Abstract
Rheumatoid arthritis (RA) is associated with progressive joint destruction, with functional status influenced by both disease activity and radiographic progression. The case for early aggressive treatment of RA is based on large amounts of good data in many countries. Studies with conventional disease-modifying anti-rheumatic drugs in early RA have shown improved outcomes compared with later treatment, especially if an aggressive approach with combinations of drugs is used. Early intervention with tumour necrosis factor (TNF) inhibitors has been shown to improve clinical outcomes, induce remission and prevent radiographic progression. It also improves patients’ functional status, health-related quality of life, and reduces fatigue. Patients with RA have reduced productivity, an increased number of lost work days and retire early; enabling patients to work should be at the core of a therapy’s cost-effectiveness. Introduction of anti-TNF therapy early in RA has been shown to decrease job loss and reduce the amount of working time missed. Although the drug costs of initial treatment with combination therapy including a TNF inhibitor are high, these may be compensated by the reduction in lost productivity, making such a strategy cost-effective overall. In addition, some patients who respond well to combination therapy may be able to stop the TNF inhibitor. It is important to assess the benefits of any intervention not just to healthcare costs but to society as a whole, and physicians should be advocates for optimal access to effective therapies for their patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rheumatoid arthritis (RA) is associated with progressive joint destruction. A longitudinal study in the Netherlands in the late 1980s and 1990s followed a cohort of RA patients over 12 years [1]. It showed a steady deterioration in Sharp score over time, indicating continuous radiological progression despite treatment with disease-modifying anti-rheumatic drugs (DMARDs). The Disease Activity Score (DAS) and Health Assessment Questionnaire (HAQ) score showed a more variable course, but the two scores correlated well over the 12 years [1]. However, the correlation between HAQ and Sharp scores increased with time. Therefore, functional status is influenced primarily by disease activity in the early years, but radiographic progression has an increasing effect on function over time. A cohort of patients treated in the Leiden Early Arthritis Cohort showed an approximately 4-point difference in Sharp score between those treated conventionally during 1993–1995 and those treated with DMARDs within 2 weeks of diagnosis during 1995–1998, which was sustained to at least 4 years [2]. This suggests that a window of opportunity may exist, whereby early diagnosis and aggressive treatment might alter the natural history of RA [3].
With the development of biologic agents, such as tumour necrosis factor (TNF) inhibitors in the past decade, the case for early treatment has become even stronger. In a competitive world, physicians must be advocates for their patients for healthcare resources. An unmet need of rheumatology patients remains, with many patients not receiving the recommended therapy [4], and rheumatology needs to maintain its share of the available resources. The case for early aggressive treatment of RA is built on large amounts of good data in many countries, but it needs to be effectively communicated, for both payer and clinical audiences.
Clinical benefits of early intervention
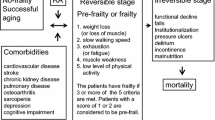
Inflammation is the major factor driving the progression of structural damage in RA [5], with magnetic resonance imaging data showing that synovial thickness predicts bone damage [6]. Disease duration has been shown to be the most important predictor of response to treatment [7, 8]. Function (as measured by HAQ) has a reversible component due to inflammation and an irreversible component reflecting permanent bone damage; the longer the disease duration, the less reversible the functional loss becomes [9]. These factors may lead to a window of opportunity for early treatment of RA, a concept supported by the finding that a single dose of corticosteroid given within 3 months of symptom onset can achieve clinical remission in about half of patients [10].
Indeed, early treatment of RA with DMARDs has been shown to improve long-term clinical outcomes. A meta-analysis of 12 studies of early vs delayed (5–13 months) DMARD therapy found a significant 33% reduction of radiographic progression in patients treated early [11]. Patients with more aggressive disease seemed to benefit most from early DMARD initiation (p = 0.04) [11].The FIN-RACo study showed that early treatment of RA with a combination of DMARDs was more effective than single DMARD therapy, with clinical remission seen in 37% of patients receiving combination DMARDs, compared with 18% in those patients receiving a single DMARD (p = 0.003), and clinical improvement in 71% vs 58% (p = 0.058), respectively, at 2 years [12]. A 5-year extension of this study demonstrated improved long-term radiographic outcomes in patients who had been treated with this early aggressive strategy, with median Larsen scores at 5 years of 11 vs 24 in those patients receiving DMARD monotherapy (p = 0.001), although there was a trend towards an increase in progression in both groups [13].
However, radiographic progression of RA continues in a substantial proportion of patients who achieve low disease activity levels with conventional DMARDs [14]. A number of studies have shown that the early introduction of biologic therapies improves clinical outcomes. The COmbination of Methotrexate and ETanercept in active early rheumatoid arthritis (COMET) trial was the first RA study with remission as a primary endpoint. Methotrexate-naïve patients who had early (3–24 months’ duration) moderate-to-severe RA (DAS28 ≥ 3.2) were randomised to treatment for 1 year with methotrexate alone (n = 268) or methotrexate in combination with etanercept (n = 274) [15]. Clinical remission (defined as DAS28 <2.6) at 1 year was achieved by 50% of patients in the combination therapy group compared with 28% of those on methotrexate alone (p < 0.001). Eighty percent of patients treated with combination therapy, vs 59% of those receiving methotrexate alone, had no radiographic progression (p < 0.001) [15]. In addition, the Early Rheumatoid Arthritis (ERA) study demonstrated that etanercept monotherapy was superior to methotrexate at 2 years in terms of ACR20 response (72% vs 59%; p = 0.005) and radiographic progression (increase in total Sharp score 1.3 vs 3.2; p = 0.001) [16].
Another study—called PREMIER—compared combination therapy with adalimumab plus methotrexate (n = 268) against monotherapy with either adalimumab (n = 274) or methotrexate (n = 257) in methotrexate-naive patients with RA of <1 year’s duration [17]. After 1 year, ACR50 response was significantly better with combination therapy than with either agent alone (62% vs 41% for adalimumab and 46% for methotrexate; p < 0.001), and this response was sustained at 2 years. After 1 year of treatment, clinical remission (defined as DAS28 <2.6) was achieved in 43% of patients receiving combination therapy, compared with 23% of patients receiving adalimumab monotherapy and 21% of those receiving methotrexate monotherapy (both p < 0.001). There was significantly less radiographic progression at 6 months, 1 year and 2 years in patients who received adalimumab plus methotrexate, compared with either monotherapy (Fig. 1). Progression was also significantly lower with adalimumab alone than with methotrexate alone, despite the similarity in clinical responses [17]. Adalimumab in combination with methotrexate resulted in less radiographic progression than methotrexate monotherapy across the spectrum of clinical response [18].
The BeSt study randomised 508 patients with recent-onset RA to four treatment strategies: (1) sequential monotherapy (starting with methotrexate); (2) step-up to combination therapy (starting with methotrexate); (3) initial combination therapy with methotrexate, sulphasalazine, and a tapered high dose of prednisone; and (4) initial combination therapy with methotrexate and infliximab [19]. Initial combination therapy, either with prednisone or with infliximab, resulted in more continuous clinical remission (DAS <1.6) and less joint damage progression than initial monotherapy. After 2 years, 40% of patients in group 1, 34% in group 2, 20% in group 3 and 18% in group 4 had radiographic progression greater than the smallest detectable difference [19].
Effect of early intervention on patient-reported outcomes
The COMET trial also looked at a range of patient-reported outcomes. Patients receiving combination therapy had significantly greater improvements in HAQ than did those receiving methotrexate alone (p < 0.001), and significantly more of them achieved a minimum clinically important difference in HAQ (88% vs 78%, p = 0.006) [20]. Improvement in SF-36 scores was significantly greater in the etanercept plus methotrexate group than the methotrexate monotherapy group in the domains of physical functioning, vitality, bodily pain and role limitation—emotional (Fig. 2). A significantly greater improvement in SF-36 physical component scores was seen with combination therapy; while no difference was seen in mental component scores [20]. The EuroQol health assessment (EQ-5D) utility score (where 0 = death and 1 = perfect health) improved from a baseline of 0.39 in both groups to 0.73 in the combination therapy group, compared with 0.68 in the methotrexate group (p = 0.011).
Change in mean SF-36 scores from baseline to 52 weeks after treatment with etanercept plus methotrexate (ETN+MTX) or MTX alone [20], *p < 0.001; **p = 0.02; † each domain range is from 0 (worst) to 100 (best). Reproduced with permission
Fatigue, which is likely to be an important factor in absenteeism from work, was measured on a visual analogue scale (VAS: from 0 = no fatigue to 100 = worst imaginable fatigue) improved by 48% with combination therapy vs 34% with methotrexate (p < 0.001) [20]. With etanercept plus methotrexate, fatigue improved by 30% in the first 2 weeks, whereas patients on methotrexate took approximately 10 weeks to achieve this improvement [20]. Tools for measuring fatigue have not yet been fully developed, but other studies have shown reductions in fatigue with anti-TNF therapy in RA [21].
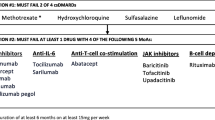
Cost-effectiveness of TNF inhibitors in combination with methotrexate after two DMARD failures [23]
The ERA study showed that significantly more patients treated with etanercept than with methotrexate had an improvement of at least 0.5 units in the HAQ score after 2 years (55% vs 37%; p < 0.001) [16]. A subanalysis of the PREMIER study found that the Physical Component Summary score on the SF-36 quality of life scale had improved after 1 year’s treatment with adalimumab plus methotrexate and was similar to that of the US population, whereas the score for patients treated with methotrexate alone remained significantly below that of the US population [22]. In the BeST study, initial combination therapy resulted in greater improvement in functional ability (HAQ) at 3 and 6 months, compared with initial monotherapy [19]. This improvement was maintained despite infliximab being withdrawn in many patients [19].
Cost-effectiveness of anti-TNF therapy
Cost-effectiveness is calculated as an incremental cost-effectiveness ratio (ICER), or cost per quality-adjusted life-year. Data from the Harvard School of Public Health assigns an ICER of $33,168 for use of etanercept vs methotrexate in RA, which is well below the accepted cost-effectiveness threshold of $50,000. It is also considerably lower than the ICERs of other established interventions, such as screening vs no screening for hypertension ($49,041), coronary artery bypass grafting vs medical management for angina ($64,298), and dialysis vs no dialysis for renal failure ($174,367).
An economic appraisal by the National Institute for Health and Clinical Excellence (NICE) in 2007 found that treatment with etanercept plus methotrexate had similar cost-effectiveness whether it was started in DMARD-naïve patients, in patients who had failed to respond to one conventional DMARD or in those who had failed two DMARDs [23]. All three anti-TNF agents were found to be cost-effective. However, etanercept was more cost-effective than adalimumab, which was in turn more cost-effective than infliximab [23]. NICE also found that anti-TNF therapy in patients who had failed on two DMARDs was considerably more cost-effective in those with early RA (Fig. 3) [23]. However, this finding in favour of early treatment was considered uncertain due to the limited data available.
Total lost work days over 52 weeks with etanercept plus methotrexate (ETN+MTX) or MTX alone [31], optimistic scenario: sum of missed workdays, reduced workdays and stopped workdays; pessimistic scenario: highest value among missed workdays, reduced workdays and stopped workdays, *Probability of [(ETN+MTX) − MTX] > 0 among 10,000 samples generated using Bootstrapping methods
Impact of early intervention on ability to work
Patients with RA have reduced productivity, an increased number of lost work days, and retire early. A systematic review reported that 66% of employed RA patients had experienced work loss (absenteeism or short-term sick leave) in the previous 12 months; the median duration of work loss was 39 days [24]. Approximately a third of RA patients stop work early, which begins soon after onset, with time from diagnosis of RA until a 50% probability of being work disabled varying from 4.5 to 22 years [24]. In a prospective cohort substudy of the FIN-RACo early intervention trial, 75% of patients lost work days in the first 5 years after diagnosis [25]. The mean productivity loss per year (human capital method—see below) was €7,217, and work loss was related to HAQ score and increasing erosions [25]. Rates of work disability in RA increase over time, being approximately 20% in the first year after diagnosis, 32–50% after 10 years, and up to 90% after 30 years [26–28].
The Prevention of Work Disability (PROWD) study randomized methotrexate-naïve patients with both early RA (<2 years) and self-reported work impairment due to RA to treatment with methotrexate alone (n = 73) or in combination with adalimumab (n = 75) for 56 weeks [29]. Over the duration of the trial, job loss or imminent job loss occurred in 19% of patients in the combination therapy group, compared with 40% in the methotrexate group (p = 0.005) [29]. The difference was maintained when patients who withdrew due to ineffective treatment were included (28% vs 52%, p = 0.003). The mean work time lost was 8.6% with combination therapy and 18.4% with methotrexate alone [29].
Improved ability to work may outweigh treatment costs. In an observational work loss and productivity survey of 86 patients who switched to etanercept therapy, missed work days decreased from 1.8 to 0.1 per month, the number of days that RA limited work decreased from 6.5 to 0.2 per month, and the effect of RA on productivity (1–10 scale) improved from 5.8 to 2.1 (all p < 0.001) after the switch to etanercept [30].
The COMET study included 205 patients who were working full- or part-time at baseline. Patients in the methotrexate arm (n = 100) had an average age of 45.1 years, disease duration of 8.9 months, a HAQ score of 1.5, and a DAS28 of 6.4 [31]. Those in the etanercept plus methotrexate arm had an average age of 45.4 years, disease duration of 8.6 months, HAQ 1.6, and DAS28 6.3. This was, therefore, a population of relatively young patients with very early RA, medium functional loss and high disease activity. Among these patients, the number of missed work days over 52 weeks was 14.3 with combination therapy vs 31.9 with methotrexate monotherapy (p = 0.01) [31]. The reduction in working time over 52 weeks was 10.5 days with etanercept plus methotrexate and 19.8 days with methotrexate alone (p = 0.08). The total loss in work productivity was significantly lower with combination therapy; calculated using an optimistic or a pessimistic scenario (Fig. 4) [31].
Outside of clinical trials, data from the Stockholm anti-TNFalpha follow-up registry show significant increases in hours worked per week in RA patients receiving anti-TNF therapy [32]. Patients (n = 594) aged 18–55 years with RA worked a mean of 20 h/week at baseline; this increased by 2.4 h after 6 months, by 4 h at 1 year, and by 6.3 h after 2 years (all p < 0.001 vs baseline), after which it stabilised. The authors calculated that, over 5 years of treatment, the expected indirect cost gain corresponded to 40% of the annual anti-TNF drug cost in patients continuing treatment [32].
The value of a therapy may, therefore, be reflected in a patient being able to work, which may be apparent in a reduction of the number of working days lost due to RA, reduced fatigue or increased productivity. Enabling patients to work should be at the core of any therapy’s cost-effectiveness.
Strategies to decrease costs
One way of potentially reducing the cost of anti-TNF therapy could be to use a “step-back” strategy, in which the TNF inhibitor is stopped in patients who have responded well to initial combination therapy. Preliminary data suggest that approximately 40% of such patients will continue to do well on methotrexate monotherapy [33]. The alternative strategy of trying one drug after another can take many months or even years, during which time the patient is likely to be accumulating joint damage and may risk being unable to work. The step-back strategy is likely to be well received in countries where patients pay substantial contributions towards drug costs; the initial outlay is quite high, but there is a 50:50 chance of being able to substantially reduce the cost after the first year of treatment.
Use of such a strategy may represent an additional argument for early intervention. Withdrawal of therapy from patients with longstanding RA is likely to lead to flare-ups of disease, whereas early establishment of remission in patients with early RA may allow withdrawal of the anti-TNF agent from a combined therapy regimen [34]. This approach is now recognised in some RA treatment recommendations, including those of the French Society for Rheumatology, which recommend reducing, the dose of anti-TNF agent in patients achieving prolonged remission [35].
Attributing value to ability to work
In the BeSt study, described above, many early RA patients in the two initial combination therapy arms were able to step back to monotherapy with sulphasalazine or methotrexate. Cost and utility data were collected over 2 years, and the patient’s age was taken into account [36]. Drug costs were highest with the initial infliximab combination therapy strategy, but sick leave was lowest and hours worked highest in this study arm (Table 1). Depending on the extent to which productivity is valued, infliximab costs could be largely compensated for by savings on productivity [36].
The friction cost method of evaluating the impact of productivity loss allows for the replacement of an absent worker by other workers or by previously unemployed people. Productivity is valued as the loss incurred during the time between a person’s absence from work or termination of employment and the point at which another worker fills that position. This method does not allow for people stopping and restarting work. Conversely, the human capital approach derives from the observation that a person’s earnings over a lifetime reflect an investment by society and employers in that individual through education, on-the-job training and work experience. These investments influence the person’s value to the economy, and thus productivity loss is valued by using market wage rates. For people not working for a wage, wages are valued at what replacement workers would earn for their specific services. In BeSt, use of the friction cost method resulted in similar indirect costs in the four study arms; however, use of the human capital method resulted in the value of sustained productivity in the initial infliximab arm largely compensating for the extra drug costs (Table 1) [36].
Health economic analyses of studies with adalimumab and certolizumab have been submitted for publication and should strengthen the economic argument for early biologic therapy in RA.
Conclusions
Early treatment is essential for optimal outcomes, not just clinically but cost-effectively, and it is important to assess the benefits of any intervention not only to healthcare costs, but also to society as a whole.
Early aggressive DMARD therapy can improve clinical outcomes in RA patients, including reduction of long-term radiographic progression. Early use of anti-TNF therapy has the potential to alter the natural history of RA. The COMET trial demonstrated that with early use of etanercept and methotrexate combination therapy, more patients achieve a better quality of life, over half of patients achieve functional remission, and most patients show no radiographic progression. The BeSt study showed the potential to obtain a durable response to biologic therapy in some patients.
When evaluating the use of TNF inhibitors, it is important to consider more than just direct healthcare costs. Ability to work has important societal and personal implications. The COMET trial also demonstrated that patients treated early with etanercept and methotrexate were more likely to remain employed and miss fewer days from work. BeSt showed a reduction in sick leave and an increase in hours worked among patients treated with initial combination therapy including infliximab, while PROWD showed reduced loss of work in patients treated with adalimumab combination therapy.
Value is an increasingly important aspect of health care, and it is essential that physicians can communicate with payers in language they understand; physicians must be advocates for optimal access to effective therapies for their patients.
References
Drossaers-Bakker KW, de Buck M, van Zeben D, Zwinderman AH, Breedveld FC, Hazes JM (1999) Long-term course and outcome of functional capacity in rheumatoid arthritis: the effect of disease activity and radiologic damage over time. Arthritis Rheum 42:1854–1860
van Aken J, Lard LR, le Cessie S, Hazes JM, Breedveld FC, Huizinga TW (2004) Radiological outcome after 4 years of early vs delayed treatment strategy in patients with recent onset rheumatoid arthritis. Ann Rheum Dis 63:274–279
Cush JJ (2007) Early rheumatoid arthritis—is there a window of opportunity? J Rheumatol Suppl 80:1–7
Benhamou M, Rincheval N, Roy C, Foltz V, Rozenberg S, Sibilia J et al (2009) The gap between practice and guidelines in the choice of first-line disease modifying antirheumatic drug in early rheumatoid arthritis: results from the ESPOIR cohort. J Rheumatol 36:934–942
Emery P, McInnes IB, van Vollenhoven R, Kraan MC (2008) Clinical identification and treatment of a rapidly progressing disease state in patients with rheumatoid arthritis. Rheumatology 47:392–398
Emery P (2002) Magnetic resonance imaging: opportunities for rheumatoid arthritis disease assessment and monitoring long-term treatment outcomes. Arthritis Res 4(Suppl 2):S6–S10
Anderson JJ, Wells G, Verhoeven AC, Felson DT (2000) Factors predicting response to treatment in rheumatoid arthritis: the importance of disease duration. Arthritis Rheum 43:22–29
Möttönen T, Hannonen P, Korpela M, Nissilä M, Kautiainen H, Ilonen J et al (2002) Delay to institution of therapy and induction of remission using single-drug or combination-disease-modifying antirheumatic drug therapy in early rheumatoid arthritis. Arthritis Rheum 46:894–898
Aletaha D, Smolen J, Ward MM (2006) Measuring function in rheumatoid arthritis: identifying reversible and irreversible components. Arthritis Rheum 54:2784–2792
Green M, Marzo-Ortega H, McGonagle D, Wakefield R, Proudman S, Conaghan P, Gooi J, Emery P (1999) Persistence of mild, early inflammatory arthritis: the importance of disease duration, rheumatoid factor, and the shared epitope. Arthritis Rheum 42:2184–2188
Finckh A, Liang MH, van Herckenrode CM, de Pablo P (2006) Long-term impact of early treatment on radiographic progression in rheumatoid arthritis: a meta-analysis. Arthritis Rheum 55:864–872
Mottonen T, Hannonen P, Leirisalo-Repo M, Nissila M, Kautiainen H, Korpela M et al (1999) Comparison of combination therapy with single-drug therapy in early rheumatoid arthritis: a randomized trial. Lancet 353:1568–1573
Korpela M, Laasonen L, Hannonen P, Kautiainen H, Leirisalo-Repo M, Hakala M et al (2004) Retardation of joint damage in patients with early rheumatoid arthritis by initial aggressive treatment with disease-modifying antirheumatic drugs: five-year experience from the FIN-RACo study. Arthritis Rheum 50:2072–2081
Brown AK, Conaghan PG, Karim Z, Quinn MA, Ikeda K, Peterfy CG et al (2008) An explanation for the apparent dissociation between clinical remission and continued structural deterioration in rheumatoid arthritis. Arthritis Rheum 58:2958–2967
Emery P, Breedveld FC, Hall S, Durez P, Chang DJ, Robertson D, Singh A, Pedersen RD, Koenig AS, Freundlich B (2008) Comparison of methotrexate monotherapy with a combination of methotrexate and etanercept in active, early, moderate-to-severe rheumatoid arthritis (COMET): a randomised, double-blind, parallel treatment trial. Lancet 372:375–382
Genovese MC, Bathon JM, Martin RW, Fleischmann RM, Tesser JR, Schiff MH et al (2002) Etanercept vs methotrexate in patients with early rheumatoid arthritis: two-year radiographic and clinical outcomes. Arthritis Rheum 46:1443–1450
Breedveld FC, Weisman MH, Kavanaugh AF, Cohen SB, Pavelka K, van Vollenhoven R et al (2006) The PREMIER study: a multicenter, randomized, double-blind clinical trial of combination therapy with adalimumab plus methotrexate vs methotrexate alone or adalimumab alone in patients with early, aggressive rheumatoid arthritis who had not had previous methotrexate treatment. Arthritis Rheum 54:26–37
Emery P, Genovese MC, van Vollenhoven R, Sharp JT, Patra K, Sasso EH (2009) Less radiographic progression with adalimumab plus methotrexate vs methotrexate monotherapy across the spectrum of clinical response in early rheumatoid arthritis. J Rheumatol 36:1429–1441
Allaart CF, Goekoop-Ruiterman YP, de Vries-Bouwstra JK, Breedveld FC, Dijkmans BA, FARR Study Group (2006) Aiming at low disease activity in rheumatoid arthritis with initial combination therapy or initial monotherapy strategies: the BeSt study. Clin Exp Rheumatol 24(6 Suppl 43):S-77–S-82
Kekow J, Moots RJ, Emery P, Durez P, Koenig A, Singh A et al (2010) Patient-reported outcomes improve with etanercept plus methotrexate in active early rheumatoid arthritis and the improvement is strongly associated with remission: the COMET trial. Ann Rheum Dis 69:222–225
Yount S, Sorensen MV, Cella D, Sengupta N, Grober J, Chartash EK (2007) Adalimumab plus methotrexate or standard therapy is more effective than methotrexate or standard therapies alone in the treatment of fatigue in patients with active, inadequately treated rheumatoid arthritis. Clin Exp Rheumatol 25:838–846
Kimel M, Cifaldi M, Chen N, Revicki D (2008) Adalimumab plus methotrexate improved SF-36 scores and reduced the effect of rheumatoid arthritis (RA) on work activity for patients with early RA. J Rheumatol 35:206–215
National Institute for Health and Clinical Excellence (2007) Adalimumab, etanercept and infliximab for the treatment of rheumatoid arthritis. NICE, London
Burton W, Morrison A, Maclean R, Ruderman E (2006) Systematic review of studies of productivity loss due to rheumatoid arthritis. Occup Med (Lond) 56:18–27
Puolakka K, Kautiainen H, Pekurinen M, Möttönen T, Hannonen P, Korpela M et al (2006) Monetary value of lost productivity over a five year follow up in early rheumatoid arthritis estimated on the basis of official register data on patients’ sickness absence and gross income: experience from the FIN-RACo trial. Ann Rheum Dis 65:899–904
Lacaille D (2005) Arthritis and employment research: where are we? Where do we need to go? J Rheumatol Suppl 72:42–45
Puolakka K, Kautiainen H, Möttönen T, Hannonen P, Korpela M, Hakala M et al (2005) Early suppression of disease activity is essential for maintenance of work capacity in patients with recent-onset rheumatoid arthritis: five-year experience from the FIN-RACo trial. Arthritis Rheum 52:36–41
Eberhardt K, Larsson BM, Nived K, Lindqvist E (2007) Work disability in rheumatoid arthritis—development over 15 years and evaluation of predictive factors over time. J Rheumatol 34:481–487
Bejarano V, Quinn M, Conaghan PG, Reece R, Keenan AM, Walker D et al (2008) Effect of the early use of the anti-tumor necrosis factor adalimumab on the prevention of job loss in patients with early rheumatoid arthritis. Arthritis Rheum 59:1467–1474
Mazonson P, Globe D, Santas C, Murphy R, Cheng A, Huang X et al (2008) Assessing the impact of etanercept treatment on productivity: results from a recent RA patient work loss and productivity survey. Ann Rheum Dis 67(Suppl II):646
Anis A, Zhang W, Emery P, Sun H, Singh A, Freundlich B, Sato R (2009) The effect of etanercept on work productivity in patients with early active rheumatoid arthritis: results from the COMET study. Rheumatology 48:1283–1289
Augustsson J, Neovius M, Cullinane-Carli C, Eksborg S, van Vollenhoven RF (2010) Patients with rheumatoid arthritis treated with tumour necrosis factor antagonists increase their participation in the workforce: potential for significant long-term indirect cost gains (data from a population-based registry). Ann Rheum Dis 69:126–131
Tanaka Y, Takeuchi T, Mimori T, Miyasaka N, Koike T (2009) Discontinuation of infliximab therapy is possible after acquiring remission in patients with rheumatoid arthritis (RA): first report on RRR (remission induction by remicade in RA) study. Ann Rheum Dis 68(Suppl 3):120
Saleem B, Nizam S, Emery P (2006) Can remission be maintained with or without further drug therapy in rheumatoid arthritis? Clin Exp Rheumatol 24(Suppl 43):S-33–S-36
Fautrel B, Pham T, Mouterde G, Le Loët X, Goupille P, Guillemin F et al (2007) Recommendations of the French Society for Rheumatology regarding TNFalpha antagonist therapy in patients with rheumatoid arthritis. Joint Bone Spine 74:627–637
van den Hout WB, Goekoop-Ruiterman YP, Allaart CF, de Vries-Bouwstra JK, Hazes JM, Kerstens PJ et al (2009) Cost-utility analysis of treatment strategies in patients with recent-onset rheumatoid arthritis. Arthritis Rheum 61:291–299
Conflict of interest
The content of this article is the sole responsibility of the author. Medical writing assistance for the preparation of this article was provided by Synergy who received financial support from Pfizer. F. Breedveld has received honoraria from Abbott and Pfizer for speaking and consulting.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Breedveld, F. The value of early intervention in RA—a window of opportunity. Clin Rheumatol 30 (Suppl 1), 33–39 (2011). https://doi.org/10.1007/s10067-010-1638-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-010-1638-5