Abstract
Systemic sclerosis (SSc) is a systemic autoimmune disease characterized by fibrosis of the skin and internal organs, which can cause significant morbidity and mortality. The prognostic factors for survival were not fully evaluated in Asian population. We investigated the prognostic factors for survival of SSc among Korean patients. A total of 243 SSc patients were enrolled from Seoul National University Hospital between 1972 and 2007. Age at onset, gender, cutaneous subset, autoantibody status, major organ involvement, and occurrence of malignancy were evaluated with all-cause mortality as the end point. A multivariate Cox proportional hazard model was used to retrieve the prognostic factors for survival. During the follow-up of 1,967 person-years, 33 patients died. Old age at onset (hazard ratio [HR] 7.4, 95% confidence interval [95% CI] 1.9–28.1), diffuse cutaneous subset (HR 2.5, 95% CI 1.1–5.9), presence of anti-Scl-70 antibody (HR 3.0, 95% CI 1.2–7.1), forced vital capacity less than 70% (HR 2.8, 95% CI 1.3–6.2), and heart involvement (HR 4.2, 95% CI 1.7–10.2) were found to be significant risk factors for mortality in multivariate analysis. In Korean SSc patients, old age, diffuse cutaneous involvement, anti-Scl-70 antibody, and internal organ involvement are risk factors for mortality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Systemic sclerosis (SSc) is a systemic autoimmune disease characterized by fibrosis of the skin and internal organs, possibly caused by genetic, environmental, and immunologic dysregulation [1]. It is a very rare disease, affecting 1.96–22.8 persons per million per year, occurring mostly in middle-aged women [2, 3]. Despite the significant improvement of prognosis in these patients with the introduction of angiotensin converting enzyme inhibitors, the 10-year survival rate for those with disease is still less than 70% [4–6].
The major cause of death in SSc is the involvement of the internal organs, including lungs, pulmonary arteries, and kidneys [6–11]. Several survival analyses performed in Caucasian SSc patients showed that the presence of a diffuse cutaneous subset, anti-Scl-70 antibody, pulmonary vascular disease, interstitial lung disease, renal involvement, and anemia are the risk factors for mortality [5–14]. Prognostic factors among Asian patients have been reported for Japanese and Thai populations [15, 16]. The significant risk factors in the Japanese study [15] were Barnett type III (diffuse), positive anti-Scl-70 antibody, and negative anticentromere antibody, while in the Thai study [16], significant risk factors were age >45 years and cardiac involvement. However, true survival risk factors are still not apparent in Asian populations because interrelationships among the clinical factors were not fully evaluated in either study. Therefore, we decided to investigate the survival risk factors in our single center cohort of Korean SSc patients.
Patients and methods
Study population
This is a retrospective cohort study. A total of 243 SSc patients were diagnosed as SSc in Seoul National University Hospital (SNUH) between January 1972 and 2007, and all of them fulfilled the American College of Rheumatology (ACR) preliminary classification criteria for SSc [17]. Of these, we excluded 13 patients with missing information regarding age and skin subset. Finally, 230 study subjects were analyzed. The patients were not limited to those visiting rheumatology clinic but all the patients who were cared at SNUH under the diagnosis of SSc were included.
The information for prognostic factors was collected as follows: age at enrollment and at diagnosis, gender, cutaneous subset, autoantibody status (anticentromere antibody, anti-Scl-70 antibody, and antiribonucleoprotein antibody), and major organ involvement including kidneys, heart, and lungs. The history of malignant diseases was collected from the National Central Cancer Registry by December 31, 2003. All SSc patients whose cancer status was not recorded in that registry were actively followed up for their cancer status in our outpatient department by June 2007. The survival status of patients was ascertained from National Death Certificate database by December 31, 2005, and the surviving SSc patients were actively followed up for their disease status in our outpatient department by June 2007. Therefore, we could ascertain survival status of all patients at June 2007. Among the 230 patients, 149 patients were actively followed up at our institute until the end point of the study. Since it is difficult to define when the disease begins, age at onset was defined as the age when the SSc was diagnosed.
The cutaneous subset was classified as diffuse or limited subsets based on the classification by LeRoy et al., focusing on the extent of skin involvement; limited subset was defined as those whose scleroderma was limited to the hands, face, feet, and forearms [18]. Major organ involvement was classified as follows: interstitial lung disease was defined as the presence of bibasilar pulmonary fibrosis in chest radiograph or high-resolution computed tomography without any evidence of other lung disease. Lung involvement was also analyzed based on forced vital capacity (FVC) [19]. Renal involvement was defined as serum creatinine over 1.2 mg/dl with elevation of blood pressure simultaneously or with the presence of microangiopathic hemolytic anemia. Heart involvement was defined as the presence of major conduction disturbance, ventricular arrhythmia, heart failure, or persistent pericardial effusion ≥2 months. Pulmonary hypertension was defined as systolic pulmonary artery pressure >35 mmHg with echocardiographic examination.
The Institutional Review Board of Seoul National University Hospital approved the study. Informed consent was exempted due to minimal risk for patients.
Statistical analysis
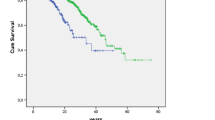
The frequency and means for clinical characteristics between the live and deceased patients were compared by Cox proportional hazard model adjusted for age and sex. Based on the backward elimination of the multivariate Cox regression model with the options of SLstay (significance level for the backward methods in SAS) = 0.1 and SLentry (value that is specified in the model statement in SAS) = 0.1, we selected the significant prognostic factors. The variables with more than 10% missing value (anti-Scl-70 antibody, antiribonucleoprotein antibody, pulmonary hypertension, and heart involvement) were also included in the multivariate analyses as a categorical variable to avoid distortion of real associations due to nonresponse. All values were presented as a hazard ratio with a 95% confidence interval. The survival curves were made by the Kaplan–Meier methods on the strata of specific variables. The 5-year and 10-year survival times were calculated by the life table method. All statistical tests were performed using SAS Version 9.1 for Windows. The survival graph was obtained with SPSS version 12 for Windows.
Results
Among the 230 SSc patients, 33 (14.3%) were deceased. Cumulative 5-year survival and 10-year survival rates were 85.4% and 80.1%, respectively. Median survival time was 27.4 years. Total follow-up time was 1,967 person-years. Mean age at onset was 43.7 ± 4.0 years old, and the male to female ratio was 1:8.
Clinical characteristics of the live and deceased patients are compared in Table 1. Age at onset, cutaneous subset, anti-Scl-70 antibody, impaired lung function (FVC < 70% or ≥70%), heart involvement, and pulmonary artery hypertension were significantly different between the live and deceased patients in univariate analyses adjusted for age and gender. The survival curve of each condition is described in Fig. 1. Mean survival times were significantly different depending on the age at onset (Age < 33 years, 28.3 years versus Age > 54 years, 12.5 years, p = 0.005), cutaneous subsets (limited, 31.8 years versus 20.0 years, p = 0.002), FVC (FVC ≥ 70%, 29.8 years versus FVC < 70%, 21.4 years, p = 0.034), or heart involvement (absence 26.6 years versus presence 12.5 years, p < 0.001).
The multivariate Cox proportional hazard model revealed old age at onset, diffuse cutaneous involvement, the presence of anti-Scl-70 antibody, heart involvement, and FVC < 70% as the risk factors associated with mortality (Table 2).
Discussion
In this study, we found that age, diffuse cutaneous subset, the presence of anti-Scl-70 antibody, FVC < 70%, and heart involvement are the risk factors for mortality in Korean patients with SSc. The results of our study are generally consistent with the previous Caucasian cohort studies in that aging, diffuse subset, presence of anti-Scl70 antibody, and involvement of the internal organs are the survival risk factors for SSc [5–14].
For lung involvement, FVC < 70%, not radiologic lung involvement, was a significant risk factor for survival in our cohort. Although interstitial lung disease can cause significant morbidity and mortality [4], it has diverse clinical courses ranging from stable, minimal involvement to severe progressive respiratory failure [20]. These results suggest that impaired lung function or the rate of decline might be genuine risk factors of mortality rather than the simple presence of any kind of impaired lung function [5, 21].
In this study, we could not find a significant association for the presence of anticentromere antibody, scleroderma renal crisis, or pulmonary hypertension with survival risk factors in Koreans. This does not indicate that these clinical variables are unimportant, but merely that they are important for very few of our patients. Korean SSc patients show low prevalence of anticentromere antibody (13.6% in this study), renal crisis (2.7%), and isolated pulmonary hypertension (2.1%) [22–24]. Low mortality (3.2%) of the patients with anticentromere antibody and high mortality of the patients with renal crisis (33.3%) suggest that these variables may contribute to survival. The pulmonary hypertension was associated with mortality in univariate analysis but failed to fit into the multivariate model since it was tightly related with lung involvement.
In this study, 5-year and 10-year survival rates of Korean patients were 85.4% and 80.1%, respectively. These values are comparable to the reported 75–90% and 64–81% in other populations [5–8]. Different survivals from different studies may reflect the population structure or prevalence of complication rates. The difference may also arise from the different definition of survival. Some defined it from diagnosis [6, 7] and others from the initial appearance of symptoms [8, 9].
In this study, only those who fulfilled the ACR criteria were included [17]. It has been reported that 15–39% of SSc patients, especially patients in the limited cutaneous subset, fail to satisfy the ACR criteria [18, 25]. Survival rates of Korean patients would improve if we applied more inclusive criteria for limited subset [18, 25].
There are several caveats in this study. First, the population in this study was a single center patient cohort. While a single center cohort often has the advantage of collecting a homogeneous population with the same diagnostic tools, it may not represent the Korean population as a whole. Although our population includes more patients who live in the Seoul area than in other areas, it does include a nationwide population, and the epidemiologic, clinical, and serologic characteristics of our cohort are very similar to the reports from other cohorts studied in Korea [22, 23] Second, this study has several limitations indigenous to retrospective study such as missing data and misclassification. Since the pulmonary artery pressure was not measured in all patients, some patients who had dyspnea or chest pain might have been classified into cardiac complications. Third, prevalence of anticentromere antibody was very low in our population. The prevalence of autoantibodies in systemic sclerosis can be different geographically and ethnically. For example, the prevalence of anticentromere antibody was reported to be lower in non-Caucasian than Caucasian [26]. Our lower prevalence of anticentromere antibody (13.6%) was consistent with prevalences of anticentromere antibody in other Korean studies (1.9–3.6%) [22, 23]. Fourth, prevalence of renal crisis is low in our population. In addition to low prevalence of anticentromere antibodies, rare renal crisis seems to be another feature of Korean patients with SSc. The previous Korean studies also reported 1.9 ~ 3.5% rate of SRC [22, 23]. In conclusion, the risk factors for mortality in Korean patients with SSc were age at onset, presence of anti-Scl-70 antibody, diffuse cutaneous subset, forced vital capacity of lung less than 70.0%, and cardiac involvement. Our results suggest that patients with SSc have similar prognostic factors regardless of their ethnic group.
References
Agarwal SK, Tan FK, Arnett FC (2008) Genetics and genomic studies in scleroderma (systemic sclerosis). Rheum Dis Clin North Am 34:17–40
Chifflot H, Fautrel B, Sordet C, Chatelus E, Sibilia J (2008) Incidence and prevalence of systemic sclerosis: a systematic literature review. Semin Arthritis Rheum 37:223–235
Mayes MD, Lacey JV Jr, Beebe-Dimmer J, Gillespie BW, Cooper B, Laing TJ et al (2003) Prevalence, incidence, survival, and disease characteristics of systemic sclerosis in a large us population. Arthritis Rheum 48:2246–2255
Steen VD, Medsger TA (2007) Changes in causes of death in systemic sclerosis, 1972–2002. Ann Rheum Dis 66:940–944
Simeon CP, Armadans L, Fonollosa V, Solans R, Selva A, Villar M et al (2003) Mortality and prognostic factors in spanish patients with systemic sclerosis. Rheumatol (Oxford) 42:71–75
Ferri C, Valentini G, Cozzi F, Sebastiani M, Michelassi C, La Montagna G et al (2002) Systemic sclerosis: demographic, clinical, and serologic features and survival in 1,012 Italian patients. Medicine 81:139–153
Al-Dhaher FF, Pope JE, Ouimet JM (2008) Determinants of morbidity and mortality of systemic sclerosis in Canada. Semin Arthritis Rheum. doi:10.1016/j.semarthrit.2008.06.002
Czirjak L, Kumanovics G, Varju C, Nagy Z, Pakozdi A, Szekanecz Z et al (2008) Survival and causes of death in 366 hungarian patients with systemic sclerosis. Ann Rheum Dis 67:59–63
Ioannidis JP, Vlachoyiannopoulos PG, Haidich AB, Medsger TA Jr, Lucas M, Michet CJ et al (2005) Mortality in systemic sclerosis: an international meta-analysis of individual patient data. Am J Med 118:2–10
Jacobsen S, Ullman S, Shen GQ, Wiik A, Halberg P (2001) Influence of clinical features, serum antinuclear antibodies, and lung function on survival of patients with systemic sclerosis. J Rheumatol 28:2454–2459
Hachulla E, Carpentier P, Gressin V, Diot E, Allanore Y, Sibilia J et al (2009) Risk factors for death and the 3-year survival of patients with systemic sclerosis: the French itinerair-sclerodermie study. Rheumatol (Oxford) 48:304–308
Jacobsen S, Halberg P, Ullman S (1998) Mortality and causes of death of 344 Danish patients with systemic sclerosis (scleroderma). Br J Rheumatol 37:750–755
Simeon CP, Armadans L, Fonollosa V, Vilardell M, Candell J, Tolosa C et al (1997) Survival prognostic factors and markers of morbidity in Spanish patients with systemic sclerosis. Ann Rheum Dis 56:723–728
Steen VD, Medsger TA Jr (2000) Severe organ involvement in systemic sclerosis with diffuse scleroderma. Arthritis Rheum 43:2437–2444
Nishioka K, Katayama I, Kondo H, Shinkai H, Ueki H, Tamaki K et al (1996) Epidemiological analysis of prognosis of 496 Japanese patients with progressive systemic sclerosis (SSc). Scleroderma Research Committee Japan. J Dermatol 23:677–682
Ruangjutipopan S, Kasitanon N, Louthrenoo W, Sukitawut W, Wichainun R (2002) Causes of death and poor survival prognostic factors in Thai patients with systemic sclerosis. J Med Assoc Thai 85:1204–1209
Subcommittee for scleroderma criteria of the American Rheumatism Association Diagnostic and Therapeutic Criteria Committee (1980) Preliminary criteria for the classification of systemic sclerosis (scleroderma). Arthritis Rheum 23:581–590
LeRoy EC, Black C, Fleischmajer R, Jablonska S, Krieg T, Medsger TA et al (1988) Scleroderma (systemic sclerosis): classification, subsets and pathogenesis. J Rheumatol 15:202–205
Goh NS, Desai SR, Veeraraghavan S, Hansell DM, Copley SJ, Maher TM et al (2008) Interstitial lung disease in systemic sclerosis: a simple staging system. Am J Respir Crit Care Med 177:1248–1254
Peters-Golden M, Wise RA, Schneider P, Hochberg M, Stevens MB, Wigley F (1984) Clinical and demographic predictors of loss of pulmonary function in systemic sclerosis. Medicine 63:221–231
Tashkin DP, Clements PJ, Wright RS, Gong H Jr, Simmons MS, Lachenbruch PA et al (1994) Interrelationships between pulmonary and extrapulmonary involvement in systemic sclerosis. A longitudinal analysis. Chest 105:489–495
Park SK, Kim TH, Jun JB, Jung SS, Bae SC, Kim TY et al (2001) The clinical features and autoantibody profile of progressive systemic sclerosis in Korea. J Korean Rheum Assoc 8:243–252
Lee EB, Han CW, Baek HJ, Kang SW, Cha HS, Kim HA et al (1999) Study on the clinical characteristics of systemic sclerosis. Korean J Med 57:1053–1061
Lee EB, Kim JY, Lee YJ, Abdallah A, Lympany P, Song YW (2004) Transforming growth factor-beta1 polymorphisms in Korean patients with systemic sclerosis. Tissue antigens 63:491–495
LeRoy EC, Medsger TA Jr (2001) Criteria for the classification of early systemic sclerosis. J Rheumatol 28:1573–1576
Cepeda EJ, Reveille JD (2004) Autoantibodies in systemic sclerosis and fibrosing syndromes: clinical indications and relevance. Curr Opin Rheumatol 16:723–732
Disclosures
None
Author information
Authors and Affiliations
Corresponding author
Additional information
Sources of support
This work was supported by a grant of the Korea Health 21 R&D Project, Ministry of Health, Welfare & Family Affairs, Republic of Korea (A030001, A084204).
Rights and permissions
About this article
Cite this article
Kim, J., Park, S.K., Moon, K.W. et al. The prognostic factors of systemic sclerosis for survival among Koreans. Clin Rheumatol 29, 297–302 (2010). https://doi.org/10.1007/s10067-009-1324-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-009-1324-7