Abstract
There have been marked changes in the management of juvenile idiopathic arthritis (JIA) over recent decades, mainly with earlier use of methotrexate (MTX). Our aim was to describe orthopaedic interventions in a large group of adults with JIA followed up over several decades. This was a retrospective observational study of adult JIA patients attending a teaching hospital clinic, with information collated on JIA subtype, disease duration, orthopaedic interventions, and exposure to MTX. The study included 144 patients with median disease duration of 19 years. Survival analysis showed that joint surgery was observed in the majority (75%) of patients with disease duration over 40 years with a trend for less joint surgery in patients with oligoarticular JIA. In total, 41 patients (28.5%) had received joint surgery, and 17/41 (41%) have required multiple procedures. Of those who have required joint surgery, 20/41 (48%) had started MTX in their adult years, with only 5/41 (12%), starting MTX prior to first joint replacement and none within 5 years of disease onset. Of the patients who have not had joint surgery to date, most (46/103, 45%) were receiving MTX or another immunosuppressive agent; in the majority of cases, MTX was started within 2 years of disease onset. Many adults with JIA require joint replacement surgery and ongoing immunosuppressive treatments, emphasising that JIA is not a benign disease. Many patients who have had joint replacement surgery have had exposure to MTX albeit after many years after disease onset; it remains to be seen whether patients who have received MTX therapy early in their disease course will ultimately have less requirement for joint surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The term juvenile idiopathic arthritis (JIA) encompasses a heterogeneous group of subtypes, based on clinical and serological features and with variable prognosis and outcome [1, 2]. Outcome studies of JIA demonstrate that over one third of patients have ongoing active disease into adulthood, report poorer health and functional outcomes than healthy individuals, and many experience sequelae of previous active disease including joint damage ultimately requiring joint replacement surgery, osteoporosis, reduced visual acuity, short stature, and adverse psychosocial impact with high unemployment [1, 3–11]. Outcome from joint replacement surgery in JIA is variable but studies report improvement in functional outcome, range of movement, and pain relief, although there is a high rate of complications including loosening, sepsis, periprosthetic fracture, and persistent pain [3–11].
Clearly, JIA is not a benign disease, and joint damage occurs early [12]; this has lead to earlier and more aggressive use of immunosuppressive treatments to optimise functional outcome and reduce the risk of joint damage [13]. The main therapeutic advances in JIA include the routine use of methotrexate (MTX), [14] intra-articular corticosteroids, and more recently, biologic and other anticytokine therapies [13–16]. For most children presenting currently with incident JIA, the expected outcome is that of remission without functional limitation albeit with the need to take potent immunosuppressive agents for many years. The ultimate aim of current management approaches is to optimise disease control, reduce long-term functional limitation, and avoid, or at least postpone, any requirement for joint replacement. The aim of this retrospective observational study was to describe the orthopaedic interventions in a large group of adults with JIA, spanning several decades of care, and to comment on the impact of earlier use of MTX.
Patients and methods
A clinic for adults with JIA was set up in 1995 within the adult Musculoskeletal Unit (a regional service at the Freeman Hospital), Newcastle Hospitals NHS Trust, in order to provide continuity of care for patients with JIA transferring from the children’s arthritis service (within the same NHS Trust) as well as the care for all adult patients with JIA, who were hitherto under the care of adult rheumatologists or orthopaedic surgeons within the same unit. Patients in the JIA continuity clinic have been managed by one consultant rheumatologist (Helen Foster), with all patients being classified using the International Leagus of Associations for Rheumatology (ILAR) criteria for JIA [2]. A previous cross-sectional study of outcome in this patient group demonstrated that many had ongoing active disease in adult years, with marked adverse psychosocial impact including high unemployment despite high educational attainment compared to healthy controls [15], and many have evidence of osteopenia [16]. For this current study, adult patients with JIA were identified from the departmental database and with a piloted proforma. The following data was collated from the case notes: patient demographics, JIA subtype, disease duration, age of disease onset, medication (including prior and current diseases modifying antirheumatic agents (DMARDs) and biologic agents), and orthopaedic surgical interventions. Data was entered into an Excel spreadsheet, and statistical analysis was performed using SPSS version 15.0. A Kaplan–Meier survival curve was plotted for the whole group with the first orthopaedic surgical intervention (invariably joint replacement) as failure point. Cox proportional hazards regression analysis was also performed with inclusion of age, gender, type of disease, age at onset, and MTX exposure (within 5 years of disease onset) as predictor variables of survival without joint surgery. A subsequent stepwise regression analysis was performed with inclusion of only significant (p < 0.05) covariates. For the purpose of the regression analysis, patients were grouped into oligoarticular and “non-oligoarticular subtypes” (the latter group being patients with a polyarticular course despite different onset subtypes) as a pragmatic attempt to analyse the effect of MTX exposure in the patient group. The study was registered with the Newcastle upon Tyne Hospitals NHS Trust Audit Department and was exempted from ethical approval.
Results
Patients
A total of 144 patients were identified (98/144 (68%) female), with a median age at the time of study of 25.5 years (range 17–75) and median disease duration of 19 years (range 1–67); notably a significant proportion (63/144, 44%) had disease duration of more than 21 years. Table 1 demonstrates that all subtypes of JIA were represented in the patient group; the majority having oligoarticular JIA (60/144, 42%), followed by polyarticular JIA (41/144, 28%, of whom 13/41 (32%) were rheumatoid factor (RF) positive), systemic onset JIA (17/144, 12%), and juvenile psoriatic arthritis (13/144, 9%), all of whom had a polyarticular course, and enthesitis-related arthritis (10/144, 4.8%) of whom three had developed classical ankylosing spondylitis in adult years. A further three patients were “unclassified” having overlapping features of more than one type (namely being HLA B27 positive, rheumatoid factor positive with a polyarticular course, and one patient also had psoriasis).
Orthopaedic surgery
Table 1 shows that within the total group, joint surgery has been required in 28.5% of patients and included a variety of procedures, namely: hip replacement(s) in 25/144 (17.4%), knee replacement(s) in 18/144 (12.5%), hip resurfacing (n = 2), shoulder replacement (n = 1), elbow replacement (n = 6), wrist arthroplasty (n = 4), wrist arthrodesis (n = 8), ankle arthroplasty (n = 2), ankle arthrodesis (n = 6), finger metacarpophalangeal joint multiple arthroplasty (n = 4), thumb interphalangeal joint fusion (n = 1), and talonavicular fusion (n = 1). Almost half of all patients with systemic onset and polyarticular JIA required multiple procedures, and this was significantly more than the other subtypes (p < 0.01, Chi-squared test); the requirement for joint surgery (any type) was more evident in those with rheumatoid factor positive rather than rheumatoid factor negative polyarticular JIA (31% versus 17%). Notably, within the oligoarticular JIA group, seven patients (7/60, 11.7%) required hip or knee joint replacement surgery.
The median time to first joint replacement was similar across the JIA subtypes (median 13 (range 4–49 years)), and the patient group who had undergone joint surgery (of any type) were older compared to those without joint surgery at the time of study (median age 41 years (range 27–75) and 26 years (range 17–60), respectively (p < 0.001)). Within the patient group with lower limb arthroplasties (n = 29 patients, 43 procedures), most patients had more severe forms of JIA (24% systemic onset JIA, 31% RF positive polyarticular onset JIA), long disease duration (80% being more than 21 years), and the median disease duration to joint surgery was lower for hip replacement compared to knee replacement (13 years (range 4–50) versus 28 years (range 8–60), respectively, p = 0.028, Mann–Whitney U test). A subgroup of nine patients (9/29 (31%)), required both bilateral hip and knee replacements, and joint surgery at one site was associated with requirement for further lower limb joint surgery (p < 0.001, Fisher’s exact test). Many patients required revision of lower limb arthroplasty (17/41, 41%), often needing multiple procedures (maximum nine hip replacements in one patient), and most had systemic onset or polyarticular onset JIA; although notably, two patients in this group had oligoarticular onset JIA. The median time from first joint surgery to revision knee replacement was 8 years (range 1 month–26 years) and to revision hip replacement being 13 years (range 3–20 years).
Methotrexate exposure
Within the total group, many patients (72/144, 50%) had been exposed to DMARD therapy, mostly MTX (53/72, 74%); although many of these individuals (34/53, 64%) had received other agents (many prior to 1995), invariably used sequentially and including sulphasalazine (8/34, 24%), leflunomide (5/34, 15%), gold (2/34, 6%), and penicillamine (2/34, 6%); in addition, in more recent years, many had been exposed to biologic treatments due to ongoing active disease and included etanercept (19/34, 56%), infliximab (6/34, 18%), and adalimumab (2/34, 6%). Many patients have had oral corticosteroids, although it was not possible from the case notes to establish the duration of exposure or the doses used. The median disease duration prior to MTX exposure was 13 years (range 0–33), which was similar across JIA subtypes with the exception of systemic JIA, with a shorter median of 3 years (1–30), albeit reflecting low numbers of patients. At the time of the study, many patients (31/144, 21.5%) were currently taking anticytokine agents including etanercept (n = 27), infliximab (n = 3), or adalimumab (n = 1) and invariably in combination with MTX. Notably, eight out of 41(19.5%) patients who had joint surgery previously were currently on MTX and etanercept, although in all cases, etanercept had been started many years after disease onset (89% > 10 years).
Of those patients who had undergone any form of joint surgery, many (20/41, 49%) had received MTX, including patients who had received lower limb arthroplasty (13/29, 45%). However, most of these patients had started MTX in their adult years with only 5/41(12%) starting MTX prior to the first joint replacement and none within the first 5 years of disease duration. In contrast, of the patients who have not had any joint surgery to date (n = 103), most are receiving MTX (46/103, 45%), and in many cases 12/46 (25%), this was started within 2 years of disease onset; notably in this group, many have prolonged disease duration (72/103, 70%) more than 10 years, median disease 20 years (range 5–36), and almost one third have severe forms of JIA (i.e., polyarticular and systemic onset subtypes 30/103, 29%).
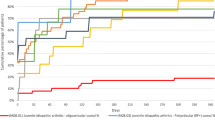
Kaplan–Meier survival analysis was performed for the whole group with the first joint surgery as endpoint (Fig. 1), with most patients (more than 75%) requiring joint surgery by 45 years of disease duration. Cox proportional hazards regression analysis (Fig. 2) was performed with age at the time of the study, gender, duration of disease, subtype of JIA, and MTX exposure within 5 years of disease onset as predictor variables of need for joint surgery. Stepwise regression analysis was performed with inclusion of significant (p < 0.05) covariates—amongst the predictor variables, none were significant other than JIA subtype (when grouped into oligoarticular and “non-oligo articular” types). However, a further linear stepwise regression analysis after splitting the “non-oligoarticular” group into various subtypes (i.e., polyarticular RF positive, polyarticular RF negative, systemic onset, and others) did not demonstrate the JIA subtype to be a significant factor. Joint surgery-free survival was significantly higher (p = 0.029) for the oligoarticular patients compared to other patients (pooled together and termed “non-oligoarticular”). Further analysis of those patients with non-oligoarticular JIA (n = 84) explored the influence of MTX exposure and other factors that may associate with the need for joint surgery (Table 2). Patients in this group who required joint surgery were significantly older at the time of the study with longer disease duration (p < 0.001), and although exposure to MTX was similar to those without joint surgery, the median disease duration prior to MTX exposure was significantly longer (p < 0.001). Notably, none of the non-oligoarticular JIA patients who had joint surgery had been exposed to MTX within 5 years of disease onset compared to 25% of those who have not had joint surgery to date. Moreover, in this subgroup analysis (Table 2), if disease duration is restricted to 25 years or less (i.e., the period in which methotrexate has been used), then the same significant effects are noted but with larger p values mainly due to the smaller sample sizes (particularly in the surgery group).
Discussion
JIA is a heterogeneous group of disorders with many patients having ongoing active disease into adult life or sequalae from previously active disease, resulting in functional limitation and worse quality of life compared to healthy controls [3, 9, 15, 17–23]. Most published outcome studies, however, are prone to selection bias towards more severe disease subtypes with patients recruited from specialist centres and are difficult to compare due to different methodologies and measures of outcome being used and different nomenclatures (such as juvenile chronic arthritis and juvenile rheumatoid arthritis) which have been replaced by the term JIA. Importantly, published outcome studies reflect management strategies from several decades ago, prior to routine use of MTX in clinical practise and the emergence of more potent immunosuppressive agents. Despite these limitations, however, it is clear that chronic arthritis starting in childhood is not a benign disease. Furthermore, the need for joint replacement surgery, especially lower limb arthroplasty, in adults with childhood chronic arthritis is also well reported along with significant complication and revision rates as a consequence of corticosteroid use, skeletal abnormalities from disease onset in childhood years, and osteopenia [3, 24]. Worse functional outcome and increased need for joint replacement surgery is reported in polyarticular onset JIA and prolonged disease duration, early hip involvement, and presence of rheumatoid factor [21, 22, 25–27]. More recent data have shown that worse baseline functional outcome is reported in delayed access to paediatric rheumatology care [15], and joint damage is more likely the longer the interval to starting MTX [1, 27]. Given the long latency from disease onset to emergence of joint damage and potential need for joint replacement, it is not surprising that there are no outcome studies to determine whether early use of immunosuppression such as MTX ultimately reduce the need for orthopaedic intervention.
This retrospective observational study describes adults with JIA with particular reference to orthopaedic interventions, namely joint replacement surgery, and we discuss the potential impact of current treatment strategies. We acknowledge the limitations of this study being biassed towards more severe JIA subtypes followed up in a tertiary unit and the patients not being an incident cohort. Furthermore, the spread of JIA subtypes is not typical of that observed in a regional paediatric rheumatology service, with a relatively low proportion of oligoarticular onset JIA and high proportion of patients with more severe subtypes, namely systemic onset JIA and rheumatoid factor positive polyarticular JIA. The data from the patient group, therefore, has to be interpreted with caution but, nonetheless, the observations are important; this is a large group of patients with protracted continuity of care in the same hospital service with available case note documentation of clinical disease course, treatment, and orthopaedic interventions. MTX was first used in Newcastle for JIA patients in 1993, and this is the first study to our knowledge to report orthopaedic interventions in patients spanning the decades pre- and postintroduction of MTX in routine clinical practise.
In the total patient group, there were relatively small numbers of patients within each JIA subtype, and pooling of all patients with a polyarticular course was a pragmatic attempt to analyse the data. This is logical given that the original ILAR classification refers to the JIA subtype in the first 6 months of disease course and has not been validated prospectively; although, anecdotally in clinical practise, many patients follow a polyarticular course despite the onset subtypes. Our survival analysis demonstrates a high overall need for joint replacement surgery within this patient group and predictably those with oligoarticular JIA having a significantly better prognosis with fewer joint replacements over time. Almost one third of patients required joint replacement surgery, predominantly lower limb arthroplasty and often, at multiple joints with high rates of revision surgery. Patients requiring joint surgery were more likely to be older, have longer disease duration, and more severe disease by JIA subtypes with polyarticular course; these findings are consistent with previous studies of poor outcome in JIA. The interval to first joint replacement was lower for those requiring hip replacement compared to other joint surgery and highlights hip disease as a poor prognostic indicator. The time to first revision lower limb arthroplasty was shorter for knee replacements compared to hips but similar to reported surgical outcomes for adults with JIA and shorter than surgical outcomes for adults with rheumatoid arthritis. The observation that a significant proportion of oligoarticular onset JIA patients also ultimately required joint replacement surgery and subsequent revision surgery emphasises the reported heterogeneity within this subtype [28] and that a benign course and outcome is not universal.
In the patient group as a whole, almost 50% had received DMARDs and particularly MTX, often after many years of other DMARDs beforehand. This reflects changes in clinical practise with evidence that other agents such as gold, penicillamine, and hydroxychloroquine have little benefit over placebo, and their use has become obsolete since the 1990s. In contrast to current clinical practise where MTX is invariably commenced at diagnosis in all subtypes except oligoarticular JIA, in the study population, there was often a prolonged interval from disease onset before starting MTX. A significant proportion of patients were also taking biologic agents at the time of the study, often in combination with MTX, and including several who have had previously joint replacement surgery; this observation reflects severity of ongoing disease activity into adult years, but notably, biologic therapy was started many years after disease onset and in all cases, many years after the first orthopaedic intervention. MTX exposure overall was similar in patients who had received joint replacement surgery or not (34% compared to 32%); although notably, few patients (12%) started MTX prior to the first joint replacement, and none started MTX within the first 5 years following disease onset. In contrast, within the patients who have not had joint surgery to date, many had started MTX within 2 years of disease onset—this subgroup is of particular interest as many have potentially severe subtypes of JIA, and already many have prolonged disease duration at the time of the study; it is intriguing to contemplate that their early exposure to MTX may reduce the need for joint surgery, and further follow-up of this subgroup is in progress. The impact of corticosteroids on the need for orthopaedic intervention in this patient group is difficult to ascertain given that many patients with more severe subtypes of JIA have had some exposure to corticosteroids at some time, and many patients are likely to have had osteopenia to some degree. However, given that orthopaedic intervention was required for some patients with oligoarticular JIA (and who were much less likely to have received oral corticosteroids), this study suggests that the pathogenesis of joint damage in JIA is complex and may only be addressed by long-term prospective studies.
In summary, this observational study of adults with JIA shows that many patients required joint replacement, usually lower limb arthroplasty, often at multiple sites, and that subsequent early revisions are not uncommon. Many patients reflect management prior to the routine use of MTX early in the disease course; although due to ongoing active disease in adult years, many have received immunosuppressive treatment including MTX and in some cases, combined with biologic agents. We also describe a subset of predominantly younger adults with JIA who have not required joint replacement surgery to date. Many of these patients have severe subtypes of JIA and are taking DMARDs (mainly MTX), some in combination with anticytokine agents, and in contrast to those having had joint surgery, they started MTX much earlier in their disease course. It remains to be seen whether this will ultimately result in fewer patients requiring joint replacement surgery.
References
Ravelli A, Martini A (2007) Juvenile idiopathic arthritis. Lancet 369:767–778
Petty RE, Southwood TR, Manners P, Baum J, Glass DN et al (2004) International League of Associations for Rheumatology classification of juvenile idiopathic arthritis: second revision, Edmonton, 2001. J Rheumatol 31:390–392
Williams WW, McCullough CJ (1993) Results of cemented total hip replacement in juvenile chronic arthritis. A radiological review. J Bone Joint Surg Br 75:872–874
Sarokhan AJ, Scott RD, Thomas WH, Sledge CB, Ewald FC, Cloos DW (1983) Total knee arthroplasty in juvenile rheumatoid arthritis. J Bone Joint Surg Am 65:1071–1080
Thomas A, Rojer D, Imrie S, Goodman SB (2005) Cemented total knee arthroplasty in patients with juvenile rheumatoid arthritis. Clin Orthop Relat Res 433:140–146
Parvizi J, Lajam CM, Trousdale RT, Shaughnessy WJ, Cabanela ME (2003) Total knee arthroplasty in young patients with juvenile rheumatoid arthritis. J Bone Joint Surg Am 85-A:1090–1094
Cage DJ, Granberry WM, Tullos HS (1992) Long-term results of total arthroplasty in adolescents with debilitating polyarthropathy. Clin Orthop Relat Res 283:156–162
Chmell MJ, Scott RD, Thomas WH, Sledge CB (1997) Total hip arthroplasty with cement for juvenile rheumatoid arthritis. Results at a minimum of ten years in patients less than thirty years old. J Bone Joint Surg Am 79:44–52
Lyback CO, Belt EA, Hamalainen MM, Kauppi MJ, Savolainen HA, Lehto MU (2000) Survivorship of AGC knee replacement in juvenile chronic arthritis: 13-year follow-up of 77 knees. J Arthroplasty 15:166–170
Witt JD, Swann M, Ansell BM (1991) Total hip replacement for juvenile chronic arthritis. J Bone Joint Surg Br 73:770–773
Rydholm U, Boegard T, Lidgren L (1985) Total knee replacement in juvenile chronic arthritis. Scand J Rheumatol 14:329–335
Wallace CA, Levinson JE (1991) Juvenile rheumatoid arthritis: outcome and treatment for the 1990s. Rheum Dis Clin North Am 17:891–905
Hashkes PJ, Laxer RM (2005) Medical treatment of juvenile idiopathic arthritis. Jama 294:1671–1684
Cespedes-Cruz A, Gutierrez-Suarez R, Pistorio A, Ravelli A, Loy A et al (2008) Methotrexate improves the health-related quality of life of children with juvenile idiopathic arthritis. Ann Rheum Dis 67:309–314
Foster HE, Marshall N, Myers A, Dunkley P, Griffiths ID (2003) Outcome in adults with juvenile idiopathic arthritis: a quality of life study. Arthritis Rheum 48:767–775
Bartram S, Foster H, Francis R (2000) Bone mineral density and juvenile chronic arthritis: comment on the article by Zak et al. Arthritis Rheum 43:710
Packham JC, Hall MA, Pimm TJ (2002) Long-term follow-up of 246 adults with juvenile idiopathic arthritis: predictive factors for mood and pain. Rheumatology (Oxford) 41:1444–1449
Packham JC, Hall MA (2002) Long-term follow-up of 246 adults with juvenile idiopathic arthritis: social function, relationships, and sexual activity. Rheumatology (Oxford) 41:1440–1443
Packham JC, Hall MA (2002) Long-term follow-up of 246 adults with juvenile idiopathic arthritis: education and employment. Rheumatology (Oxford) 41:1436–1439
Packham JC, Hall MA (2002) Long-term follow-up of 246 adults with juvenile idiopathic arthritis: functional outcome. Rheumatology (Oxford) 41:1428–1435
Oen K (2002) Long-term outcomes and predictors of outcomes for patients with juvenile idiopathic arthritis. Best Pract Res Clin Rheumatol 16:347–360
David J, Cooper C, Hickey L, Lloyd J, Dore C et al (1994) The functional and psychological outcomes of juvenile chronic arthritis in young adulthood. Br J Rheumatol 33:876–881
Peterson LS, Mason T, Nelson AM, O’Fallon WM, Gabriel SE (1997) Psychosocial outcomes and health status of adults who have had juvenile rheumatoid arthritis: a controlled, population-based study. Arthritis Rheum 40:2235–2240
Lehtimaki MY, Lehto MU, Kautiainen H, Savolainen HA, Hamalainen MM (1997) Survivorship of the Charnley total hip arthroplasty in juvenile chronic arthritis. A follow-up of 186 cases for 22 years. J Bone Joint Surg Br 79:792–795
Ruperto N, Ravelli A, Levinson JE, Shear ES, Murray K et al (1997) Long-term health outcomes and quality of life in American and Italian inception cohorts of patients with juvenile rheumatoid arthritis. II. Early predictors of outcome. J Rheumatol 24:952–958
Ruperto N, Levinson JE, Ravelli A, Shear ES, Link Tague B et al (1997) Long-term health outcomes and quality of life in American and Italian inception cohorts of patients with juvenile rheumatoid arthritis. I. Outcome status. J Rheumatol 24:945–951
Flato B, Lien G, Smerdel A, Vinje O, Dale K et al (2003) Prognostic factors in juvenile rheumatoid arthritis: a case-control study revealing early predictors and outcome after 14.9 years. J Rheumatol 30:386–393
Guillaume S, Prieur AM, Coste J, Job-Deslandre C (2000) Long-term outcome and prognosis in oligoarticular-onset juvenile idiopathic arthritis. Arthritis Rheum 43:1858–1865
Competing interest
None
Disclosures
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Malviya, A., Johnson-Lynn, S., Avery, P. et al. Juvenile idiopathic arthritis in adulthood and orthopaedic intervention. Clin Rheumatol 28, 1411–1417 (2009). https://doi.org/10.1007/s10067-009-1266-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-009-1266-0