Abstract
Intra-articular corticosteroid injection (IACI) is a very popular procedure. In this review, we wanted to review all that had been published about local effects of IACIs. English literature search was made through PubMed using the terms intra-articular and local effect. Effects on subjective, functional, structural, cellular, humoral, molecular, and imaging aspects were included. Also, all local adverse effects were documented. The main beneficial effect of IACI is pain relief. The duration of this effect is variable and depends on underlying disease, type of disease, amount of structural damage, type of IACI, dose of IACI, presence of joint effusion, level of inflammatory mediators, emptiness of joint effusion, availability of imaging, and others. At large, inflammatory problems had higher rate of favorable response in terms of pain and function. IACI at the knee joint in juvenile idiopathic arthritis patients resulted in remission for >6 months in >80% of the patients with a mean duration of ∼1.2 years, while in the osteoarthritic knee there was a pain relief for 3 weeks only and in rheumatoid arthritis (RA) knee for 8 weeks. There was no joint space loss at the knee joint following multiple IACI in osteoarthritis and also no increase in cartilage or bone erosions in RA following a single IACI. IACI guide imaging is important in achieving better results in particular joints. Joint infection rate is very low. Other adverse effects included intra-articular and periarticular calcifications, cutaneous atrophy, cutaneous depigmentation, avascular necrosis, rapid destruction of the femoral head, acute synovitis, Charcot’s arthropathy, tendinopathy, Nicolau’s syndrome, and joint dislocation. IACI is associated with a wide range of local effects. Subjective and functional favorable response is prominent mainly in juvenile idiopathic arthritis patients. Adverse effects are either rare or insignificant.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intra-articular corticosteroid injection (IACI) is a very popular procedure [1]. It has been in medical practice for nearly 60 years [2]. It has the advantage of targeting the painful joint, directly resulting, usually, in a swift and remarkable response with less systemic effect. The main indication for IACI is joint pain. The major preparations in terms of popularity are methylprednisolone acetate (MPA), triamcinolone hexacetonide (TAH), triamcinolone acetonide (TA), betamethasone acetate/betamethasone sodium phosphate (Celestone Chronodose) and betamethasone dipropionate/betamethasone sodium phosphate (Diprospan) [3]. These preparations are ester compounds that dissolve slowly in order to achieve a prolonged effect. The duration of response had been found to vary according to the type of IACI, dose, subtype of arthritis, duration of disease prior to injection, and accuracy of injection [3].
The most commonly injected joint is the knee; however, nearly every joint could be injectable including the facet joints where guiding imaging could be very helpful.
In this study, we want to review all what had been published in the English literature about local effects of IACI in humans.
Patients and methods
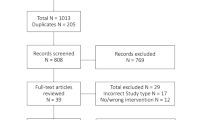
Literature search was done through PubMed, using the terms intra-articular and corticosteroids up to and including the year 2008. Reports were also located using references of related articles. Only reports related to humans in the English literature were included. Articles where IACI were given periarticularly were not included. The local effects of IACI were divided into two major categories, one category of adverse effects and the other of favorable and other effects. The effects of the second category included subjective, functional, structural, cellular, humoral, molecular, imaging, and other parameters. At large, the basic problems of the injected joints were divided into either inflammatory or degenerative/mechanical.
Results
Degenerative/mechanical
Osteoarthritis—knee
This is the most investigated topic. In a meta-analysis study, it had been shown that IACI is associated with symptomatic relief for only 3 weeks (Table 1). For patients’ global and function, there was a lack of effect beyond 1 week [4]. Compared to hyaluronic acid (HA) injection, no difference up to 4 weeks but between 4 and 13 weeks, HA was superior to IACI at least in one variable, WOMAC osteoarthritis (OA) index, pain, range of motion (ROM; flexion), and number of responders or Lequesne’s index. Compared to joint lavage, there was no difference. In some studies, joint lavage was superior to IACI where IACI had improvement of pain and Lequesne’s functional index at weeks 1 and 4 only, while joint lavage had significant pain improvement at weeks 1, 4, 12, and 24 without effect on Lequesne’s functional index [5]. Comparing arthroscopic lavage (AL) versus AL plus IACI or regular lavage vs regular lavage plus IACI, there was no significant difference between the groups [6].
Predictors of improvement in some studies were joint effusion, successful aspiration of the joint fluid prior to injection, and less severe radiographic changes [7]. In other studies, no predictors of response were found [8]. In patients with knee OA and Baker cyst, 40 mg of TA accounted for reduction in the dimensions of the cyst as well as cyst wall thickness and improvement of ROM as a result of that [9]. In evaluating structural changes, multiple injections of 40 mg of TA at the knee joint every 3 months and up to 2 years compared to normal saline showed no difference between the two groups with respect to loss of joint space over time [10]. Synovial inflammation assessed by gadolinium-enhanced magnetic resonance imaging (MRI) decreased within the first week following the injection and remained low during remission [11].
MPA significantly reduced the number of mast cells in primary OA and tended to decrease the number of hypertrophic and increase the number of fibroblast-lining cells. There was a decrease in the number of macrophages, lymphocytes, and adipocytes and an increase in number of fibroblasts and the amount of collagen [12]. MPA resulted in a significant decrease in CD68+ staining in the synovial lining layer, but no change in the CD68 expression in the synovial sublining layer. There was no significant difference in the MCP-1, MIP-1 alpha, matrix metalloproteinase (MMP)-1, MMP-3, tissue inhibitor of metalloproteinase (TIMP)-1, and TIMP-2 immunostaining in the synovial lining or sublining layers [13].
Adhesive capsulitis and frozen shoulder
In comparing different preparations of ultrasound (U/S)-guided IACIs with or without physical therapy (PT) to placebo/saline injection at the glenohumeral joint with or without PT, there was a significantly greater improvement in shoulder pain and disability index in the IACI group compared to injection alone lasting for 6–12 weeks. Beyond this period, no significant difference was seen. PT usually improves the ROM, especially external rotation [14]. U/S-guided IACIs were associated with better visual analog scale (VAS) for pain and shoulder function assessment scale at 6 weeks compared to blinded injections [15].
Serial IACI is also a common practice for these problems. There was a beneficial effect with up to three IACI with limited evidence that four to six injections were beneficial [16]. Multiple injections were beneficial until week 16 from the date of the first injection.
OA—carpometacarpal joint
In prospectively evaluating the effect of IACI of 5 mg of TH vs saline injection in 41 patients with first carpometacarpal (CMC) joint OA, there was no difference in pain score using VAS, joint stiffness, joint tenderness, and patient’s or physician’s global assessment. Nonparametric analysis of each group individually revealed significant improvement in patient’s and physician’s global assessment at 4, 12, and 24 weeks in the placebo group and at 4 and 12 weeks in IACI group [17]. In comparing MPA and HA in degenerative trapeziometacarpal joint, there was a relief of pain after 1 month in both groups. Grip strength improved in MPA at 1, 3, and 6 months, while in HA group, grip improved after 6 months and the pinch and function using Purdue Pegboard test after 3 months [18]. Case series evaluating 25 patients with OA of CMC receiving 0.25 ml of MPA and evaluating pain score using VAS showed significant improvement at 1 month but not after 3, 6, and 12 months. Five patients were free of pain for 12 months.
OA—hip
In a prospective cohort study evaluating 120 patients referred for IACI at the hip joint, two groups were created; one injected with 40 mg of MPA and the other with 80 mg of MPA. The first group had significant improvement in pain and stiffness but not disability at 6 weeks, and the improvement at 12 weeks was maintained, while the second group had significant improvement of pain, stiffness, and disability at 6 and 12 weeks [19].
Degenerative—acromioclavicular joint
Following IACI in 20 patients with primary acromioclavicular joint (ACJ) arthritis, constant score continued to improve significantly after 6 and 12 months. The benefit is felt up to 5 years [20]. The short-term effects of IACI (evaluated prior and 2 weeks later) under image intensifier guidance in 18 patients with isolated ACJ arthropathy revealed significant improvement in pain score and range of extension. In patients with radiographic evidence of degenerative ACJ changes, there was also significant improvement in the range of horizontal flexion [21].
Degenerative—temporomandibular joint
The effects of IACI or HA injection in OA of the temporomandibular joint (TMJ; 20 patients each group) at days 1 and 15, were evaluated at day 14, 1 and 6 months following the injection. Both groups had less pain lasting for 6 months more at the HA group. A decrease in crepitations was observed in both groups. The HA group had improvement of mandibular vertical opening and protrusion. Lateral movement from the affected side improved in both subjects [22].
Degenerative—facet joint
Out of 57 patients with facet joint infiltration for lumbar back pain, 51 were available for follow-up. Fifty-three percent had complete or partial relief after 8 weeks, and 68% had complete or partial relief after 6 months. No predictors of response were found [23]. Excellent pain relief was achieved in 75% of patients after image-guided IACI in the treatment of lumbar facet joint synovial cysts. The cyst resolved completely or partially in 89%.
Inflammatory
Rheumatoid arthritis—knee
IACI following joint aspiration, showed improvement in pain, morning stiffness of the knee, circumference of the knee, walking distance and ROM after 1 and 3 months. Rest is not essential for IACI to be beneficial [24]. In a study on 300 rheumatoid arthritis (RA) patients injected with TA or TAH, 18% of the patients with TAH were pain free at 12 weeks compared to 9% with TA, and after 12 weeks 59% continued improvement with TAH compared to 44% with TA [25]. IACI improved extensor muscle strength at days 7 and 14. ROM also improved. Synovial fluid (SF) withdrawal alone improved extensor muscle torque. In evaluating joint effusion or swelling in 31 RA patients following IACI of 20 mg of TAH, there was a significant decrease in joint effusion and swelling evaluated manually or by inspection within the first week. This significant positive effect was observed also at weeks 6, 12, 26, and 52 [26]. Following IACI of 40 mg of TA at the knee joint in 43 RA patients after maximal joint aspiration, 39 patients (91%) were effusion free 2 weeks later. Following IACI of 80 mg of MPA to the knee joint in 18 RA patients (after maximal aspiration) and followed by serial MRI studies on days 1, 7, 30, 180, and at relapse, there was a mean duration of clinical remission (neither joint swelling or tenderness) of the joint for 8 weeks [27]. Synovial membrane volume had decreased significantly on day 1 with further decrease to 45% and 67% in both joint membrane volume and joint effusion volume, respectively. At relapse, the joint membrane volume increases to preinjection level while the joint effusion remained significantly less than pretreatment levels. Over time, there was no change in the MRI score of cartilage and bone erosions at any knee. There was a statistically significant inverse correlation between synovial membrane volume and duration of clinical remission of the joint. No correlation was found between duration of remission and pretreatment joint effusion, radiographic or MRI score of erosions, erythrocyte sedimentation rate (ESR), CRP, or duration of knee symptoms. In other studies, it was found that aspiration of SF can reduce the risk for relapse and SF C4; percent of SF polymorphonuclear (PMN) cells, blood hemoglobin, and serum C3 correlated significantly with the decrease in knee joint circumference after 2 months [28]. The clinical effect also positively correlated with pretreatment sublining macrophage number and vascular cell adhesion molecule 1 expression. Frequent IACIs in RA patients (four or >IACIs in an asymmetric pattern in a single year) was not associated with increased risk for arthroplasty. It may offer some chondroprotection [29].
Pannus width 1 week following IACI decreased by 20% and 68% in two of six RA patients [30]. Power Doppler sonography with an intravenous ultrasound contrast agent, before and 3 weeks after IACI of 40 mg of TAH, in 18 RA patients after joint aspiration, showed statistically significant reduction of synovial perfusion [31]. Positron emission tomography performed prior and following IACI in RA patients showed 50% reduction in the uptake in the treated knees. Correlation was found also between clinical and histological measures with 99mTc-IgG uptake in RA patients.
IACI resulted in a fall in synovial fluid leukocyte count, mainly in PMN cell count and less in mononuclear cell count with the development of relative lymphocytosis later. It also resulted in a decrease in the number of mast cells (67–96%) and lymphocytes where the number of macrophages remained the same when the synovium was rebiopsied 1–2 weeks later [32]. Neutrophil migration was reduced in nearly all RA patients with a significant correlation with pain score. There was also an increase in albumin concentration and a rise in viscosity and mucin content.
Overall synovial protein expression of tumor necrosis factor (TNF), interleukin (IL)-1 beta, extranuclear high mobility group box protein (HMGB)-1, vascular endothelial growth factor (VEGF), and ICAM-1 was reduced but without significant effect on vascularity. In contrast, expression of IL-1 alpha, VEGF, and cytoplasm HMGB-1 protein in vascular endothelial cells was not affected. It downregulated levels of messenger RNA encoding IL-1 alpha and IL-1 beta but not TNF or HMGB-1 [33]. S100A12 synovial expression was reduced 2 weeks after IACI. Although abundant in presteroid samples of synovial membrane, collagenase and TIMP mRNA were nearly undetectable in tissues 1–2 weeks following IACI. Human leukocyte antigen (HLA)-DR mRNA and C2 and C3 hybridization levels also were significantly decreased.
RA—wrist
Twelve RA patients with active wrist inflammation and treated with DMARDS received U/S-guided IACI of 40 mg of MPA and were evaluated by Doppler U/S and contrast-enhanced MRI prior and following the IACI. There was a significant improvement in swollen target joint score, tender target joint score, and physician’s VAS after 4 weeks. There was no change in MRI or U/S findings; however, MRI erosion score increased [34]. There is no need for elastic wrist orthosis as a postinjection requirement.
RA—TMJ joint
In evaluating the short-term effects (4 weeks) of three different injections, saline, steroids, or HA, among three groups of RA-TMJ arthritis (41 patients total), the HA and steroid groups had significant subjective effects. Maximal voluntary mouth opening significantly increased, and number of tender muscle regions significantly decreased in both groups [35]. TNF in SF of TMJ of patients predicted a treatment effect of IAC on TMJ movement pain. SF 5-hydroxytryptamine (5-HT) was negatively and plasma 5-HT positively correlated with change in TMJ pain after treatment [36].
In evaluating long-term effect of HA or betamethasone injections on TMJ arthritis at 1 or 2 years of follow-up assessing subjective symptoms, clinical signs, and bite force, there was a significant improvement in all parameters in both groups. Even after 8 years of follow-up, the subjective as well the clinical signs were still significantly reduced. Erosions that were before injection remineralized at the follow-up [37].
Juvenile idiopathic arthritis—knee
IACI at the knee joint in pauciarticular juvenile idiopathic arthritis (JIA) resulted in full remission, lasting >6 months, in ∼82% of the patients [38]. The mean duration of remission was 13.9 months. Beneficial effect usually starts within 1 day–2 weeks following the injection. The probability of staying in remission was much higher with TA than with MPA. Discontinuation of all the medications was achieved in 74.4% and correction of joint contraction in 14%. In all the patients with Baker’s cyst and tenosynovitis, there was a complete remission. So IACI may be the only therapy needed in patients with pauciarticular JIA, obviating the need for prolonged oral medications [38, 39]. IACI in the lower extremity has positive effect regarding pain, walking velocity, and joint movement. It also influences the gait pattern of joints that had not been injected [40]. The beneficial effect did not correlate with sex, age of onset, ESR at onset, presence of antinuclear antibody (ANA), HLA, or presence of uveitis [41]. However, sustained clinical response correlated with higher ESR and earlier treatment. Patients with high SF PMN% and ANA positivity tended to have shorter remissions [42]. There is some evidence to the support of knee rest following IACI in JIA patients. MRI showed long-lasting suppression of inflammation and pannus without evidence of toxic effects on cartilage. Statural growth was not affected [43].
S100A12 level in JIA decreased after IACI. MMP-3 and possibly IL-6 and IL-10 are candidate for the development of a set of biomarkers to predict response to IACI among children with chronic arthritis. Carriers of a macrophage migration inhibitory factor 173 C allele were four times more likely to relapse within 3 months.
JIA—TMJ
IACI is the most promising modality of treatment of TMJ inflammation in JIA, and it could potentially prevent mandibular growth alteration [44]. In one study, 23 patients had computed tomography (CT)-guided IACI with triamcinolone preparations. Of 23 patients, 14 had follow-up by MRI. Seventy-seven percent had complete resolution of pain, and 43% had increase in maximal incisal opening. Patients under 6 years of age showed the best results. MRI showed resolution of effusion in 48%.
JIA—subtalar joint
Fluoroscopically guided IACI at the subtalar joint in JIA patients resulted in 89% favorable response rate with mean duration of 1.2 ± 0.9 years [45].
Sacroiliac joint in spondyloarthropathy (SPA)
More than 90% of the patients with inflammatory sacroiliitis who had CT-guided IACI, had a significant abatement of subjective complains for 10 ± 5 months. The percentage contrast enhancement at dynamic MRI showed a significant reduction [46]. In a double-blind study of ten SPA patients with sacroiliitis (13 joints), six were injected with steroids and seven with placebo. Five of six patients injected with steroids had >70% relief of pain after 1 month while none from the placebo group. Results were still significant at 3 months (62%) and at 6 months (58%). In evaluating 30 patients with SPA (54 joints) who had CT-guided IACI using 40 mg of TA by pain and MRI scores prior and following the injection, there was a significant improvement of the back pain at 5.2 ± 1.3 months in 83.3% of the patients. Subjective improvement lasted for 8.9 ± 5.3 months.
Twenty out of 31 patients and nine out of 15 patients after the first and second MRI-guided IACI at the sacroiliac joint reported subjective improvement which lasted for a mean of 8.7 ± 10.9 and 16.1 ± 15.8 months, respectively. Subchondral bone marrow edema resolved in 15 of 20 patients who reported subjective improvement after the first injection.
Miscellaneous
There was a nonsignificant reduction of pain at the shoulder 3 weeks following three serial injections of 40 mg of TA compared to placebo in a multicenter, placebo-controlled study of 37 patients with stroke [46]. IACI of ten adult hemophiliacs (19 joints) resulted in a subjective improvement at 24 h in 79% of the patients that persisted up to 8 weeks in 59%. The number of episodes of hemarthroses decreased from 7.7 bleeds in the 8-week period before injection to 1.9 bleeds in the 8 weeks following the injection. Improvement correlated with the presence of synovitis but not with radiologic changes [47].
Adverse effects
Infections
The perceived risk of joint infection following IACI is considered very low with a rate of ∼1:1,000 to ∼1:25,000 [48]. The risk is higher among immune-compromised and incapacitated patients (Table 2) [49]. However, under simple rules of antiseptic measures, the procedure is considered very safe. Even in patients who had surgery of the hip or knee following previous IACI, there was no significant increase in joint infection compared to those who did not have it. The knee is the most common infected joint, and this stems from being the most injected joint. However, relative to the frequency of injection, the hip is the most infectable joint. Other joints that developed infection following IACI include glenohumeral and facet joints. The time interval for developing clinical signs ranged from 6 days to a few weeks. A wide range of organisms had been identified as causes of infection including gram-positive and gram-negative aerobic bacteria (Staphylococcus, Streptococcus alpha, Pseudomonas, Escherichia coli), anaerobic bacteria (Bacteroides, Clostridium, Propionibacter), fungal (Candida species, Aspergillus fumigatus), and mycobacterium (Mycobacterium abscessus and Mycobacterium avium). However, according to the reported number of fatalities, the prognosis of joint infection following IACI does not seem to be worse than the other group.
There were few fatalities, including one case with hip infection due to Staphylococcus aureus and another case of shoulder infection with gas gangrene and cultures positive for both E. coli and Clostridium [50, 51]. There was also a case of endocarditis, complicating facet joint injection [52].
Calcifications
The most common local adverse effect of IACI, where nearly one of two-four joints following IACI will end with calcifications [53]. These calcifications are mostly pericapsular or intracapsular and rarely intra-articular. They were noted 2 months to 1 year or more following the IACI, with the knee being the most common joint. The location of the calcification is related to the site of the needle injection and varies in size, shape, and structure, being fine at the beginning but tends to coalesce and become coarse with time. Usually, these calcifications are asymptomatic but may become symptomatic if it interferes with the normal mechanics of the joint. Microscopically, there is inflammation, necrosis, and calcifications. These calcifications are composed of hydroxyapatite.
Skin atrophy (linear or nonlinear)
This is one of the most common local adverse effects (around 8%). It is more common in JIA patients. It usually develops 1–4 months following the injection. The atrophy seems to be due to leakage of the injected steroids into the skin. This adverse effect is most likely to happen with small joint injection where accuracy of injection is not guaranteed, the subcutaneous tissue is thinner than around larger joints, and also usually a relatively larger volume and dose of steroids are injected “in” these small joints [54]. This atrophy could be accompanied with hypopigmentation or, rarely, hyperpigmentation.
Depigmentation
Hypopigmentation usually develops after the second injection and may develop simultaneously in more than one injected joint [55]. It usually develops 2 months after the injection but could develop as early as 48 h following the injection. It occurs more in dark-skinned people. The diameter of the hypopigmentation could reach 40 mm. It usually normalizes within 2 months, but in other cases, it may take many months or even stay without any change at all. Linear hypopigmentation could result from lymphogenous spread. Hyperpigmentation could also occur but is very rare [54].
Charcot’s arthropathy
Characterized by rapid resorption and regeneration or fragmentation of the joint that usually follows repeated IACIs (in some cases, nearly 20 injections given twice weekly) [56]. The important criteria needed here is pain-free period/s following the injection that allows excessive unguarded activity in these joints, resulting in destructive changes. Most joints that were reported include knees, hips, and shoulders.
Acute synovitis
This is a rare phenomenon that usually develops after a few to 24 h following IACI, usually of short-acting preparations, reported first by Hollander. Aspiration of the joint effusion usually reveals increased white cell count, mainly PMNs with numerous rod-shaped negatively birefringent intracellular and extracellular steroid crystals [57]. NSAIDS are usually helpful.
Avascular necrosis
Most common joints involved are the hips (proximal femur; 66), knees (distal femur or proximal tibial plateau), and shoulders (proximal humerus). At the knee or shoulders, it usually develops following multiple steroid injections within a short period of time (days or months) with or without continuous oral steroid intake for different periods. The calculated total doses were 160 mg of prednisone, equivalent and higher, with a latent period of few months and in some cases even after 1 week.
Rapid destruction of the femoral head
This term is used to describe a situation of joint destruction and disappearance of joint space following just one IACI [58]. It is usually seen in women with unilateral hip involvement 3–12 months following the injection. Microscopically, there is total necrosis of the underlying trabecular bone and marrow tissue underneath the cartilage.
Nicolau’s syndrome
This is characterized by a sudden sharp pain and pallor at the site of the injection, then erythematous, developing into a purple livedo-like rash after few hours, progressing over a few days towards skin necrosis [59]. Deeper tissues like muscle could be involved. This phenomenon is not peculiar to corticosteroid only but could happen following different intramuscular preparations. The exact mechanism is not clear, but an eventual arterial insult seems to be behind this phenomenon.
Tendinopathy
It includes tendonitis or rupture. Most of the rupture cases affect the Achilles tendon (50%), followed by the patellar (19%) and biceps tendons (8%) [60]. In nearly a quarter of the cases, the rupture occurs after a single IACI and usually develops in less than 2 months.
Joint dislocation
This is reported in one case following IACI at the metatarsophalangeal joint [61].
Discussion
The main beneficial effect of IACI is pain relief. The duration of this effect is variable and depends on different parameters, including type of joint, underlying disease, time interval to treatment, amount of structural damage, type of IACI, dose of IACI, presence of joint effusion, level of inflammatory mediators, emptiness of joint effusion prior to injection, and availability of imaging guidance. In terms of function, favorable results are obtained in some joints with usually less duration. In general, inflammatory joint diseases are associated with higher rate of favorable response and longer duration compared to mechanical/degenerative joint diseases.
Unfortunately, the mean duration of pain relief following IACI at the osteoarthritic knee, the most common arthritic problem, is just 3 weeks with nearly no impact on function. In such cases, it is most recommended to exploit all the measures for higher successful rate like evacuating knee fluid as much as possible in case it exists.
Among the other degenerative/mechanical problems, ACJ, TMJ, and facet joint problems had the highest rate of pain relief duration following IACI, and IACI at these sites are recommended under imaging guidance. IACI will not probably be helpful for hip joint with advanced changes.
The shoulder joint is unique in the sense that serial injections are recommended to achieve better results in adhesive capsulitis followed by PT.
The most plausible results following IACI are among pauciarticular JIA patients. Total remission could be achieved in >80% of the patients, for >6 months with a mean duration of nearly 15 months in patients with involvement of the knee. Discontinuation of medication was achieved in more than 70% of the patients with correction of contractures in some of them. Unlike adult patients with OA or RA, in JIA patients, there is some evidence to support knee rest following IACI. IACI also is the most promising modality of treatment in TMJ involvement in JIA patients, especially those less than 6 years old.
Sacroiliitis due to different spondyloarthropathies is associated with a significant improvement for more than 6 months in 58 to >90 of the patients. CT guidance is very important here to achieve accurate localization.
The rheumatoid knee is probably the second-most injected type of joint after the osteoarthritic knee. The clinical results are better than in OA but less than JIA. Following IACI at the knee joint in RA patients, there was an immediate effect demonstrated by a decrease in synovial membrane volume within the first day. There is usually a significant decrease in joint effusion within the first week that can last for even 1 year. Mean duration of remission at the RA knee joint is about 8 weeks, and aspiration of the joint fluid can reduce relapse. Percentage of synovial PMN leukocyte number correlated significantly with favorable response after 2 and 6 months. It is interesting to note the dramatic regression in pannus size was 1 week following IACI in some patients.
There is no joint space loss in OA of the knee following multiple IACIs every 3 months and up to 2 years. Also, in RA, there was no increase in the score of bone erosions following a single IACI.
In both RA and OA of the knee, there was a reduction in the number of mast cells and lymphocytes at the synovium on rebiopsy.
Joint infection is the most serious adverse effect of IACI. Fortunately, the risk is very low under simple antiseptic measures. Special care should be given when injecting the hip and injecting incapacitated patients or those who are immune-compromised. The prognosis of joint infection following IACI does not seem to be worse than those not following IACI.
The most common adverse effects are not considered serious ones, like local calcifications, skin atrophy, and hypopigmentation. Special care needs to be given for accurate localization and avoidance of spillage of the steroids during penetration and withdrawal of the needle.
Other less common, but more serious, adverse effects could also be manipulated with precautionary measures like less repetitive injection to prevent Charcot’s arthropathy, avoidance of short-acting preparations to decrease the risk of acute synovitis, and lastly to reconsider IACI in women with one-sided OA of the hip to avoid rapid destruction of the femoral head.
References
Snibbe JC, Gambardella RA (2005) Use for injections in osteoarthritis in joints and sports activity. Clin Sports Med 24:83–91
Hollander JL, Brown EM, Jessar RA, Brown CY (1951) Hydrocortisone and cortisone injected into arthritis joints: comparative effects and use of hydrocortisone as a local antiarthritic agent. JAMA 147:16329–16335
Dent PB, Walker N (1998) Intra-articular corticosteroids in the treatment of juvenile rheumatoid arthritis. Curr Opin Rheumatol 10:475–480
Bellamy N, Campbell J, Robinson V, Gee T, Bourne R, Wells G (2005) Intraarticular corticosteroid for treatment of osteoarthritis of the knee. Cochrane Database Syst Rev 2:CD005328
Ravaud P, Moulinier P, Giraudeau B, Ayral X, Guerin C, Noel E, Thomas P et al (1999) Effects of joint lavage and injection in patients with osteoarthritis of the knee. Arth & Rheum 42:475–482
Smith MD, Wetherall M, Darby T, Esterman A, Slavotinek J, Roberts-Thomson P et al (2003) A randomized placebo-controlled trial of arthroscopic lavage versus lavage plus intra-articular corticosteroids in the management of symptomatic osteoarthritis of the knee. Rhematology (Oxford) 42:1477–1485
Gaffney K, Ledingham J, Perry JG (1995) Intra-articular triamcinolone hexacetonide in knee osteoarthritis: factors influencing the clinical response. Ann Rheum Dis 54:379–381
Jones A, Doherty M (1996) Intra-articular corticosteroids are effective in osteoarthritis but there are no clinical predictors of response. Ann Rheum Dis 55:829–832
Acebes JC, Sanchez-Pernaute O, Diaz-Oca A, Herrero-Beaumont G (2006) Ultrasonographic assessment of Baker’s cysts after intra-articular corticosteroid injection in knee osteoarthritis. J Clin Ultrasound 34:113–117
Raynauld JP, Buckland-Wright C, Ward R, Choquette D, Haraoui P, Martel-Pelletier J et al (2003) Safety and efficacy of long-term intra-articular steroid injections in osteoarthritis of the knee. Arthritis & Rheum 48:370–377
Ostergaard M, Stoltenberg M, Henrilsen O, Lorenzen I (1996) Quantitative assessment of synovial inflammation by dynamic gadolinium-enhanced magnetic resonance imaging. A study of the effect of intra-articular methylprednisolone on the rate of early synovial enhancement. Br J Rheumatol 35:50–59
Ronchetti P, Guerra D, Taparelli F, Boraldi F, Bergamini G, Mori G et al (2001) Morphological analysis of knee synovial membrane biopsies from a randomized controlled clinical study comparing the effects of sodium hyaluronate (hyalgen) and methylprednisolone acetate (Depomedrol) in osteoarthritis. Rheumatology (Oxford) 40:158–169
Young L, Katrib A, Cuello C, Vollmer-Conna U, Bertouch JV, Roberts-Thompson PJ (2001) Effects of intraarticular glucocorticoids on macrophage infiltration and mediators of joint damage in osteoarthritis synovial membranes: findings in a double-blind, placebo-controlled study. Arthritis Rheum 44:343–350
Carette S, Moffet H, Tardif J, Bessette L, Morin F, Fremont P et al (2003) Intraarticular corticosteroids, supervised physiotherapy, or a combination of the two in the treatment of adhesive capsulitis of the shoulder. Arthritis Rheum 48:829–838
Naredo E, Cabero F, Beneyto P, Cruz A, Mondejar B, Uson J et al (2004) A randomized comparative study of short term response to blind injection versus sonographic-guided injection of local corticosteroids in patients with painful shoulders. J Rheumatol 31:308–314
Shah N, Lewis M (2007) Shoulder adhesive capsulitis. Systemic review of randomized trials using multiple corticosteroid injections. Br J Gen Pract 57:662–667
Meenagh JK, Patton J, Kynesight GD (2004) A randomized controlled trial of intra-articular corticosteroid injection of the carpometacarpal joint of the thumb in osteoarthritis. Ann Rheum Dis 63:1260–30
Stahl S, Karsh-Zafrir I, Ratzon N, Rosenberg N (2005) Comparison of intraarticular injection of depot corticosteroid and hyaluronic acid for treatment of degenerative trapeziometacarpal joints. J Clin Rheumatol 11:299–302
Robinson P, Keenan AM, Conaghan PG (2007) Clinical effectiveness and dose response of image-guided intra-articular corticosteroid injection for hip osteoarthritis. Rheumatology (Oxford) 46:285–291
Hussain S, Jacobs LG, Hashmi R (2008) The long-term effectiveness of steroid injections in primary acromioclavicular joint arthritis: a five-year prospective study. J Shoulder Elbow Surg 17:535–538
Kurta I, Datir S, Dove M, Rahamatalla A, Wynn-Jones C, Maffulli N (2005) The short term effects of a single corticosteroid injection on the range of motion of the shoulder in patients with isolated acromioclavicular joint arthropathy. Acta Orthop Belg 71:656–661
Bjornland T, Gjaerum AA, Moystad A (2007) Osteoarthritis of the temporomandibular joint: an evaluation of the effects and complications of corticosteroid injection compared with injection with sodium hyaluronate. J Oral Rehabil 34:583–589
Anand S, Butt MS (2007) Patients’ response to facet joint injection. Acta Orthop Belg 73:230–233
Chatham W, Williams G, Moreland L, Parker JW, Ross C, Alcrcon SG et al (1989) Intraarticular corticosteroid injections: should we rest the joints? Arthritis Care Res 2:70–74
Blyth T, Hunter JA, Stirling A (1994) Pain relief in the rheumatoid knee after steroid injection. A single-blind comparison of hydrocortisone succinate, and triamcinolone acetonide or hexacetonide. Br J Rheumatol 33:461–463
Meninger R, Reinhardt S, Sondgen W (1994) Intra-articular treatment of rheumatoid knee-joint effusion with triamcinolone hexacetonide versus sodium morrhuate. Scand J Rheumatol 23:249–254
Ostergaard M, Stoltenberg M, Gideon P, Sorensen K, Henriksen O, Lorenzen I (1996) Changes in synovial membrane and joint effusion volumes after intra-articular methylprednisolone. Quantitative assessment of inflammatory and destructive changes in arthritis by MRI. J Rheumatol 23:1151–1161
Luukkainen R, Hakala M, Sajanti E, Huhtala H, Yli-Kerttula U, Hameenkorpi R (1992) Predictive value of synovial fluid analysis in estimating the efficacy of intra-articular corticosteroid injections in patients with rheumatoid arthritis. Ann Rheum Dis 51:874–876
Roberts WN, Babcock EA, Reitbach SA, Owen DS, Irby WR (1996) Corticosteroid injection in rheumatoid arthritis does not increase rate of total joint arthroplasty. J Rheumatol 23:1001–1004
Leitch R, Walker SE, Hillard AE (1996) The rheumatoid knee before and after arthrocentesis and prednisolone injection: evaluation by Gd-enhanced MRI. Clin Rheumatol 15:358–366
Sallafi F, Carotti M, Manganelli P, Filippucci E, Giuseppetti GM, Grassi W (2004) Contrast-enhanced power Doppler sonography of knee synovitis in rheumatoid arthritis: assessment of therapeutic response. Clin Rheumatol 23:285–290
Malone DG, Wilder RL, Saavedra-Delgado AM, Metcalfe DD (1987) Mast cell numbers in rheumatoid synovial tissues. Correlations with quantitative measures of lymphocytic infiltration and modulation by anti-inflammatory therapy. Arthritis Rheum 30:130–137
Af Klint E, Grundman C, Engstrom M, Cartrina AI, Makrygiannakis D, Klareskog L et al (2005) Intra-articular glucocorticoid treatment reduces inflammation in synovial cell infiltrations more efficiently than in synovial blood vessels. Arthritis Rheum 52:3880–3889
Boesen M, Boesen L, Jensen KE, Cimmino MA, Torp-Pedersen S, Terslev L et al (2008) Clinical outcome and imaging changes after intraarticular (IA) application of etanercept of methylprednisolone in rheumatoid arthritis. Magnetic resonance imaging and ultrasound-Doppler show no effect of IA injections in the wrist after 4 weeks. J Rheumatol 35:584–591
Kopps S, Akerman S, Nilner M (1991) Short-term effects of intra-articular sodium hyaluronate, glucocorticoid, and saline injections on rheumatoid arthritis of the temporomandibular joint. J Craniomandib Disord 5:231–238
Fredriksson L, Alstergren P, Kopp S (2006) Tumor necrosis factor-alpha in temporomandibular joint synovial fluid predicts treatment effect on pain by intra-articular glucocorticoid treatment. Mediators Inflamm 2006:59425
Wenneberg B, Kopp S, Grondahl HG (1991) Long-term effect of intra-articular injections of a glucocorticoid into the TMJ: a clinical and radiographic 8-year follow-up. J Craniomandib Disord 5:11–18
Padeh S, Passwell JH (1998) Intraarticular corticosteroid injection in the management of children with chronic arthritis. Arthritis Rheum 41:1210–1214
Beukelman T, Guevara JP, Albert DA (2008) Optimal treatment of knee monoarthritis in juvenile idiopathic arthritis: a decision analysis. Arthritis Rheum 59:1580–1588
Hertberger-Ten Cate R, de Vries-van der Vlugt BC, van Suijlekom-Smit LW, Cats A (1991) Intra-articular steroids in pauciarticular juvenile chronic arthritis, type 1. Eur J pediatr 150:170–172
Brostrom E, Hagelberg S, Haglund-Akerlind Y (2004) Effect of joint injections in children with juvenile idiopathic arthritis: evaluation by 3D-gait analysis. Acta Paediatr 93:906–910
Lepore L, Del Santo M, Malorgio C, Presani G, Petricarari S, Prodan M (2002) Treatment of juvenile idiopathic arthritis with intra-articular triamcinolone hexacetonide: evaluation of clinical effectiveness correlated with ANA and T gamma/delta + and B CD5+ lymphocyte populations of synovial fluid. Clin Exp Rheumatol 20:719–722
Huppertz HI, Tschammler A, Horwitz AE, Schwab KO (1995) Intraarticular corticosteroids for chronic arthritis in children: efficacy and effects on cartilage and growth. J Pediatr 127:317–321
Arabshahi B, Dewitt EM, Cahill AM, Kaye RD, Baskin KM, Towbin RB et al (2005) Utility of corticosteroid injection for temporomandibular arthritis in children with juvenile idiopathic arthritis. Arthritis Rheum 52:3563–3569
Cahill AM, Cho SS, Baskin KM, Beukelman T, Cron RQ, Kaye RD, Towbin RB (2007) Benefit of fluoroscopically guided intraarticular, long-acting corticosteroid injection for subtalar arthritis in juvenile idiopathic arthritis. Pediatr Rheumatol 37:544–548
Snels IA, Beckerma H, Twisk JW, Dekker JH, De Coning P, Koppe PA et al (2000) Effect of triamcinolone acetonide injections on hemiplegic shoulder pain: a randomized clinical trial. Stroke 31:2396–2401
Shupak R, Teitel J, Garvey MB, Freedman J (1988) Intraarticular methylprednisolone therapy in hemophilic arthropathy. Am J Hematol 27:26–29
Pal B, Morris J (1999) The perceived risks of joint infection following intra-articular corticosteroid injection: a survey of rheumatologists. Clin Rheumatol 18:264–265
Ostensson A, Geborek P (1991) Septic arthritis as a non-surgical complication in rheumatoid arthritis: relation to disease severity and therapy. Br J Rheumatol 30:35–38
Yangco BG, Germain BF, Deresinski SC (1982) Fatal gas gangrene following intra-articular steroid injection. Am J Med Sci 283:94–98
Kortelainen ML, Sarkioja T (1990) Fatal complications of intra-muscular and intra-articular injections. Z Rechtsmed 103:547–554
Hoelzer BC, Weingarten TN, Hooten WM, Wright AS, Wilson WR, Wilson PR (2008) Paraspinal abscess complicated by endocarditis following a facet joint injection. Eur J Pain 12:261–265
Gilsanz V, Bernstein BH (1984) Joint calcification following intra-articular corticosteroid therapy. Radiology 151:647–649
Cassidy JT, Bole GG (1966) Cutaneous atrophy secondary to intra-articular corticosteroid administration. Ann Int Med 65:1008–1018
Rogojan D, Hetland ML (2004) Depigmentation—a rare side effect of intra-articular glucocorticoid treatment. Clin Rheumatol 23:373–375
Parikh JR, Houpt JB, Jacobs ST, Fernandes BJ (1993) Charcot’s arthropathy of the shoulder following intraarticular corticosteroid injection. J Rheumatol 20:885–887
Berger RG, Yount WJ (1990) Immediate “steroid flare” from intraarticular triamcinolone hexacetonide injection: case report and review of the literature. Arthritis Rheum 33:1284–1286
Yamamoto T, Schneider R, Iwamoto Y, Bullough P (2006) Rapid destruction of the femoral head after a single intraarticular injection of corticosteroid into the hip joint. J Rheumatol 33:1701–1704
Cherasse A, Kahn MF, Mistrih R, Maillard H, Strauss J, Tavernier C (2003) Nicolau’s syndrome after local glucocorticoid injection. Joint Bone Spine 70:390–392
Blanco I, Krahenbuhl S, Schlienger RG (2005) Corticosteroid-associated tendinopathy. Drug Safety 28:633–643
Reis ND, Karkabi S, Zinman C (1989) Metatarsophalangeal joint dislocation after local steroid injection. J Bone Joint Surg Br 71:864
Quistgaard E, Christensen R, Torp-Pedersen S, Bliddal H (2006) Intra-articular treatment of hip osteoarthritis: a randomized trial of hyaluronic acid, corticosteroid and isotonic saline. Osteoarthritis Cartilage 14:163–170
Bollow M, Braun J, Taupitz M, Haberle J, Reibhauer BH, Paris S et al (1996) CT-guided intraarticular corticosteroid injection into the sacroiliac joints in patients with spondyloarthropathy: indication and follow-up with contrast-enhanced MRI. J Comput Assist Tomogr 20:512–520
Laroche M, Arlet J, Mazieres B (1990) Osteonecrosis of the femoral and humeral heads after intraarticular corticosteroid injections. J Rheumatol 17:549–551
Disclosures
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Habib, G.S., Saliba, W. & Nashashibi, M. Local effects of intra-articular corticosteroids. Clin Rheumatol 29, 347–356 (2010). https://doi.org/10.1007/s10067-009-1357-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-009-1357-y