Abstract
The objective of the study was to review the association between fibromyalgia (FM) and sexual dysfunction in women and possible mechanisms of such association. PubMed, MEDLINE, and EMBASE databases (1950–2008) were searched for the key words “fibromyalgia”, “chronic pain”, “sexual dysfunction”, “female”, “sexuality”, “depression”, and “quality of life”. All relevant articles in English and secondary references were reviewed. All reviewed studies showed that FM is associated with sexual dysfunction in women. The major findings were as follows: decreased sexual desire and arousal, decreased experience of orgasm, and increased pain with intercourse. FM, sexual dysfunction, and depression may be interrelated with the depressive mood responsible for desire and arousal problems. On the other hand, in FM patients, the threshold at which sensory input becomes painful is lower than normal that can explain pain on intercourse. Additional studies are needed to evaluate the casual relationship and mechanism of association between FM and sexual dysfunction in women.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fibromyalgia (FM) is one of the most common chronic musculoskeletal pain disorders. FM is defined by the American College of Rheumatology as chronic (≥3 months) widespread pain and pain on palpation of at least 11 of 18 tender point sites throughout the body [1]. In addition to pain and tenderness, patients with FM also report other symptoms, including sleep disruption, fatigue, depression, anxiety, memory and concentration problems, headaches, numbness/tingling, and others [1]. FM may cause functional disability and have a significantly negative effect on quality of life [2]. It disproportionately affects women, with a prevalence of 3.4% in women, compared with 0.5% in men [3]. Prevalence of FM rises steadily with age from <1% in women aged 18–30 to almost 8% in women aged 55–64 [4].
Recently, several studies reported association between FM and sexual dysfunction in women [5–12]. Understanding this association is of importance for development of prevention and treatment strategies both for sexual dysfunction and FM and can also assist in the determination of future research goals.
In the following review, we shall attempt to describe what is currently known about the association between FM and sexual dysfunction in women, and attention will be directed toward possible mechanisms of such association.
Materials and methods
PubMed, MEDLINE, EMBASE, and Google scholar databases (up to December 2008) were searched for the key words “fibromyalgia”, “chronic pain”, “sexual dysfunction”, “female”, “sexuality”, “depression”, and “quality of life”. All relevant articles in English were reviewed. Pertinent secondary references were also retrieved. We critically analyzed all published material. We are aware that this traditional approach to narrative reviews has much more potential for bias than systematic reviews or meta-analyses; however, we have endeavored to be inclusive and open-minded. We also consulted experts in rheumatology and sexology to produce a narrative review on association between FM and sexual dysfunction.
Results
In the last several years, numerous studies were published that found association between FM and sexual dysfunction (Table 1). De Costa et al. [12] performed the first study that evaluated sexual satisfaction of FM patients. In this study, 20 women with FM were compared to 20 healthy women using Beck depression inventory and sexual experience questionnaire. Women with FM showed significantly greater modification in sexual activities (p = 0.01), greater difficulty in having orgasm (p = 0.01), and were more likely to masturbate (p = 0.053). However, this study had significant methodological problems: The sample size was small, age of women in FM group was significantly higher that controls, and sexual experience questionnaire was not validated.
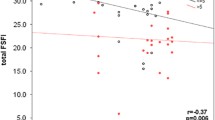
Later, Tikiz et al. [5] in observational study of 40 female subjects with FM, 27 with FM and major depression, and 33 healthy controls found that the Female Sexual Function Index (FSFI) [13] was significantly decreased in the FM and FM plus major depression groups compared with that in healthy controls 21.83 ± 5.84 and 22.43 ± 7.00 vs. 28.10 ± 6.52, respectively (p = 0.001). Women with FM and FM with major depression had significantly lower values of all FSFI parameters: desire, arousal, lubrication, orgasm, satisfaction, and more frequently experienced pain during or after vaginal penetration in comparison with healthy controls. However, it was not significantly different between patients with FM only and FM plus major depression. The authors concluded that female patients with FM have distinct sexual dysfunction compared with healthy controls, and coexistent major depression has no additional negative effect on sexual function.
Shaver and colleagues [11] performed telephone survey of 442 women with and 205 women without FM to assess their health status. Sexual function items were framed in terms of whether health has contributed to any changes and were rated as no change or increase or decrease for ten sexuality items, including desire, fantasies, arousal, vaginal dryness, vaginal tightness, pain, orgasm, masturbation, sexual activity, and satisfaction. After controlling for age, body mass index, race, employment status, marital status, having a college degree, low household income, and having ever been diagnosed with depression, they found that women with FM had significantly more negative changes in sexual function than women without FM. More specifically, women with FM showed significantly decreased sexual arousal and excitement (OR, 2.01), decreased experience of orgasm (OR, 2.22), decreased self-pleasuring/masturbation (OR, 1.91), increased vaginal tightness during penetration (OR, 2.25), and increased pain with intercourse (OR, 2.49; all p < 0.005). On the other hand, women with FM did not show decline of sexual desire compared with healthy controls.
In a smaller survey of 60 women with FM (without control group) performed by Ryan et al. [10], authors found that symptoms associated with FM affected ability “to make love” in 78% of women, and 71% of responders mentioned that FM had put a strain on their sexual relationship with their partner.
Prins et al. [9] examined sexual functioning of 63 women with FM (age, 21–54 years) by Sexual Dysfunctions-Short Form questionnaire. They found that women with FM reported more problems with sexual desire and satisfaction (Mann–Whitney Z = −3.36, p ≤ 0.001) and more pain in their body before, during, or after having sex (Z = 8.54, p ≤ 0.001). Women with FM also reported less frequent sex with partner (Z = −2.09, p < 0.05) and lower frequency of sexual satisfaction (Z = −2.06, p < 0.05). Mental distress, but not pain, was a significant predictor of virtually all aspects of sexual dysfunction. Concluding this data, authors proposed the hypotheses that the psychological but not the physiological aspect of the sexual response cycle is disturbed in FM.
In addition, same group [7] examined the predictive potential of relationship variables on sexual functioning in women with FM. They found that low relationship satisfaction was the strongest and most frequent predictor of problematic sexual functioning. More fatigue and, only after taking account of relationship satisfaction, more active involvement of the spouse were associated with reduced sexual functioning and satisfaction. Results of this study suggested that for women with FM, relationship satisfaction is good for sexual functioning. Although having an involved spouse is good for the relationship, it may be bad for sexual functioning.
Discussion
Despite differences in studied populations, design, and quality, all reviewed studies showed that FM is associated with sexual dysfunction in women. The major findings were decreased sexual arousal and excitement [5, 9, 11, 12], decreased experience of orgasm [5, 9, 11, 12], and increased pain with intercourse [5, 11].
Two major hypotheses were proposed to explain the association between sexual dysfunction and FM in women. Prins and colleagues [9] argued that in women with FM, the psychological but not the physiological aspect of the sexual response cycle is disturbed. On the other hand, Tikiz and colleagues [5] suggested that FM is directly, not though psychological pathway, associated with sexual dysfunction, and depression just coexists with FM, but has neutral effect on sexual function.
Depression and anxiety have been cited as possible factors leading to poor sexual functioning in people with chronic pain [14, 15]. In a recent study of Orellana et al. [8], sexual function was assessed by Changes in Sexual Functioning Questionnaire and was compared between 31 women with FM, 20 age-matched healthy women, and 26 women with rheumatoid arthritis. FM and rheumatoid arthritis patients showed a significantly higher rate of sexual dysfunction compared to healthy controls. Sexual dysfunction was more frequent among FM patients (97%) than in rheumatoid arthritis patients (84%) but without statistical differences. Among other studied covariates, only the intensity of depression was associated with the sexual dysfunction in patients with FM in the multivariate analysis. Circumferential support for the hypothesis that depression is responsible for sexual dysfunction of FM patients can be found in the fact that women with a history sexual abuse or other traumatic events in childhood reported more chronic pain symptoms and utilized more health care resources compared to non-abused control subjects [16, 17]. Alexander et al. [18] described that 57% of FM patients reported a history of sexual/physical abuse. In a study of patients from a specialized clinic in rheumatic diseases in Guatemala City [19], 70.7% of patients with FM reported abuse, 24.3% verbal, 60.9% physical, and 14.8% sexual. On the other hand, as we mentioned before, the study of Tikiz et al. [5] found that major depression has no additional effect on sexual function of women with FM. Depression and FM often coincide and share common symptoms [20], and it is possible that each of this condition has a separate pathway of association with sexual dysfunction.
There were studies that reported significant comorbidity between vulvodynia that usually severely impacts sex life and FM [21, 22]. Gordon et al. [22] reported that vulvar pain disorders were observed in approximately 20.6% of women with FM and 16.8% of women with chronic depression in a web-based study. As well, Aydin et al. [6] found that complaints of pain during sexual intercourse were more common in FM patients (50%) than in our healthy controls (16.7%). Shaver et al. [11], who found significant association between FM and increased pain and vaginal tightness with intercourse, proposed the following explanation for association between FM and sexual dysfunction: In FM patients, the threshold at which sensory input (e.g., touch pressure) becomes painful is lower than normal, and pain tolerance is low [23], so pain on intercourse is likely.
All aforementioned studies were cross-sectional and cannot establish the casual relationship between sexual dysfunction and FM in women. We believe that FM could influence sexual dysfunction in women via both psychological (depression, anxiety, fatigue etc.) and physiological (low pain tolerance, vulvodynia, pain in body before, during or after having sex, etc.) pathways (Fig. 1). Moreover, these physiological (pain) and psychological (depression) factors are interrelated [24]. Another possible pathway is that sexual dysfunction (dissatisfaction) can lead to psychological (and even physiological) stress in women and, this way, to facilitate development of FM. However, no studies evaluated this sequence of events in a longitudinal study. Further longitudinal studies are essential to establish the casual relationship and mechanism of association between FM and sexual dysfunction.
Conclusions
Sexual dysfunction, particularly sexual desire and arousal problems, appear to be common in female patients with FM. Therefore, FM, sexual dysfunction, and depression/anxiety may be interrelated, with the depressive mood and anxiety responsible for desire and arousal problems in those patients. However, it is difficult to explain the exact mechanism of this relation. Additional studies are needed to evaluate the casual relationship and mechanism of association between FM and sexual dysfunction in premenopausal women.
Physicians dealing with FM in their daily practice should be aware of possibility of sexual dysfunction in female patients. Sexual anamnesis has to be a routine part of evaluation of female FM patients. In light of aforementioned studies, we believe that sexology intervention has to be a part of complex treatment of FM in women.
References
Wolfe F, Smythe HA, Yunus MB, Bennett RM, Bombardier C, Goldenberg DL, Tugwell P, Campbell SM, Abeles M, Clark P et al (1990) The American College of Rheumatology 1990 criteria for the classification of fibromyalgia. Report of the Multicenter Criteria Committee. Arthritis Rheum 33:160–172
Wolfe F, Anderson J, Harkness D, Bennett RM, Caro XJ, Goldenberg DL, Russell IJ, Yunus MB (1997) Work and disability status of persons with fibromyalgia. J Rheumatol 24:1171–1178
Wolfe F, Ross K, Anderson J, Russell IJ, Hebert L (1995) The prevalence and characteristics of fibromyalgia in the general population. Arthritis Rheum 38:19–28
White KP, Speechley M, Harth M, Ostbye T (1999) The London Fibromyalgia Epidemiology Study: comparing the demographic and clinical characteristics in 100 random community cases of fibromyalgia versus controls. J Rheumatol 26:1577–1585
Tikiz C, Muezzinoglu T, Pirildar T, Taskn EO, Frat A, Tuzun C (2005) Sexual dysfunction in female subjects with fibromyalgia. J Urol 174:620–623
Aydin G, Basar MM, Keles I, Ergun G, Orkun S, Batislam E (2006) Relationship between sexual dysfunction and psychiatric status in premenopausal women with fibromyalgia. Urology 67:156–161
Kool MB, Woertman L, Prins MA, Van Middendorp H, Geenen R (2006) Low relationship satisfaction and high partner involvement predict sexual problems of women with fibromyalgia. J Sex Marital Ther 32:409–423
Orellana C, Casado E, Masip M, Galisteo C, Gratacos J, Larrosa M (2008) Sexual dysfunction in fibromyalgia patients. Clin Exp Rheumatol 26:663–666
Prins MA, Woertman L, Kool MB, Geenen R (2006) Sexual functioning of women with fibromyalgia. Clin Exp Rheumatol 24:555–561
Ryan S, Hill J, Thwaites C, Dawes P (2008) Assessing the effect of fibromyalgia on patients’ sexual activity. Nurs Stand 23:35–41
Shaver JL, Wilbur J, Robinson FP, Wang E, Buntin MS (2006) Women’s health issues with fibromyalgia syndrome. J Womens Health (Larchmt) 15:1035–1045
De Costa ED, Kneubil MC, Leao WC, The KB (2004) Assessment of sexual satisfaction in fibromyalgia patients. Einstein 2:177–181
Rosen R, Brown C, Heiman J, Leiblum S, Meston C, Shabsigh R, Ferguson D, D’Agostino R Jr (2000) The Female Sexual Function Index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther 26:191–208
Monga TN, Tan G, Ostermann HJ, Monga U, Grabois M (1998) Sexuality and sexual adjustment of patients with chronic pain. Disabil Rehabil 20:317–329
Ambler N, Williams AC, Hill P, Gunary R, Cratchley G (2001) Sexual difficulties of chronic pain patients. Clin J Pain 17:138–145
Finestone HM, Stenn P, Davies F, Stalker C, Fry R, Koumanis J (2000) Chronic pain and health care utilization in women with a history of childhood sexual abuse. Child Abuse Negl 24:547–556
Goldberg RT, Pachas WN, Keith D (1999) Relationship between traumatic events in childhood and chronic pain. Disabil Rehabil 21:23–30
Alexander RW, Bradley LA, Alarcon GS, Triana-Alexander M, Aaron LA, Alberts KR, Martin MY, Stewart KE (1998) Sexual and physical abuse in women with fibromyalgia: association with outpatient health care utilization and pain medication usage. Arthritis Care Res 11:102–115
Castro I, Barrantes F, Tuna M, Cabrera G, Garcia C, Recinos M, Espinoza LR, Garcia-Kutzbach A (2005) Prevalence of abuse in fibromyalgia and other rheumatic disorders at a specialized clinic in rheumatic diseases in Guatemala City. J Clin Rheumatol 11:140–145
Hudson JI, Goldenberg DL, Pope HG Jr., Keck PE Jr., Schlesinger L (1992) Comorbidity of fibromyalgia with medical and psychiatric disorders. Am J Med 92:363–367
Arnold LD, Bachmann GA, Rosen R, Kelly S, Rhoads GG (2006) Vulvodynia: characteristics and associations with comorbidities and quality of life. Obstet Gynecol 107:617–624
Gordon AS, Panahian-Jand M, McComb F, Melegari C, Sharp S (2003) Characteristics of women with vulvar pain disorders: responses to a Web-based survey. J Sex Marital Ther 29(Suppl 1):45–58
Bendtsen L, Norregaard J, Jensen R, Olesen J (1997) Evidence of qualitatively altered nociception in patients with fibromyalgia. Arthritis Rheum 40:98–102
Stahl S, Briley M (2004) Understanding pain in depression. Hum Psychopharmacol 19(Suppl 1):S9–S13
Disclosures
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kalichman, L. Association between fibromyalgia and sexual dysfunction in women. Clin Rheumatol 28, 365–369 (2009). https://doi.org/10.1007/s10067-009-1093-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-009-1093-3