Abstract
The objective of this study was to review all the published articles in the English literature about the systemic effects of intra-articular corticosteroid injection (IACI) in humans. Reports were searched through Pubmed using the terms intraarticular or intra-articular and steroids, corticosteroids, or glucocorticosteroids up and including the year 2007. Reports were also located through references of articles. Only objective findings outside the injected joint were included. The overwhelming majority of the studies was done at the knee joint and in rheumatoid arthritis/juvenile idiopathic arthritis patients. Many of the studies were done on the hypothalamic–pituitary–adrenal axis. Serum cortisol decreased within hours with a nadir after usually 24–48 h following the IACI. Recovery to baseline takes 1–4 weeks and sometimes longer depending on the type and dose of IACI and on the number of injected joints. Serum cortisol levels were blunted following adrenocorticotropic hormone stimulation in a small proportion of patients following methylprednisolone acetate injection and more common following other preparations. IACI resulted in a transient increase in blood glucose levels over few days in controlled diabetic patients with knee osteoarthritis. Peak levels are around 300 mg%. IACIs are associated with reduction in inflammatory markers like C-reactive protein and erythrocyte sedimentation rate that start few days following the IACI and could last for months. The effect on inflammatory cytokines is immediate with significant decrease within hours. IACI may induce remission also in patients with oligo-/polyarthritis and/or in patients with extra-articular manifestations. Other metabolic, hematologic, vascular, allergic, visual, psychologic, and other effects were also reported.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intra-articular corticosteroid injection (IACI) is a very popular therapeutic modality for local treatment of painful joints [1]. It has the advantage of locally delivering corticosteroids and less systemic spreading. The most commonly injected joint is the knee, and other joints like shoulder, wrist, tempero-mandibular joint, ankle and elbow are not infrequently injected [2]. The main indication for IACI is pain associated mainly with inflammatory or degenerative changes.
The first report on this modality of treatment was published in 1951 by Hollander [3]. This report had stimulated a widespread use of IACI. Later on, Hollander himself reported that branched esters were superior to hydrocortisone, and subsequently, esters of prednisolone, triamcinolone, and dexamethasone had been developed. Most of the currently used preparations were developed during the 1960s [4–7]. Some of the preparations are composed of two compounds [6, 7].
The most commonly used intra-articular corticosteroids (IAC) nowadays are methylprednisolone acetate (MPA), triamcinolone hexaacetonide (TH), triamcinolone acetanoide (TA), betamethasone acetate/betamethasone sodium phosphate (Celestone Chronodose), and betamethasone dipropionate/betamethasone sodium phosphate (Diprospan) [8].
In terms of comparative efficacy, 20 mg of TH was comparable to 40 mg of TA and to 40 mg of MPA in patients with juvenile idiopathic arthritis (JIA) [9].
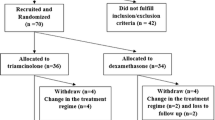
Materials and methods
In this review, we will present all that had been published about the systemic effects of these crystalloid steroids following IACI in humans in the English literature up and including the year 2007. Reports were searched through Pubmed using the terms intra-articular or intra-articular and steroids, corticosteroids or glucorticosteroids. Reports were also located through references of the articles. Only objective findings outside the injected joint were included, and subjective findings like patient or physician global assessment and pain following the IACI were not included. Cases that were subjective to different modalities of treatment in addition to IACI where the true contribution of IACI could not be assessed were not included. Also, studies talking about remission, especially in patients with juvenile idiopathic arthritis where the remission is due solely to complete improvement of the injected joint/s with the lack of extra-articular manifestations or distant swollen/tender un-injected joints that showed also complete improvement, were not included.
Before starting with the systemic effects, we will discuss what is known about the pharmacokinetics and pharmacodynamics of these compounds.
Results
Pharmacokinetics and pharmacodynamics
Following IACI of 40 or 80 mg of MPA at the knee joint in rheumatoid arthritis (RA) patients after maximal aspiration of synovial fluid, early levels of methyprednisolone (MP) were seen 30 min later with peak levels seen after 2–12 h (mostly after 4–8 h) and complete clearance from the blood after 5 days [10]. Maximal serum MP concentration and mean area under the curve were much higher following injecting the same dose but divided in both knees than in one knee. Similar pattern of levels were seen in both RA and osteoarthritis (OA) patients. The absorption from the knee joint is faster after joint evacuation of synovial fluid, while injecting into a knee with effusion will result in measurable serum levels of MP for a longer time [11].
Injecting betamethasone depot preparation at the knee joint had resulted in earlier serum peak levels of betamethasone within just 30 min with a half-life of 2 h [12].
Peak levels of triamcinilone were seen after 8 h following the injection of 20 mg of TH at the knee joint in RA patients [13]. There was no difference in the levels between resting and mobile patients. Complete absorption of TH and also of TA from the knee joint was observed over a period of 2–3 weeks following the IACI [14].
Remixolone, a relatively new IAC preparation, could be detected in the plasma over 3 months following an IACI of a single dose of 40 mg. The suspension dissolves very slowly in the joint cavity [15].
The mean residence time of the different IAC preparations at the knee joint was 25, 6, 3.8, 2.8, and 2.6 days for remixolone, TH, TA, betamethasone acetate, and MPA, respectively [19]. It had been shown that the duration of the clinical effectiveness of different IAC preparations correlates well with their mean residence time [16].
Systemic effects
Table 1 summarizes all the reported systemic effects.
Endocrine
-
(a)
Hypothalamic–pituitary–adrenal (HPA) axis: The effect on the HPA axis is the most studied topic in this field [10, 13, 17–30]. Under this topic, we will summarize the studies that were done on cortisol levels (plasma, saliva, and 24-h urine cortisol) [10, 13, 17–21, 23–26, 29, 30], adrenocorticotropic hormone (ACTH) levels [13, 19–21, 30], and ACTH stimulation tests [18, 26–28].
The overwhelming majority of these studies were done on RA or JIA patients, and the knee was the most commonly injected joint.
Following a single injection of different IAC preparations at the knee joint, there was a significant reversible decrease in serum cortisol levels [10, 13, 18, 19, 23–26, 29, 30]. The earliest significant decrease could be seen within just 4 h [26]. Maximal suppression would be seen after 24–48 h and rarely up to 4 days [10, 13, 23–26, 29].
In a few studies only, no effect of IACI on blood cortisol levels was found.
The level and duration of suppression are dependent on the type of preparation, dose, and number of injected joints. Higher dose and longer residence time at the joint of the injected IAC preparation will have deeper and prolonged suppressive effect [15, 21]. Also, splitting the dose between two or more joints will have more and longer suppressive effect than giving the total dose at one joint [10].
Normalization of plasma cortisol levels will usually occur 1–2 weeks following IACI of usual doses of MPA, betamethasone, and cotrivazole [6, 26]. As for TH, it usually takes 2–4 weeks [21]. There are few studies with TA, where normalization was observed within 28 days [23].
Saliva cortisol level, which is considered reliable in reflecting plasma cortisol levels, were suppressed for a median of 16 days in 22 children with chronic arthritis who received IACI of 20–60 mg of TH, mostly at the knee joint. Normalization of levels was seen before day 28 in 95% of the patients [21].
Twenty-four-hour urine cortisol levels decreased significantly the day after the injection of 20 mg of TH at the knee joint in 20 RA patients with active synovitis [13]. ACTH levels also decreased significantly the day after the injection; however, it normalized after 48 h [13]. In another study, ACTH levels were undetectable from day 2 to at least 1–2 weeks following IACI of usual doses of betamethasone or cotrivazole at the knee joint and following IACI of cotrivazole at the ankle or wrist joints [26].
Although serum cortisol levels were deeply suppressed during the early days following different IACIs, ACTH stimulation test showed mixed results. ACTH stimulation test of 1 μg of tetracosactide hexaacetate (Synacthen, Novartis Pharma, Basel, Switzerland) in 25 patients with rheumatic diseases following IACI of 20–160 mg of MPA mostly at the knee joint resulted in blunted peak cortisol response in one, three, and one patients at days 1, 7, and 14, respectively, following the IACI [18]. However, normal response was observed following 0.25 mg of ACTH1–24 (Cortrosyn®, Organon, Holland) stimulation at days 3, 7, and 14 after an IACI of 20 mg of TH at the knee joint in ten RA patients.
One microgram of ACTH stimulation 2 days after IACI at the knee joint of 7 mg of betamethasone in three patients, of 3.75 mg of cotrivazole in three patients, and of 1.85 mg of cotrivazole at the ankle joint in one patient, all with sport injury, resulted in suppressed serum cortisol levels 30 min later in all of them [26].
Regarding multiple injections, two out of eight patients treated regularly by IACIs of MPA (160 mg/visit) for periods ranging from 1 to 11 years at intervals of 5–6 weeks showed suppression of cortisol levels following ACTH stimulation and insulin stress tests 5–6 weeks after the last injection [28].
-
(b)
Cushing’s syndrome: Based on what was mentioned before, it is not surprising to encounter reports of Cushing’s syndrome following IACI [22, 27, 31–33]. Most of the cases had been reported in JIA patients [30, 32, 33]. It is usually seen after repetitive injections [27, 31, 32] and sometimes after even one [32] or two injections [26, 32]. It is much more reported following IACIs of TA [31], where prevalence was about 5% among a large group of patients with JIA from one center, than with TH where the prevalence was about 0.5% [31]. It usually develops weeks after the last injection [31]. Signs of moon face and buffalo hump usually resolve after 4–6 months [31, 32] and sometimes up to 11 months following the last injection [22].
Metabolic
-
(a)
Glucose metabolism: There are very few reports on this topic. In a case report from 1989, an IACI of 4 mg of betamethasone at the knee joint had resulted in a very high level of serum glucose of 1,000 mg/dl 2 h following the injection in an aged patient [34]. In a prospective study done by us in diabetic patients with painful shoulders, an injection of 35 mg of MPA at the gleno-humeral joint had no significant effect on blood glucose or fructosamine levels [35]. However, following IACI of 50 mg of MPA at the knee joint in controlled diabetic patients with symptomatic osteoarthritis of the knee, we showed significant increase in blood glucose levels as early as 2 h with peak levels seen after a few to 24 h following the injection in all the patients [36]. Peak levels could reach 500 mg/dl but mostly around 300 mg/dl. The significant increase usually lasted 2–3 days and up to 5 days. In some patients, the increase in glucose levels was very mild. On the other hand, injecting 1 ml of Celestone Chronodose at the knee joint had resulted in a brisk significant increase in blood glucose levels in all the patients within 1 h and returning to pre-injection levels mostly within 2 days [37]. Maximal levels were similar to those obtained following MPA injection.
-
(b)
Cholesterol and triglycerides: No significant effect was seen after three consecutive injections of 1.5 ml of cortivazole at the shoulder joint on cholesterol or triglyceride levels [19].
-
(c)
Bone and cartilage: Cartilage oligomatrix protein (COMP) and osteoacalcin, markers of cartilage turnover and bone formation, respectively, were decreased significantly when collected 1, 2, 7, and 14 days after IACI of 20 mg of TH [38]. COMP decreased more significantly in resting patients (for 24 h). Deoxypyridinoline, a marker of bone resorption, did not decrease in either group. In another study assessing the effect of 40 mg of TA injected mainly at the knee joint in RA patients at days 1, 3, 7, 14, and 28 following the injection, there was a drastic decline of serum osteocalcin 1 day after the IACI and returned to pretreatment levels on day 14. There was no effect on urinary pyridinoline, a bone resorption marker [23].
-
(d)
Growth suppression: After one IACI of 20 mg of TH into the knee of two patients with JIA, there was a transient suppressive effect of the growth of the contralateral lower leg detected by knemometry [39].
-
(e)
Electrolytes: No effect was seen after three consecutive injections of 1.5 ml of cortivazole at the shoulder joint on serum sodium or potassium levels [19].
Inflammatory markers and cytokines
-
(a)
Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP): One week following an IACI at one or both knees, there was a significant drop in CRP and ESR in a cohort of 20 RA patients. The mean drop was 46% in both, and the effect lasted over a variable period up to 6 months [40].
IACI of 40 mg of TH at the knee joint in six RA patients had resulted in a significant decrease in CRP levels in five patients when repeated after <21 days and in four patients when repeated after 50–80 days following the IACI [41]. There was a significant decrease in one out of five patients with ankylosing spondylitis. In another study, there was about 16% decline in ESR at day 3 and 24% decline at day 28 following an IACI of 40 mg of TA injected mainly at the knee joint in RA patients [23].
-
(b)
Cytokines: Following IACI of MPA at doses of 40–240 mg total at either one or more and up to five major joints at one setting in six RA patients, tumor necrosis factor alfa (TNFα) release after lipopolysaccharide (LPS) stimulation was low when analyzed after 4, 8, 12, 24, 48, and 96 h later [25]. Maximal suppression was at 4 and 8 h. Mifepristone, a glucocorticoid antagonist, restored the LPS stimulated release.
In a case of active RA, IACI of 20 mg of TA at the knee joint had resulted in a significant decrease in six key inflammatory regulators: IL-2, IL-4, IL-6, IL-7, IL-17, and TNFα. There was no significant change in IL-1β, IL-13, granulocyte colony-stimulating factor (CSF), granulocyte-macrophage CSF and MCP-1 [42].
Hematologic
-
(a)
Sickle cell crisis: Two cases of RA, with sickle cell disease in one and trait in the other, developed sickle cell crisis following IACI of 40 and 80 mg of MPA at the knee joint [43]. Both were female. The first patient developed it thrice, 12–48 h following the injection and the second patient developed it twice, 12–24 h following the injection.
-
(b)
Peripheral blood leucocytes: An IACI of MPA of a total dose of 40–240 mg at either one or more (up to five major joints simultaneously) in six RA patients resulted in a significant fall in circulating lymphocytes and monocytes when evaluated at 4, 8, 12, and 24 h later [25]. However, these cells had recovered when evaluated at 48 h, and a significant lymphocytosis had developed by 96 h. Granulocyte count did not change during the first 12 h but increased by nearly double fold by 24 and 48 h. By 96 h, their number was not significantly different than at baseline.
An IACI of 80 mg of MPA at the knee joint in eight women with inflammatory arthritis, mostly RA, had resulted in an increase in leukocyte count above the normal limits as early as 8 h in two patients. Peak levels were mostly seen after 24 h.
-
(c)
Viscosity: Following an IACI of 40, 20, and 20 mg of MPA, TH, or prednisolone tertiary butyl acetate, respectively, in patients with RA, plasma viscosity fell slightly (not significant) by 6 weeks in all three groups [29].
Vascular
-
(a)
Blood pressure: A study with three consecutive injections of 3 days apart each at the shoulder joint of 1.5 ml of cortivazole resulted in a modest but significant increase in systolic blood pressure on days 1 and 7 after the last injection. On day 21, it was normal [19].
In evaluating simultaneous polyarticular IACIs of TA with a total dose of 234 ± 26.2 mg vs. intra-muscular (IM) injection of a similar dose in the treatment of RA patients, the IAC group had significantly lower systolic blood pressure levels when compared to baseline and assessed at weeks 1, 4, 12, and 24 after the injection, while the IM group had significantly higher diastolic blood pressure during follow-up as compared to baseline [20].
-
(b)
Flushing: In a group of consecutive patients with different rheumatic diseases who received IACI of 40 mg of TA and had a follow-up, 40 out of 100 patients (40%) reported facial flushing on questionnaire and serious flushing in 15 (15%) [44]. This symptom appeared on average 19 h after the injection and lasted on average 36 h. Of those who needed a repeated injection, six were injected with TA, and all (100%) had repeated flushing, while 18 patients were injected with TH, and only nine (50%) of them developed flushing. The flushing was more common among females.
Effect on distant joints and/or extra-articular manifestations in patients with chronic arthritis
In a study evaluating three different preparations, MPA, TH, and prednisolone tertiary butyl acetate at doses of 40, 20, and 20 mg respectively in 30 RA patients with bilateral synovitis of both knees, only the TH group showed improvement at the contralateral knee [30].
Following IACI at the knee joint of either 4 mg of dexamethasone tertiary butyl acetate (nine patients) or 80 mg of MPA (11 patients) in 20 patients, mostly RA patients, there was an improvement in all the patients in at least two of the following parameters: articular index, swollen joint count, or joint effusion [45]. Regarding hand grip, seven out of 18 patients showed improvement, more promising in the MPA group.
IACI of a total dose of 40 mg of TH injected at four joints in a patient with JIA resulted in a transient remission with an immediate disappearance of fever and rash that were part of his disease [46]. This effect lasted for 3 weeks after adding also methotrexate and ibuprofen.
Five out of six patients with JIA who were given IACI for active arthritis and had also active iritis had remission of eye inflammation for a mean of 9 months (range 3–25) afterwards [33].
In a study following 21 children with chronic arthritis, two patients had atopic dermatitis that abated following TH injection but worsened 4–6 weeks later [47].
Other effects
Anaphylaxis and other allergic reactions
Anaphylactic shock following IACI was reported in several cases [48–50]. The reactions were typical of classic anaphylactic shock with symptoms and signs developing as early as just few seconds after the termination of the injection [49] minutes [48, 50] or even few hours later. All the patients were treated with subcutaneous injection of adrenalin and some of them with systemic steroids mostly hydrocortisone [49] and or antihistamines. No fatality was recorded.
In two cases, skin tests were done; in one, it was positive or the injected steroid (triamcinolone) and negative for other steroids, and in another case, it was positive for paramethasone and other steroids but negative to hydrocortisone.
Other than anaphylaxis, there were very few reports of less severe allergic reactions [2]
Visual
There are few reports of hallucinations following IACI. Idiopathic central serous chorioretinopathy following IACI of 40 mg of TA at the wrist joint was reported in a 36-year-old woman [51]. She presented 1 day following the injection with impaired vision. Her visual impairment improved totally over a period of 5 weeks spontaneously.
Psychological effect
Behavioral changes were reported in two cases following IACI of 80 mg of MPA at the shoulder or hip joint [52, 53]. The first developed agitation and disorientation the next day and the other paranoid delusions and visual and auditory hallucinations. The first case was treated with chlorpromazine, and in the other, symptoms resolved spontaneously after 3 days.
Infections
An independent 89-year-woman with bilateral OA of the knees and no previous medical history of significance developed systemic tuberculosis with pulmonary and knee involvement 2 months following a second IACI (type not specified). Patient died due to severe sepsis leading to her death later [54] with subsequent growth of mycobacterium tuberculosis from sputum and synovial fluid cultures.
Hyaluronic acid
Hyaluronan (HA) has a major role in regulating synovial fluid volume. Following an IACI of 40 mg of TH, there was a significant decrease in the serum level of HA of all eight patients with RA by about 59% in contrast to an increase in synovial HA in these patients. In OA patients (eight patients) the opposite phenomenon was obtained. In most of ankylosing spondylitis patients, there was no change in the level of either serum HA or synovial HA [41].
Hiccups
Although hiccups may develop after intravenous treatment of steroids, it was reported in only one case following each IACI [55]. In both times, it developed the next day after the injection, lasting for 24 h in the first (disappeared without medications) and for 2 weeks (relieved only after levomepromazine treatment) in the second time.
Effect on other meds
IACI of different preparations, mostly MPA, had resulted in a decrease of more than 40% in serum salicylate level due to increased renal clearance [56]. The nadir was seen 19 h on average following the injection. This effect is more pronounced once both knees are injected simultaneously.
Discussion
Although IACs are given locally at one or more joints, a significant proportion of the injected compound will be absorbed resulting in significant measurable serum levels over days to weeks following the injection depending on the type and dose of the preparation and also on the number of injected joints. It must be remembered that the overwhelming data comes from studies done at the knee joint.
The spectrum of known systemic effects of IACI in some way is similar to that following oral or intravenous root of administration but still limited. However, the characteristics of these effects are different, and this is mainly due to the formulation of the IAC, a branched ester and also due to the place of injection, the cavity of the joint. Some of the effects following IACI were peculiar and unique, that were not described following the oral or intravenous roots of administration like the sickle cell crisis in patients with sickle cell disease.
As had been shown, the HPA axis is the most studied topic where most studies had shown a sharp drop of serum cortisol level within hours to very low or undetectable levels following IACI. This nadir lasts mostly for 2 days and sometimes up to 4 days. The level and duration of suppression and recovery are dependent on dose and type of IAC preparation and also on the number of joints injected. Recovery is faster following MPA and betamethasone depot injection and longer following the acetonides. Although the early suppression is so profound, only very few patients from those who had an IACI with MPA had a blunted serum cortisol response following ACTH stimulation test, while following IACI of betamethasone preparations and cotrivazole, the percentage of patients with blunted response is higher. These findings may have a major impact on patients who are exposed to stressful events like surgical procedures within a short period of time following IACI. The adrenal gland should be assessed for its ability to secrete endogenous steroids before embarking on stressful procedures.
Our data on the effect on glucose metabolism is pioneering with the previous lack of needed information that already exists for oral or intravenous administration of steroids. Prior to these studies, actually a diabetic patient could not have a reliable answer for a legitimate question by him: Doc, how will the injection affect my diabetes? So it can be said that controlled diabetic patients will have a transient significant increase in blood glucose levels for a few days following IACI at the knee joint. The pattern of increase following the Celestone-Chronodose is quite uniform with an abrupt significant increase in blood glucose levels within the first hour following the injection and decline to normal levels after about 48 h. Mean peak levels are around 300 mg%. Blood glucose increase following MPA injection is more gradual and in some is minimal with similar mean peak levels. More studies are needed to explore the effects of the injection of other IAC preparations at the knee joint, other joints, or even following IACI at multiple joints simultaneously.
IACI had not only a positive subjective effect on pain alleviation at remote joints but also positive objective findings within a short period of time reflecting early appearance of significant levels of the corticosteroid at the serum. As expected, IACI resulted in a decrease in both classic inflammatory markers, the ESR and CRP. The level of decrease is variable but apparent within days lasting for weeks to months. There was an immediate significant decline in inflammatory cytokines like IL-2, IL-4, IL-6, IL-7, IL-17, and TNFα within just few hours following the IACI. There were also cases of remission especially in JIA patients with multiple joint involvements where an IACI at a single joint had a remissible effect on distant joints and also on extra-articular manifestations.
There are nearly no reports linking IACI with systemic infections. There is one case report of pulmonary and articular tuberculosis following IACI in a very old woman. Alertness to tuberculous infection in patients with advanced age, immune-suppression, or comorbidities with or without a history of tuberculosis is recommended.
The clinical significance of reduced serum levels of acetylsalicylic acid following IACI in patients treated with aspirin for different indications is still not known. It may be that patients on chronic aspirin treatment need to increase the dose of their aspirin for few days more or less following IACI. More studies are needed to explore the consequences of this effect.
References
Snippe JC, Gambardella RA (2005) Use for injections in osteoarthritis in joints and sports activity. Clin Sports Med 24:83–91
Caldwell JR (1996) Intra-articular corticosteroids. Guide for selection and indications for use. Drugs 52:S07–S14
Hollander JL, Brown EM, Jessar RA, Brown CY (1951) Hydrocortisone and cortisone injected into arthritis joints: comparative effects and use of hydrocortisone as a local antiarthritic agent. JAMA 147:16329–16335
Schwartz S (1960) Intra-articular administration of triamcinolone acetonide: a preliminary report. N Y State J Med 60:3422–3425
Kendall PH (1967) Triamcinolone hexacetonide. A new corticosteroid for intra-articular therapy. Ann Phys Med 9:55–58
Norcross BM, Winter JA (1961) Methylprednisolone acetate: a single preparation suitable for both intra-articular and systemic use. N Y State J Med 61:552–561
Roberts HJ (1965) Local injection of a preparation containing two betamethasone esters in the treatment of noninfectious musculoskeletal disorders. J Am Geriatr Soc 13:275–291
Centeno LM, Moore ME (1994) Preferred intraarticular corticosteroids and associated practice; a survey of members of the American college of rheumatology. Arthritis Care Res 7:151–155
Zulian F, Martini G, Gobber D, Plebani M, Zacchello F, Manners P (2004) Triamcinolone acetanoide and hexacetonide intra-articular treatment of symmetrical joints in juvenile idiopathic arthritis: a double-bind trial. Rheumatology (Oxford) 43:1288–1291
Armstrong RD, English J, Gibsn T, Chakraborty J, Marks V (1981) Serum methylprednisolone levels following intra-articular injection of methylprednisolone acetate. Ann Rheum Dis 40:571–574
Bertouch JV, Sallustio BC, Mefflin BJ, Brooks BM (1983) A comparison of plasma methylprednisolone concentrations following intraarticular injection in patients with rheumatoid arthritis and osteoarthritis. Aust N Z Med 13:583–585
Gless KH, Klee HR, Vecsei P, Weber M, Haack D, Lichtwakd K (1981) Plasma concentration and systemic effect of betamethazone following intraarticular injection. Disch Med Wschr 106:704–707
Weitof T, Ronnblom L (2006) Glucocorticoid resorption and influence on the hypothalamic-pituitary-adrenal axis after intra-articular treatment of the knee in resting and mobile patients. Ann Rheum Dis 65:955–957
Derendorf H, Mollmann H, Gruner A, Haack D, Gyselby G (1986) Pharmacokinetics and pharmacodynamics of glucocorticoid suspensions after intra-articular administration. Clin Pharmacol Ther 39:313–317
Derendorf H, Mollman H, Voortman G, van den Ouweland FA, van de Putte LB, Gevers G et al (1990) Pharmacokinetics of rimexolone after intra-articular administration. J Clin Pharmacol 30:476–479
Blyth T, Hunter JA, Stirling A (1994) Pain relief in the rheumatoid knee after steroid injection: a single blind comparison of hydrocortisone succinate, and triamcinolone acetonide or heaxacetonide. Br J Rheumatol 3:461–463
Lazarevic MB, Skosey JL, Djordjevic-Denic G, Swedler WI, Zgardic I, Myones BA (1995) Reduction of cortisol levels after single intra-articular and intramuscular steroid injection. Am J Med 99:370–373
Mader R, Lavi L, Luboshitzky R (2005) Evaluation of the pituitary-adrenal axis function following single intraarticular injection of methylprednisolonone. Arthritis Rheumatism 52:924–928
Younes M, Neffati F, Touzi M, Hassan-Zrour S, Fendri Y, Bejia I et al (2007) Systemic effects of epidural and intra-articular glucocorticoid injections in diabetic and non-diabetic patients. Joint Bone Spine 74:472–476
Furtado RN, Oliveira LM, Natour J (2005) Polyarticular corticosteroid injection versus systemic administration in treatment of rheumatoid arthritis patients: a randomized controlled study. J Rheumatol 32:1691–1698
Schweitzer DH, Le-Brun PP, Krishnaswami S, Derendorf H (2000) Clinical and pharmacological aspects of accidental triamcinolone acetonide overdose; a case study. Neth J Med 56:12–16
Huppertz HI, Pfuller H (1997) Transient suppression of endogenous cortisol production after intraarticular steroid therapy for chronic arthritis in children. J Rheumatol 24:1833–1837
Emkey RD, Lindsay R, Lyssy J, Weisberg JS, Dempster DW, Shen V (1996) The systemic effect of intraarticular administration of corticosteroid on markers of bone formation and bone resorption in patients with rheumatoid arthritis. Arthritis Rheum 39:277–282
Lzarevic MB, Skosey JL, Djordjevic-Denic G, Swedler WI, Zgradic I, Myones BL (1995) Reduction of cortisl levels after single intra-articular and intramuscular steroid injection. Am J Med 99:370–373
Steer JH, Ma DT, Dusci L, Garas G, Pedersen KE, Joyce DA (1998) Altered leukocyte trafficking and suppressed tumor necrosis factor alpha release from peripheral blood monocytes after intra-articular glococorticoid treatment. Ann Rheum Dis 57:732–737
Duclos M, Guinot M, Colsy M, Merle F, Baudot C, Corcuff JB et al (2007) High risk of adrenal insufficiency after a single articular steroid injection in athletes. Med Sci Sports Exerc 39:1036–1043
O’Sullivan MM, Rumfeld WR, Jones MK, Williams BD (1985) Cushing’s syndrome with suppression of the hypothalamic-pituitary-adrenal axis after intra-articular steroid injections. Ann Rheum Dis 44:561–563
Reid DM, Eastmond C, Rennie JAN (1986) Hypothalamic-pituitary-adrenal axis suppression after repeated intra-articular steroid injection. Ann Rheum Dis 45:87
Esselinckx W, Bacon PA, Ring EFJ, Crooke D, Collins AJ, Demottaz D (1978) A thermographic assessment of three intra-aricular prednisolone analogues given in rheumatoid synovitis. Br J Clin Pharmac 5:447–451
Weiss S, Fischel B, Kisch ES (1980) Systemic effect of intra-articular steroid preparations. Ann Rheum Dis 39:413–414
Gondwe JS, Davidson JE, Deeey S, Sills J, Cleary AG (2005) Secondary Cushing’s syndrome in children with juvenile idiopathic arthritis following intra-articular triamcinolone acetonide administration. Rheumatology (Oxford) 44:1457–1458
Kumar S, Singh RJ, Reed AM, Lteif AN (2004) Cushing’s syndrome after intra-articular and intradermal administration of triamcinolone acetanoiode in three pediatric patients. Pediatrics 113:1820–1824
Bloom BJ, Miller LC, Tucker LB, Alario AJ, Schaller JG (1997) Intra-articular corticosteroids in juvenile chronic arthritis. Arthritis Rheum 39:S46
Black DM, Filak AT (1989) Hyperglycemia with non-insulin-dependent diabetes following intraarticular steroid injection. J Fam Pract 28:462–463
Habib G, Anu-Ahmad R (2007) Lack of effect of corticosteroid injection at the shoulder joint on blood glucose levels in diabetic patients. Clin Rheum 26:566–568
Habib G, Bashir M, Jabbour A (2008) Increased blood glucose levels following intra-articular injection of methylprednisolone acetate in controlled diabetic patients with symptomatic osteoarthritis of the knee. ARD 67:1790–1791
Habib GS, Safia A (2009) The effect of intra-articular steroid injection of betamethasone acetate/betamethasone sodium phosphate on blood glucose levels in controlled diabetic patients with symptomatic osteoarthritis of the knee. Clin Rheum 28:85–87
Weitoft T, Larsson A, Saxne T, Ronnblom L (2005) Changes of cartilage and bone markers after intra-articular glucocorticoid treatment with and without postinjection rest in patients with rheumatoid arthritis. Ann Rheum Dis 64:1750–1753
Heuck C, Wolthers OD, Herlin T (1999) Growth-suppressive effect of intra-articular glucocorticoids detected by knemometry. Horm Res 52:95–96
Taylor HJ, Fowler PD, David MJ, Dawes PT (1991) Intra-articular steroid: cofounder of clinical trials. Clin Rheumatol 10:38–42
Pitsillides AA, Will RK, Bayliss MT, Edwards JCW (1994) Circulating and synovial fluid hyaluronan levels. Arthritis Rheum 37:1030–1038
Alex P, Szodoray P, Arthur E, Willis L, Hynd R, Flinn D et al (2007) Influence of intraarticular corticosteroid administration on serum cytokines in rheumatoid arthritis. Clin Rheumatol 26:845–848
Gladman DD, Bombardier C (1987) Sickle cell crisis following intraarticular steroid therapy for rheumatoid arthritis. Arthritis Rheum 30:1065–1068
Pattrick M, Doherty M (1987) Facial flushing after intra-articular injection of steroid. Br Med J (Clin Res Ed) 295:1380
Koehler BA, Urowitz MB, Killinger DW (1974) The systemic effects of intra-articular corticosteroids. J Rheum 1:117–125
Magni Manzoni S, Viola S, Beduschi L, Martini A, Ravelli A (2002) Transient remission of systemic manifestations following intraarticular triamcinolone hexacetanoide injection in a boy with systemic juvenile idiopathic arthritis. Clin Exp Rheumatol 20:735
Huppertz HI, Tschammler A, Horwitz AE, Schwab KO (1995) Intra-articular corticosteroids for chronic arthritis in children. Efficacy and effect on cartilage and growth. J Pediatr 127:317–321
Karsh J, Yang WH (2003) An anaphylactic reaction to intra-articular triamcinolone: a case report and review of the literature. Ann Allergy Asthma Immunol 90:254–258
Mace S, Vadas P, Pruzanski W (1997) Anaphylactic shock induced by intraarticular injection of methylprednisolone acetate. J Rheumatol 24:1191–1194
Larsson G (1989) Anaphylactis shock after i.a. administration of triamcinolone acetonide in a 35-year-old female. Scand J Rheumatol 18:441–442
Mondal LK, Sarkar K, Datta H, Chatterjee PR (2005) Acute bilateral central serous chorioretinopathy following intra-articuar injection of corticosteroid. Indian J Ophthalmol 53:132–134
Baloch N (1974) Steroid psychosis: a case report. Br J Psychiatry 124:545–546
Robinson DE, Harrison-Hansley E, Spencer RF (2000) Steroid psychosis after an intra-articular injection. Ann Rheum Dis 59:927
Courtman NH, Weighill FJ (1992) Systemic tuberculosis in association with intra-articular steroid therapy. J R Coll Surg Edinb 37:425
Gutierrez-Urena S, Ramus-Remus C (1999) Persistent hiccups associated with intraarticular corticosteroid injection. J Rheum 26:760
Edelman J, Potter JM, Hacket LP (1986) The effect of intraarticular steroids on plasma salicylate concentrations. Br J Clin Pharmacol 21:301–307
Disclosures
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Habib, G.S. Systemic effects of intra-articular corticosteroids. Clin Rheumatol 28, 749–756 (2009). https://doi.org/10.1007/s10067-009-1135-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-009-1135-x