytokines or growth factors are produced partly by inflammatory cells infiltrating the affected tissues, such as skin or lungs, of SSc patients [1, 2].
An imbalance between T helper (Th)1 and Th2 immune responses is considered to play an important role in autoimmune diseases. Although the Th1/Th2 imbalance in SSc appears to be complicated, SSc is generally a Th2-dominant autoimmune disease. Serum levels of IL-4 and IL-13, both representative Th2 cytokines, are significantly elevated in patients with SSc compared with healthy individuals [3–5]. Furthermore, serum IL-4 levels gradually decrease as skin sclerosis improves [6]. In contrast, serum levels of IL-12, a Th1-inducing cytokine, are lower in the early phase of SSc than those in healthy individuals, but become higher in the late phase of SSc [6]. Lymphocytes from patients with clinically active SSc produce lower amounts of interferon gamma (IFN-γ), a representative Th1 cytokine, than those from patients with clinically stable disease [7]. Consistent with these findings, clinical trials of recombinant IFN-γ in the treatment of SSc revealed that IFN-γ exhibited some beneficial clinical effects [8]. Therefore, a shift from Th2 to Th1 response may be associated with an improvement in SSc.
Interleukin (IL)-33 is a new member of the IL-1 family, which includes IL-18 and IL-1β [9]. IL-33 is expressed on smooth muscle cells, epithelial cells, fibroblasts, keratinocytes, endothelial cells, dendritic cells, and activated macrophages [9, 10]. The receptor for IL-33 is a heterodimer consisting of ST2 and IL-1 receptor accessory protein [11]. ST2, a member of the IL-1 receptor family, is selectively expressed on mast cells and Th2 lymphocytes [9, 11]. Binding of IL-33 to ST2 activates nuclear factor-κB and mitogen-activated protein kinases and strongly induces gene expression of Th2 cytokines such as IL-4, IL-5, and IL-13, thereby enhancing Th2 cell differentiation [9]. IL-33 also plays a role as a chemoattractant for human Th2 cells via ST2 [12]. Recent studies have demonstrated that IL-33 is also expressed in synovial fibroblasts of patients with rheumatoid arthritis [13, 14]. Furthermore, IL-33 administration exacerbates murine collagen-induced arthritis (a model of human rheumatoid arthritis), while mice lacking ST2 develop attenuated collagen-induced arthritis [12]. Consistent with these findings, anti-ST2 antibody treatment significantly reduces the severity of murine collagen-induced arthritis [14]. Thus, IL-33 may play an important role in the pathogenesis of autoimmunity. In the present study, we examined serum IL-33 levels in SSc patients, and evaluated the results with respect to clinical features. In addition, we undertook a retrospective longitudinal study of IL-33 levels in some of these patients to determine the changes in IL-33 over time.
Materials and methods
Patients
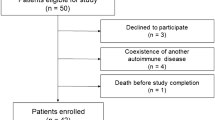
Serum samples were obtained from 69 Japanese patients with SSc (56 women and 13 men; 13–73 years of age (mean, 47 years)). All patients fulfilled criteria for SSc proposed by the American College of Rheumatology [15]. Patients were grouped according to the classification system proposed by LeRoy et al. [16]: 27 patients had limited cutaneous SSc (lSSc) and 42 had diffuse cutaneous SSc (dSSc). Anti-topoisomerase I (topo I) Abs were positive in 27 patients (26 dSSc and one lSSc), anticentromere Abs in 24 (one dSSc and 23 lSSc), anti-RNA polymerase I and III (RNAP) Abs in six (five dSSc and one lSSc), anti-U1RNP Abs in three (one dSSc and two lSSc), anti-U3RNP Abs in one (dSSc); anti-Th/To Abs in one (dSSc), and seven patients had negative results for all these Abs (all dSSc). All patients were 13–73 years of age (mean, 47 years). The median disease duration was 1.9 years (interquartile range (25th–75th percentiles), 1.0–5.0). At the first visit, six patients had been treated with low-dose steroids (prednisolone 5–20 mg/day) and four with low-dose d-penicillamine (100–500 mg/day). None of the patients had received immunosuppressive treatment. Thirty healthy Japanese individuals were included in the study as healthy controls (24 women and six men; 15–71 years of age (mean, 47 years)) and matched SSc patients demographically.
In a retrospective longitudinal study, we analyzed serum samples twice from 14 of the 69 patients with SSc who could be followed longitudinally (13 women and one man). All available patients from whom we were able to collect serum samples twice during the follow-up were examined. The median follow-up period was 3.2 years (interquartile range (25th–75th percentiles), 2.5–4.5). The median disease duration was 2.0 years (interquartile range (25th–75th percentiles), 1.0–3.0). There were seven patients with dSSc and seven with lSSc; anti-topo I Abs were positive in six patients (all dSSc), anticentromere Abs in seven (all lSSc), and anti-RNAP Abs in one (dSSc). These 14 patients were aged 33–76 years (mean, 50 years).
Fresh venous blood samples were centrifuged shortly after clot formation. All samples were stored at −70°C before use.
Clinical assessment
Complete medical history, physical examination, and laboratory tests were conducted for all patients at their first visit, with evaluations especially for pulmonary fibrosis (PF) during follow-up visits. Organ system involvement was defined as described previously [17, 18]: lung = bibasilar fibrosis on chest high-resolution computed tomography; esophagus = hypomotility shown by barium radiography; heart = pericarditis, congestive heart failure, or arrhythmia requiring treatment; kidney = malignant hypertension and rapidly progressive renal failure with no other explanation; and muscle = proximal muscle weakness and elevated serum creatine kinase. PF was defined as bibasilar interstitial fibrosis on high-resolution computed tomography of the chest. In addition, pulmonary function, including forced vital capacity (FVC) and diffusion capacity for carbon monoxide (DLco), was evaluated to examine the severity of PF. When the DLco and FVC were <75% and <80%, respectively, of the predicted normal values, they were considered to be abnormal. SSc patients who were smokers or who had respiratory disorders that could have affected percent predicted DLco or percent predicted FVC were excluded from this study. The modified Rodnan total skin thickness score (TSS) was determined as the sum of the skin thickness measurements, and by palpation on a scale of 0–3 in 17 body areas [19]. The protocol was approved by the Nagasaki University Graduate School of Biomedicinal Sciences and Nagasaki University Hospital, and informed consent was obtained from all patients.
Measurement of serum IL-33
Serum IL-33 levels were measured using specific enzyme-linked immunosorbent assay (ELISA) kits (R&D Systems, Minneapolis, MN, USA), according to the manufacturer’s protocol. Each sample was tested in duplicate and reflected the mean of the two measurements. The intraassay and interassay coefficients of variation in the IL-33 ELISA kit were 7.2% and 7.5%, respectively.
Statistical analysis
The Mann–Whitney U test was used to compare IL-33 levels, Fisher’s exact probability test was used to compare frequencies, and Bonferroni’s test was used for multiple comparisons. Pearson’s correlation coefficient was used to examine the relationship between two variables. Multivariable associations between IL-33 levels in patients with dSSc and those with lSSc with disease duration were assessed using multivariable linear regression. A probability (P) value of <0.05 was considered significant.
Results
Serum IL-33 levels in SSc patients
Serum IL-33 levels were significantly higher in SSc patients (261.7 ± 141.9 pg/ml) than in healthy individuals (174.9 ± 72.4 pg/ml; adjusted P = 0.0008; Fig. 1). IL-33 levels in dSSc patients (287.5 ± 146.6 pg/ml) were significantly higher than in lSSc patients (221.5 ± 126.5 pg/ml; adjusted P = 0.049) or healthy individuals (adjusted P = 0.0002). There was no significant difference in serum IL-33 levels between lSSc patients or healthy individuals.
Serum IL-33 levels in patients with SSc, dSSc, and lSSc, and in healthy individuals (Control). Serum IL-33 levels were determined by a specific ELISA. Horizontal lines indicate the mean value in each group. The dashed line indicates the cut-off value (mean + 2 SD of the values from healthy individuals)
Clinical correlation with serum IL-33 levels
Clinical and laboratory parameters at the first evaluation were compared between SSc patients with elevated IL-33 levels and those with normal IL-33 levels. Values higher than the mean + 2 SD (319.7 g/ml) of the control serum samples were considered to be elevated in this study. Elevated IL-33 levels were observed in 33% (23/69) of all SSc patients, 45% (19/42) of dSSc patients, and 15% (4/27) of lSSc patients. SSc patients with elevated IL-33 levels more frequently had dSSc than those with normal IL-33 levels (83% vs 50%; P < 0.01; Table 1). There was no significant association between IL-33 levels in patients with dSSc and those with lSSc on multivariable analysis correcting for disease duration. Consistent with the association of higher IL-33 levels with dSSc, SSc patients with elevated IL-33 levels had a significantly higher modified Rodnan TSS than those with normal IL-33 levels (16.3 ± 6.6 vs 10.2 ± 5.2; P < 0.05). Furthermore, IL-33 levels correlated positively with modified Rodnan TSS (P < 0.05, r 2 = 0.35; Fig. 2). The prevalence of PF and decreased percent predicted FVC in SSc patients with elevated IL-33 levels was significantly higher than in those with normal IL-33 levels (74% vs 43%, P < 0.01 and 49% vs 21%, P < 0.05, respectively; Table 1). Moreover, IL-33 levels correlated inversely with percent predicted FVC in SSc patients (P < 0.05, r 2 = −0.34; Fig. 2). Thus, IL-33 levels correlated not only with the extent of skin sclerosis but also with the severity of PF in SSc.
Longitudinal study of serum IL-33 levels
To assess changes in serum IL-33 levels over time, serum samples from 14 patients with SSc (seven dSSc and seven lSSc) were analyzed twice over a period of 3.2 years. None of these patients had received any treatment at their first visit. During the follow-up, two of the 14 patients exhibited subacute deterioration of interstitial pneumonitis and received cyclophosphamide pulse therapy. After the initial visit, four patients received treatment with low-dose steroids alone and one patient received both low-dose steroids and d-penicillamine. Four patients showed elevated IL-33 levels at the first visit, but levels decreased to the normal range thereafter (Fig. 3). Notably, mean IL-33 levels and TSS were significantly decreased during the follow-up (P < 0.01 and P < 0.05, respectively). Consistently, percent change in serum IL-33 levels was positively correlated with that in TSS (P < 0.05, r 2 = 0.36; data not shown). Percent change in serum IL-33 levels did not significantly correlate with that in percent predicted FVC (data not shown).
Discussion
This is the first report of elevated serum IL-33 levels in SSc patients. Serum IL-33 levels were elevated in dSSc, but not in lSSc, patients (Fig. 1). Elevation of IL-33 levels was consistently associated with the greater extent of skin fibrosis and greater frequency and severity of PF (Fig. 2 and Table 1). These results suggest that IL-33 plays a role in cutaneous and pulmonary fibrosis in SSc patients.
In SSc patients, CD4+ T cell infiltration is observed around small vessels in the dermis of early skin lesions [20–22]. Furthermore, the degree of cell infiltration correlates with both the degree and progression of skin thickening [20]. In this study, serum IL-33 levels were associated with the extent of skin sclerosis and severity of PF. IL-33 induces migration of Th2 lymphocytes and enhances Th2 cytokine production [12]. Consistent with this, serum concentrations of Th2 cytokines such as IL-4 and IL-13 in SSc patients are increased, while SSc patients exhibit substantial Th2 cytokine production in cultures of CD4+ T lymphocytes isolated from their affected skin [3, 5]. Furthermore, Th2 cytokines such as IL-4 enhance collagen production by fibroblasts [23, 24]. Thus, IL-33 is likely to contribute to the Th2 lymphocyte infiltration and promote Th2 cytokine production, leading to skin fibrosis in SSc.
It has recently been reported that IL-33 and its receptor ST2 are abnormally expressed in patients with SSc [25]. In lesional skin from patients with early SSc, IL-33 protein is downregulated or absent in endothelial cells and epidermis while IL-33 mRNA is upregulated. Moreover, endothelial cells, perivascular infiltrating mast cells, macrophages, T cells, B cells, and activated fibroblasts/myofibroblasts exhibit strong ST2 expression. By contrast, in lesional skin from patients with late SSc, IL-33 protein is constitutively found in endothelial cells while IL-33 mRNA expression is normal. Furthermore, ST2 expression in the skin of patients with late SSc is weaker than in the skin of those with early SSc. In early skin lesions of patients with SSc, mononuclear cells infiltrate around small vessels in the dermis and promote endothelial cell damage [21, 22]. These results suggest that the damage of endothelial cells in patients with early SSc enhances IL-33 mRNA expression and the release of IL-33 protein into circulation. Consistent with these findings, serum IL-33 levels were elevated in patients with early SSc but significantly decreased during the follow-up (Fig. 3). Thus, serum IL-33 levels are likely to reflect the degree of endothelial damage in patients with early SSc. Further studies are needed to address the role of IL-33 in the pathogenesis of SSc. Nonetheless, measurement of serum IL-33 in patients with early SSc may offer an important means for further evaluation of SSc disease severity because no specific serum marker for SSc has been found to date.
References
White B (1996) Immunopathogenesis of systemic sclerosis. Rheum Dis Clin Nor Am 32:695–708
Sato S (1999) Abnormalities of adhesion molecules and chemokines in scleroderma. Curr Opin Rheumatol 11:503–507
Needleman BW, Wigley FM, Stair RW (1992) Interleukin-1, interleukin-2, interleukin-4, interleukin-6, tumor necrosis factor-α, and interferon-γ levels in sera from patients with scleroderma. Arthritis Rheum 35:67–72
Famularo G, Procopio A, Giacomelli R et al (1990) Soluble interleukin-2 receptor, interleukin-2 and interleukin-4 in sera and supernatants from patients with progressive systemic sclerosis. Clin Exp Immunol 81:368–372
Hasegawa M, Fujimoto M, Kikuchi K, Takehara K (1997) Elevated serum levels of interleukin 4 (IL-4), IL-10, and IL-13 in patients with systemic sclerosis. J Rheumatol 24:328–332
Matsushita T, Hasegawa M, Hamaguchi Y, Takehara K, Sato S (2006) Longitudinal analysis of serum cytokine concentrations in systemic sclerosis: association of interleukin 12 elevation with spontaneous regression of skin sclerosis. J Rheumatol 33:275–284
Molteni M, Della Bella S, Mascagni B et al (1999) Increased interferon-gamma (IFN-γ) levels produced in vitro by alloactivated T lymphocytes in systemic sclerosis and Raynaud's phenomenon. Clin Exp Immunol 116:164–168
Grassegger A, Schuler G, Hessenberger G et al (1998) Interferon-gamma in the treatment of systemic sclerosis: a randomized controlled multicentre trial. Br J Dermatol 139:639–648
Schmitz J, Owyang A, Oldham E et al (2005) IL-33, an interleukin-1-like cytokine that signals via the IL-1 receptor-related protein ST2 and induces T helper type 2-associated cytokines. Immunity 23:479–490
Moussion C, Ortega N, Girard JP (2008) The IL-1-like cytokine IL-33 is constitutively expressed in the nucleus of endothelial cells and epithelial cells in vivo: a novel 'alarmin'? PLoS ONE 3:e3331
O'Neill LA, Dinarello CA (2000) The IL-1 receptor/toll-like receptor superfamily: crucial receptors for inflammation and host defense. Immunol Today 21:206–209
Komai-Koma M, Xu D, Li Y, McKenzie AN, McInnes IB, Liew FY (2007) IL-33 is a chemoattractant for human Th2 cells. Eur J Immunol 37:2779–2786
Xu D, Jiang HR, Kewin P et al (2008) IL-33 exacerbates antigen-induced arthritis by activating mast cells. Proc Natl Acad Sci USA 105:10913–10918
Palmer G, Talabot-Ayer D, Lamacchia C et al (2009) Inhibition of interleukin-33 signaling attenuates the severity of experimental arthritis. Arthritis Rheum 60:738–749
Subcommittee for Scleroderma Criteria of the American Rheumatism Association Diagnostic and Therapeutic Criteria Committee (1980) Preliminary criteria for the classification of systemic sclerosis (scleroderma). Arthritis Rheum 23:581–590
LeRoy EC, Krieg T, Black C et al (1988) Scleroderma (systemic sclerosis): classification, subsets, and pathogenesis. J Rheumatol 15:202–205
Steen VD, Powell DL, Medsger TAJ (1988) Clinical correlations and prognosis based on serum autoantibodies in patients with systemic sclerosis. Arthritis Rheum 31:196–203
Sato S, Ihn H, Kikuchi K, Takehara K (1994) Antihistone antibodies in systemic sclerosis: association with pulmonary fibrosis. Arthritis Rheum 37:391–394
Clements PJ, Lachenbruch PA, Seibold JR et al (1993) Skin thickness score in systemic sclerosis: an assessment of interobeservar variability in 3 independent studies. J Rheumatol 20:1892–1896
Roumm AD, Whiteside TL, Medsger TA Jr, Rodnan GP (1984) Lymphocytes in the skin of patients with progressive systemic sclerosis. Quantification, subtyping, and clinical correlations. Arthritis Rheum 27:645–653
Fleischmajer R, Perlish JS, Reeves JRT (1977) Cellular infiltrates in scleroderma skin. Arthritis Rheum 20:975–984
Scharffetter K, Lankat-Buttgereit B, Krieg T (1988) Localization of collagen mRNA in normal and scleroderma skin by in-situ hybridization. Eur J Clin Invest 18:9–17
Gillery P, Fertin C, Nicolas JF et al (1992) Interleukin-4 stimulates collagen gene expression in human fibroblast monolayer cultures. Potential role fibrosis. FEBS Lett 302:231–234
Chizzolini C (1999) T lymphocyte and fibroblast interactions: the case of skin involvement in systemic sclerosis and other examples. Springer Semin Immunopathol 21:431–450
Manetti M, Ibba-Manneschi L, Liakouli V et al (2010) The IL1-like cytokine IL33 and its receptor ST2 are abnormally expressed in the affected skin and visceral organs of patients with systemic sclerosis. Ann Rheum Dis 69:598–605
Acknowledgements
This work was supported by a grant from the Nakatomi Foundation.
Disclosures
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yanaba, K., Yoshizaki, A., Asano, Y. et al. Serum IL-33 levels are raised in patients with systemic sclerosis: association with extent of skin sclerosis and severity of pulmonary fibrosis. Clin Rheumatol 30, 825–830 (2011). https://doi.org/10.1007/s10067-011-1686-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-011-1686-5