Abstract
Chronic whiplash-associated disorders (WAD) remains a challenging condition for clinicians. There is substantial evidence for the presence of various cervical dysfunctions (e.g., increased cervical muscle tone and impaired cervical movement control), but their contribution to the complex clinical picture of subjects with chronic WAD seems rather limited. There is consistent evidence for increased responsiveness of the central nervous system in those with chronic WAD, and central pain processing is likely to play a crucial role in the transition from an acute whiplash trauma towards chronic WAD. The manuscript explains how our current understanding of chronic WAD can be used to steer the content of conservative interventions and how treatment of cervical dysfunctions in patients with chronic WAD should account for the processes involved in chronicity. It is recommended to prevent sensorimotor incongruence, target cognitive–emotional sensitization, and apply a cognitive behavioral therapy-guided exercise program.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic whiplash-associated disorders (WAD) is a debilitating and costly condition of at least 6-month duration and is characterized by multiple symptoms such as chronic neck pain, fatigue, dizziness, concentration difficulties, and headaches [1]. WAD are diagnosed and categorized according to the Quebec Task Force on WAD [2]. The majority of people recover within the first 3 months after a whiplash injury [3]. However, beyond this point, there is little, if any, improvement [2]. Chronic pain and pain-related disability develops in 15% to 20% of people with whiplash injuries [2, 4, 5].
Chronic WAD remains a challenging condition for clinicians, including rehabilitation specialists and physiotherapists. When assessing patients with chronic WAD, a number of cervical dysfunctions such as increased cervical muscle tone [6] and impaired cervical movement control [7–10] are likely to be revealed. Every clinician familiar with treatment of chronic WAD is aware of the difficulties to actually improve/treat these cervical dysfunctions appropriately. Moreover, when these cervical dysfunctions improve, this does not necessary result in an improvement of the patient’s health status.
During the past decade, scientific research has provided new insights into the development of chronic WAD after a whiplash trauma. Understanding the chronification process might enable rehabilitation specialists to develop a therapeutic rationale, aiming on the one hand at the prevention of chronicity and on the other hand at the treatment of chronic WAD.
The present manuscript intends to provide such a theoretical rationale. In the first part, an overview of the most prominent cervical dysfunctions in patients with WAD is presented. Its clinical importance will be discussed. In the second part, the transition from an acute whiplash trauma towards chronic WAD is explained and applied to clinical practice. This is to explore that rehabilitation should account for the process involved in chronicity of WAD. The manuscript explains how our current understanding of chronic WAD can be used to steer the content of conservative interventions for people with chronic WAD and how treatment of cervical dysfunctions in patients with chronic WAD should account for the processes involved in chronicity.
Chronic WAD: the contribution of cervical dysfunctions
During a whiplash trauma, the head is thrown backwards, forwards, or laterally, resulting in sudden high-velocity hyperextension, hyperflexion, or lateroflexion of the cervical spine (acceleration/deceleration trauma). In WAD grades I to III, fractures or dislocations of the cervical spine cannot be demonstrated. Various studies used magnetic resonance imaging to search for cervical anatomical dysfunctions or injuries. In general, very few lesions have been identified, and even when present they were neither related to symptomatology nor of prognostic value [11, 12]. In chronic WAD, there is no clinical evidence from computerized tomography or magnetic resonance imaging findings [13]. The lack of objective signs of injury calls for the assessment of cervical dysfunctions such as joint mobility, functional stability, cervical proprioception, and increased muscle tone.
Reduced neck mobility is a key clinical finding in patients who experienced a whiplash trauma [2]. From a 6-month prospective study, it was concluded that neck mobility is severely reduced immediately after, but not 3 months after, a whiplash trauma [14]. Due to the correlation with neck pain and headache [14] and because restricted neck mobility immediately after the whiplash trauma is a negative prognostic factor, cervical mobility appears to be of clinical significance in the early stages of whiplash rehabilitation. Besides these observations in (sub)acute WAD cases, a whiplash injury in general does not give rise to persistent restriction of cervical mobility [14]. Thus, reduced neck mobility is not a characteristic of chronic WAD and is unable to explain the complexity of the syndrome.
Patients with chronic WAD frequently present impaired sensorimotor control. For instance, impaired cervical proprioception has been demonstrated in patients with WAD, especially in those reporting dizziness [15–19]. However, impaired cervicocephalic kinesthetic sensibility is unrelated to pain severity [17], questioning the clinical importance of this finding. Cervical treatments and proprioceptive exercises have been shown to be effective in improving proprioceptive function and reducing the neck complaints of patients with insidious neck pain [20–22], but studies in chronic WAD are lacking.
In addition, impaired motor control of the cervical region is documented in those with WAD [7–10]. Reduced conjunct motion during cervical spine movement appears characteristic of persistent WAD and provides evidence for an altered motor control [7]. This is also illustrated via the craniocervical flexion test. During this test, subjects are positioned in supine lying and asked to perform a gentle nodding of the head. This test has been shown to activate the deep cervical flexors, such as the longus colli and capitis [6, 7]. In contrast with the larger superficial cervical muscles, such as the sternocleidomastoid muscle, the deep cervical flexors are not meant to mobilize the spine but have a stabilizing role. By stabilizing the cervical spine, they have a protective function in anticipation of and during the execution of movement tasks. In subjects without neck pain, their anticipatory contraction is a result of a feedforward mechanism orchestrated by the medullary reticular formation. During the craniocervical flexion test, patients with WAD activate their superficial flexors rather than their deep flexors [10]. This is assumed to be a compensation strategy for poor segmental stability of the cervical spine [10]. Also, altered muscle activation patterns of the upper trapezius muscle have been observed in those with WAD [23].
The abovementioned cervical dysfunctions (i.e., altered cervical muscle activation patterns and reduced conjunct motion during cervical spine movement) appear to be nonspecific for whiplash patients: identical changes appear in subjects having insidious onset neck pain [10] or chronic nonspecific neck pain [7, 23]. Importantly, these cervical dysfunctions are of limited prognostic value in the transition from acute whiplash trauma towards chronic WAD [8, 9]. Thus, these physical dysfunctions are not the reason why the treatment of people with chronic WAD can be more challenging than the treatment of patients with chronic insidious neck pain [10].
The reduced cervical mobility and impaired cervicocephalic kinesthetic sensibility are each closely related to oculomotor dysfunction in patients with WAD [16, 24]. Two ocular stabilization reflexes (i.e., the cervico-ocular reflex and the vestibulo-ocular reflex) do not adapt appropriately and lack synergy in patients with WAD, possibly explaining WAD symptoms like vertigo, dizziness, and visual disturbances like blurring of the visual image [24]. Although compelling, the clinical importance of these findings remains to be established.
Finally, the majority of people with WAD present positive trigger points on manual palpation of cervical region: 85% in the semispinalis capitis and the trapezius, 77% in the levator scapulae, 64% in the scalenus medius, 51% in the sternocleidomastoideus, and 21% in the masseter muscle [6]. As is the case with impaired motor control of the cervical spine, these trigger points appear nonspecific to whiplash patients. Only the prevalence of trigger points in the semispinalis capitis muscles is significantly higher in patients with WAD compared to those with fibromyalgia and chronic neck pain [6]. In those with WAD, trigger points appear more often in the upper part of the cervical spine, while in patients with chronic insidious onset neck pain and fibromyalgia they appear predominantly in the lower cervical spine and shoulder girdle [6].
In conclusion, various cervical dysfunctions (listed in Table 1) are documented in patients with chronic WAD. However, they appear to be nonspecific to WAD cases and their prognostic value seems limited. Cervical dysfunctions only partially explain the complex clinical picture of subjects with chronic WAD. It is recommended that clinicians keep in mind the potential cervical dysfunctions frequently seen in chronic WAD sufferers and decide on an individual basis whether they should be targeted during rehabilitation. The treatment of cervical dysfunctions in patients with chronic WAD is explained in the therapeutic implication sections below.
Chronic WAD: the contribution of abnormal sensory processing in the central nervous system
Peripheral sensitization in response to a whiplash trauma
If local (cervical) dysfunctions are unable to fully explain the complex clinical picture of chronic WAD, then what is? For a better understanding of chronic WAD, we have to take a closer look at the neurophysiology of pain. Not all nociceptive signals are perceived as pain, and not every pain sensation originates from nociception. Nevertheless, acute pain sensations, like those experienced in the days following a whiplash trauma, almost always originate from nociceptors in somatic tissue(s). When tissue is damaged after a whiplash trauma, the responsiveness of nociceptive endings is enhanced by various substances released by various sources (e.g., serotonin released by platelets, bradykinin from the plasma, prostaglandins released by damaged cells, substance P released by the primary afferent fibers) [25, 26]. This process is called peripheral sensitization of nociceptors and is no more than a protective action of the human body to prevent use and consequent further damage of the traumatized and surrounding tissues. Once stimulated, nociceptors send impulses via either fast conducting A-delta pain fibers (resulting in a sharp first pain) or slow (unmyelinated) C fibers (resulting in a duller longer-lasting pain or second pain) towards lamina I, II, and V of the dorsal horn of the spinal cord, where A-delta and C fibers synapse with spinal neurons via synaptic transmission [25].
Temporal summation of second pain
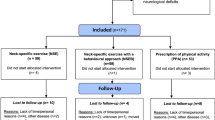
In case of a whiplash trauma with a nonspontaneous recovery, the nociceptors keep on “firing” nociceptive impulses towards the central nervous system (Fig. 1) and the dorsal horn neurons are likely to become hypersensitive [27, 28]. This increased neuronal responsiveness is accomplished by neurotransmitters like glutamate, aspartate, and substance P, which modulate the postsynaptic electric discharges with further transmission to supraspinal sites (thalamus, anterior cingulate cortex, insular cortex, and somatosensory cortex) via ascending pathways [27]. The neurotransmitters initiate increased postsynaptic responses by triggering hyperexcitability of N-methyl-d-aspartate receptor sites of second-order neurons in the dorsal horn. This mechanism is related to temporal summation of second pain or windup. Windup refers to the progressive increase of electrical discharges from the second-order neuron in the spinal cord in response to repetitive C-fiber stimulation and is experienced in humans as increased pain [29–31]. Windup is part of the process known as central sensitization [32]. When rehabilitation specialists/physiotherapists apply hands-on techniques to people with WAD and by doing so eliciting identical nociceptive stimuli to the skin, muscles, or joint capsules more often than once every 3 seconds, they are likely to trigger this mechanism of pain amplification [33].
Central sensitization
Central sensitization is defined as “an augmentation of responsiveness of central pain-signaling neurons to input from low-threshold mechanoreceptors” [34]. There is consistent evidence for altered central pain processing and central sensitization in people with chronic WAD [8, 9, 35–37]. While peripheral sensitization is a local phenomenon, central sensitization means that central pain processing pathways localized in the spinal cord and the brain sensitize. Indeed, the process of central sensitization is neither limited to the dorsal horn nor to pain amplification of afferent impulses. Central sensitization encompasses altered sensory processing in the brain and malfunctioning of descending pain-inhibitory mechanisms. Coding of the mechanism of windup involves multiple brain sites, including somatosensory (thalamus, anterior insula, posterior insula, primary somatic sensory cortex, secondary somatic sensory cortex), cognitive–evaluative/affective (anterior cingulate cortex and prefrontal cortex), and pain-modulating regions (rostral anterior cingulate cortex) [31]. In the resting state, patients with chronic WAD display an increased regional cerebral blood flow in the medial frontal gyrus, somatosensory cortex, posterior cingulate gyrus, and the parahippocampal gyrus [38].
Activation of certain regions of the midbrain activates extremely powerful descending pain-modulating pathways that project, via the medulla, to neurons in the dorsal horn that control the ascending information in the nociceptive system [25]. These pain-inhibitory pathways arise mainly from the periaqueductal gray matter and the rostral ventral medulla in the brainstem [25]. One function of the descending inhibitory pathway is to “focus” the excitation of the dorsal horn neurons by suppressing surrounding neuronal activity [39], a role attributed to the “diffuse noxious inhibitory controls” phenomenon [40]. In case of chronic WAD, these descending pain-inhibitory pathways are malfunctioning [41].
Long-term potentiation
Further to the brain processes involved in central sensitization (Fig. 1), neuronal synapses in the anterior cingulate cortex undergo long-term plastic changes like presynaptic enhancement of glutamate release, postsynaptic enhancement of glutamate-receptor-mediated responses, and recruitment of previously “silent” synapses [42]. These mechanisms all contribute to long-term potentiation of synaptic responses in the anterior cingulated cortex, which is one of the processes involved in the overall concept of central sensitization [42]. The anterior cingulate cortex is involved in acute pain experiences, empathy of pain, social exclusion, chronic pain, and hypothesized pain (reviewed in [42]). In addition, due to the interconnections of anterior cingulate cortex neurons with neurons in the amygdale, long-term potentiation in the anterior cingulate cortex is likely to be involved in psychosocial dimensions of chronic pain like emotional fear, anxiety, and depression [42].
Altered sensory processing has prognostic value for whiplash
Fifteen percent to 20% of people with whiplash injuries develop chronic pain and disability [2–5]. An important and ongoing source of pain is required before the process of peripheral sensitization can establish central sensitization. The use of anesthetic injections identified cervical intervertebral disks and cervical zygapophyseal joints as potential peripheral pain generators in patients with WAD (reviewed in [43]). It seems crucial to limit the time course of afferent stimulation of peripheral nociceptors in people with (sub)acute WAD: tissue injury healing and focal pain recovery should occur within a period of approximately 3 months to prevent development of chronic pain [44]. This notion is supported by a study showing that the presence of a pain condition prior to the whiplash trauma increases the probability for developing chronic WAD [45]. Consequently, appropriate and effective rehabilitation in those with (sub)acute WAD is important to prevent evolvement from an acute whiplash to a chronic pain syndrome, characterized by chronic pain and even symptoms of central sensitization outside the musculoskeletal system like increased sensitivity to bright lights, auditory loudness, odors, and other sensory stimuli. Altered central pain processing rather than impaired motor control has been identified as one of the prime prognostic factors for developing chronic whiplash [8, 9, 46]. From these studies, we know that abnormal sensory processing appears very soon (<7 days) after the initial whiplash trauma, and once present it has important predictive ability for chronicity.
The presence of abnormal sensory processing in those with chronic WAD is likely to have major consequences for the rehabilitation of these patients. Data suggesting that the presence of sensory hypersensitivity influences outcomes in physical rehabilitation for chronic WAD patients are available [47]. Those chronic WAD subjects having both widespread mechanical and cold hyperalgesia showed least improvement. Understanding the processes involved in the development and sustainment of chronic WAD is one thing, but how can we manage the process of central sensitization in chronic WAD patients in daily practice? How should we adapt our current rehabilitation strategies for chronic WAD sufferers to account for the processes involved in central sensitization? In the next section, we explain the different therapeutic implications of the presence of central sensitization in people with WAD.
Therapeutic implications part I: muscle techniques
Abnormal central pain processing has implications for the management of pain spots (myogeloses, taut bands, and myofascial tender/trigger points) in those with chronic WAD. As outlined above, the majority of people with WAD present positive trigger points on manual palpation [6]. Painful and tender points are probably areas of referred pain in most whiplash patients, but it is now generally accepted that anesthetizing these tender points is unlikely to produce complete pain relief [37]. Still, if muscles and fascia become hypertonic and develop trigger points in people with chronic WAD, then soft tissue mobilizations are required to release restrictions and restore local blood flow. If not, they are likely to serve as a new source of nociceptive barrage to the central nervous system, thus sustaining the process of central sensitization [48]. Indeed, experimental data suggest that central hypersensitivity in chronic WAD patients is a dynamic process that is modulated continuously by changes in nociceptive input from the periphery [37].
However, it is important not to increase pain during the treatment of trigger points. The vicinity of myofascial trigger points differs from normal muscle tissue by its lower pH levels (i.e., more acid), increased levels of substance P, calcitonin gene-related peptide, tumor necrosis factor α, and interleukin 1β, each of which has its role in increasing pain sensitivity [49]. Sensitized muscle nociceptors are more easily activated and may respond to normally innocuous and weak stimuli such as light pressure and muscle movement [49].
Therefore, starting the soft tissue mobilization superficially with well-tolerated strokes along the length of the muscle fibers (referred to as “stripping” [50]) and progressing towards deeper strokes that go perpendicular to the soft tissue fibers is recommended. Aggressive ways of treating trigger points (e.g., by using ischemic pressure) are usually not well tolerated and therefore not recommended. When applying these hands-on therapies, one should always remember that any therapeutic intervention triggering more pain will serve as a new peripheral source of nociceptive barrage and thus will sustain the process of central sensitization [33]. It should be noted that there is currently no evidence supporting the use of muscle techniques in those with chronic WAD.
Therapeutic implications part II: prevent sensorimotor incongruence
As explained in the first part of the manuscript, there are indications of impaired sensorimotor control in subjects with chronic WAD. Rehabilitation aiming at improving motor control in the cervical region is likely to have its place in the prevention of chronicity in (sub)acute whiplash cases and in the treatment of chronic WAD. Indeed, a sustained mismatch between motor activity and sensory feedback is able to serve as an ongoing source of nociception inside the central nervous system. There is evidence that a mismatch between motor activity and sensory feedback can elicit pain and sensory perceptions in healthy pain-free volunteers [51] and exacerbates pain and sensory perceptions in patients with chronic pain [52], suggesting a possible etiological role for sensorimotor incongruence in the development of (chronic) pain.
The role of the motor control system in the brain is to manage the relationship between motor commands and sensory feedback (proprioception, vision, and equilibrium). In case of inaccurate execution of cervical movements as repeatedly observed in patients with chronic WAD [7–10, 15–17], an incongruence between motor command and sensory feedback is likely to occur. The motor control system may alert the whiplash patient to the abnormality in information processing by generating warning signals (i.e., pain or other sensory changes like temperature change or a feeling of peculiarity).
Thus, if present, it seems plausible to treat impaired cervical movement control in people with chronic WAD. Again, caution is required not to induce or aggravate pain and other symptoms during treatment. Physical rehabilitation may aggravate symptoms in some patients with chronic WAD [47], as evidenced by a study showing up to 20% side effects in response to an individualized, progressive, submaximal exercise program or a self-management program consisting of advice and exercise [53]. Therefore, the use of low-load exercises and low-velocity mobilizing techniques is recommended for patients with WAD [47] and appears to be in-line with our reasoning in relation to altered sensory processing in chronic WAD. When using specific stabilization exercises to re-educate muscle control in the cervical and scapular region or when using cervical mobilizing techniques in the treatment of chronic WAD patients, it is recommended to stay below the pain threshold.
Ergonomic advice on daily activities frequently encountered by the patient might limit nociceptive barrage as well. In patients with chronic WAD, a multimodal physiotherapy program consisting of specific stabilization exercises, low-velocity mobilizing techniques, and ergonomic advice was proven to be superior over a self-management program (moderate effect size of 0.48) [47]. Other kinds of conservative treatments like pain physiology education are likely to have their place in the prevention and treatment of chronic WAD and will be explained below.
Therapeutic implications part III: target cognitive–emotional sensitization
Catastrophic beliefs about pain (i.e., helplessness, rumination, and magnification) are associated with heightened pain and disability in people with chronic WAD [54], and they play an important role in the transition from (sub)acute to chronic WAD [54, 55]. Besides catastrophizing, other psychological factors such as depression [3, 56], anxiety [3], expectations for recovery [57], and high psychological distress [45] have been identified as important prognostic factors for WAD patients. Coping strategies such as diverting attention and increasing activity are related with positive outcome [55]. Although the dysfunctional descending pain-inhibitory mechanism as seen in those with chronic WAD is primary biological, it is influenced by inappropriate cognitions, emotions, and behavior like catastrophizing, hypervigilance, avoidance behavior, and somatization. In case of more intense pain levels, pain catastrophizing is associated with decreased activity in brain regions involved in top-down pain suppression like the dorsolateral prefrontal cortex and the medial prefrontal cortex [58]. Increased neuronal activity, consistent with pain catastrophizing, has been observed in people with chronic WAD and was correlated with neck disability ratings [38]. In addition to catastrophizing, avoidance behavior and somatization may result in sensitization of dorsal horn spinal cord neurons (through inhibition of descending tracks in the central nervous system) or, alternatively, may be the result of central sensitization [59]. Sustained arousal is likely to maintain sensitization of the neurobiological loops [60].
Thus, in order to achieve a positive rehabilitation outcome for patients with WAD, it seems plausible to use intervention programs that specifically target catastrophic beliefs. One example is the progressive goal attainment program consisting of a 10-week psychosocial intervention program that aims to minimize psychological barriers to rehabilitation progress (including catastrophizing) and includes graded activity [61]. In a nonrandomized controlled clinical trial, this program was found to be effective in improving function and facilitating return to work in subjects with grades I or II WAD [61]. Gradually enhancing physical activity is likely to reduce pain catastrophizing [56]. In-line with our reasoning on central sensitization, physical activity should not exacerbate symptoms. Pain-provoking activities might confirm catastrophic cognitions.
In case of hypervigilance, catastrophizing, or avoidance behavior, intensive education about the exact nature of chronic whiplash pain is likely to facilitate effective rehabilitation. Changing inappropriate pain beliefs should be the initial phase of rehabilitation in those with chronic WAD. If not, poor understanding of pain may lead to the acquisition of maladaptive attitudes, cognitions, and behavior in relation to pain [62] and consequent poor compliance to any active treatment like motor control training and aerobic exercise interventions. In addition, education about the physiology of chronic whiplash pain seems able to improve expectations for recovery, especially in (sub)acute stages of WAD [57]. Pain physiology education was found to be effective in reducing pain catastrophizing in those with chronic low back pain [63, 64]. In patients with chronic WAD, a 4-week program including exercise and extensive education to change pain cognitions and pain-coping strategies resulted in a positive outcome [65].
It seems plausible that improving beliefs like catastrophizing is important not only for enabling proper functioning of the central pain-inhibitory pathways but to improve movement performance as well. In case motor control training appears very difficult in patients with chronic WAD, changing inappropriate beliefs might solve the problem. Indeed, inappropriate cognitions appear closely related to movement performance [66–68]. Healthy subjects display a relation between pain catastrophizing and brain activity in regions involved in motor response and motor planning (i.e., thalamus, putamen, and premotor cortex) [58]. We recently conducted a single case study design in six chronic WAD sufferers and found that intensive education about the physiology of (chronic) pain resulted in improved pain cognitions, cervical pressure pain threshold, and pain-free cervical movement performance (unpublished data—manuscript in progress).
Therapeutic implications part IV: time-contingent or pain-contingent exercise therapy?
Data are available suggesting that the presence of sensory hypersensitivity influences outcome in physical rehabilitation for chronic WAD patients [47]. Those chronic WAD subjects having both widespread mechanical and cold hyperalgesia showed least improvement. For those people with chronic WAD and evidence of central sensitization, using cognitive behavioral therapy principles to implement an individualized, progressive, and submaximal exercise program might not be appropriate.
Cognitive behavioral therapies advocates goal setting in a time-contingent rather than a pain-contingent fashion. On the one hand, this approach diverts attention away from symptoms, and by doing so it decreases hypervigilance to symptoms like pain. On the other hand, a time-contingent approach teaches the patient to ignore pain aggravations. This increases the risk of augmenting nociceptive barrage towards the central nervous system during and following treatment, which in turn is likely to sustain the process of central sensitization. We claim that this might explain the large amount of side effects (up to 20% of the subjects studied) as observed in chronic WAD patients in response to a cognitive behavioral-therapy-guided exercise program [53].
It might be warranted to redefine cognitive behavioral therapy to make it appropriate to chronic WAD. It is suggested to initiate rehabilitation with changing inappropriate cognitions and beliefs as explained above but at the same time explaining that any type of physical activity (including exercise interventions) that increases symptom severity is likely to sustain chronicity. Next, a flexible and gentle way of performing specific (e.g., cervical motor control training) and general (aerobic) exercise or activity interventions where the client is instructed to adopt exercise intensity and duration to stay below pain threshold seems appropriate. This type of rehabilitation can still be classified as a cognitive behavioral-therapy-guided exercise program but is adapted within the framework of central sensitization.
Conclusions
There is substantial evidence for the presence of various cervical dysfunctions in patients with chronic WAD, but their contribution to the complex clinical picture of subjects with chronic WAD seems rather limited. It is recommended that clinicians search for cervical dysfunctions in chronic WAD sufferers and decide on an individual basis whether they should be targeted during rehabilitation. If present, it seems plausible to treat cervical dysfunctions like decreased movement control in people with chronic WAD, but caution is required not to induce or aggravate pain and other symptoms during treatment. Given the consistent evidence for increased responsiveness of the central nervous system in those with chronic WAD, any additional or accelerated source of nociception is likely to sustain or enhance the process of central sensitization. To prevent physical rehabilitation to aggravate symptoms in patients with chronic WAD, muscle techniques, local and general exercise interventions, and psychosocial interventions should account for the processes involved in central sensitization (therapeutic recommendations are summarized in Table 2). However, although the reasoning outlined in the manuscript is based on a strong theoretical rationale (backed up by evidence from the fundamental and clinical sciences), clinical studies examining the effectiveness of the proposed treatment strategies are required.
References
Rodriquez AA, Barr KP, Burns SP (2004) Whiplash: pathophysiology, diagnosis, treatment, and prognosis. Muscle Nerve 29:768–781
Spitzer WO, Skovron ML, Salmi LR, Cassidy JD, Duranceau J, Suissa S, Zeiss E (1995) Scientific monograph of the Quebec task force on whiplash-associated disorders: redefining « whiplash » and its management. Spine 20:S1–S73
Kamper SJ, Rebbeck TJ, Maher CG, McAuley JH, Sterling M (2008) Course and prognostic factors of whiplash: a systematic review and meta-analysis. Pain 138:617–629 doi:10.1016/j.pain.2008.02.019
Radanov BP, Sturzenegger M (1996) The effect of accident mechanism and initial findings on the long-term outcome of whiplash injury. J Musculoskel Pain 4:47–60
Côté P, Hogg-Johnson S, Cassidy JD et al (2001) The association between neck pain intensity, physical functioning, depressive symptomatology and time-to-claim-closure after whiplash. J Clin Epidemiol 54:275–286
Ettlin T, Schuster C, Stoffel R, Brüderlin A, Kischka U (2008) A distinct pattern of myofascial findings in patients after whiplash injury. Arch Phys Med Rehabil 89:1290–1293
Woodhouse A, Vasseljen O (2008) Altered motor control patterns in whiplash and chronic neck pain. BMC Musculoskel Dis 9:90 doi:10.1186/1471-2474-9-90
Sterling M, Jull G, Vicenzino B, Kenardy J (2003) Sensory hypersensitivity occurs soon after whiplash injury and is associated with poor recovery. Pain 104:509–517
Sterling M, Jull G, Kenardy J (2006) Physical and psychological factors maintain long-term predictive capacity post-whiplash injury. Pain 122:102–108
Jull G, Kristjansson E, Dall’Alba P (2004) Impairment in the cervical flexors: a comparison of whiplash and insidious onset neck pain patients. Man Ther 9:89–94
Kongsted A, Sorensen JS, Andersen H, Keseler B, Jensen TS, Bendix T (2008) Are early MRI findings correlated with long-lasting symptoms following whiplash injury? A prospective trial with 1-year follow-up. Eur Spine J 17:996–1005 doi:10.1007/s00586-008-0687-9
Miettinen T, Lindgren KA, Airaksinen O, Leino E (2002) Whiplash injuries in Finland: a prospective 1-year follow-up study. Clin Exp Rheumatol 20:399–402
Hol PK (2008) Imaging in whiplash. Cephalalgia 28(S1):25–27
Kasch H, Stengaard-Pedersen K, Arendt-Nielsen L, Jensen TS (1994) Headache, neck pain, and neck mobility after acute whiplash injury. A prospective study. Spine 26:1246–1251
Louden JK, Ruhl M, Field E (1997) Ability to reproduce head position after whiplash injury. Spine 22:865–868
Heikkilä HV, Wenngren B-I (1998) Cervicocephalic kinesthetic sensibility, active range of cervical motion, and oculomotor function in patients with whiplash injury. Arch Phys Med Rehabil 79:1089–1094
Heikkilä H, Aström P-G (1996) Cervicocephalic kinesthetic sensibility in patients with whiplash injury. Scand J Rehabil Med 28:133–138
Treleaven J, Jull G, Sterling M (2003) Dizziness and unsteadiness following whiplash injury: characteristic features and relationship with cervical joint position error. J Rehabil Med 35:36–43
Treleaven J, Jull G, Lowchoy N (2005) Standing balance in persistent whiplash: a comparison between subjects with and without dizziness. J Rehabil Med 37:224–229
Jull G, Falla D, Treleaven J, Hodges P, Vicenzino B (2007) Retraining cervical joint position sense: the effect of two exercise regimes. J Orthop Res 25:404–412
Palmgren PJ, Sandstrom PJ, Lundqvist FJ, Heikkila H (2006) Improvement after chiropractic care in cervicocephalic kinesthetic sensibility and subjective pain intensity in patients with nontraumatic chronic neck pain. J Manipulative Physiol Ther 29:100–106
Rogers RG (1997) The effect of spinal manipulation on cervical kinesthesia in patients with chronic neck pain: a pilot study. J Manipulative Physiol Ther 20:80–85
Nederhand MJ, Hermens HJ, Ijzerman MJ, Turk DC, Zivold G (2002) Cervical muscle dysfunction in chronic whiplash-associated disorder grade 2: the relevance of the trauma. Spine 27:1056–1061
Montfoort I, Van der Geest JN, Slijper HP, De Zeeuw CI, Frens MA (2008) Adaptation of the cervico- and vestibulo-ocular reflex in whiplash injury patients. J Neurotrauma 25:687–693
Purves D, Augustine GJ, Fitzpatrick D, Katz LC, LaMantia A-S, McNamara JO (1997) Pain. In: Purves D, Augustine GJ, Fitzpatrick D, Katz LC, LaMantia A-S, McNamara JO (eds) Neuroscience. Sinauer, Sunderland, p 167
Ji R-R, Kohno T, Moore KA, Woolf CJ (2003) Central sensitization and LTP: do pain and memory share similar mechanisms. Trends Neurosci 26:696–705
Staud R, Smitherman ML (2002) Peripheral and central sensitization in FM: pathogenic role. Curr Pain Headache Rep 6:259–266
Baranauskas G, Nistri A (1998) Sensitization of pain pathways in the spinal cord: cellular mechanisms. Prog Neurobiol 54:349–365
Mendell LM, Wall PD (1965) Responses of single dorsal cord cells to peripheral cutaneous unmyelinated fibres. Nature 206:97–99
Gracely RH, Geisser ME, Giesecke T, Grant MAB, Petzke F, Williams DA, Clauw DJ (2004) Pain catastrophizing and neural responses to pain among persons with fibromyalgia. Brain 127:835–843
Staud R, Craggs JG, Robinson ME, Perlstein WM, Price DD (2007) Brain activity related to temporal summation of C-fiber evoked pain. Pain 129:130–142
Meeus M, Nijs J (2007) Central sensitization: a biopsychosocial explanation for chronic widespread pain in patients with fibromyalgia and chronic fatigue syndrome. Clin Rheumatol 26:465–473
Nijs J, Van Houdenhove B (2009) From acute musculoskeletal pain to chronic widespread pain and fibromyalgia: Application of pain neurophysiology in manual therapy practice. Manual Therapy 14:3–12 doi:10.1016/j.math.2008.03.001
Meyer RA, Campbell JN, Raja SN (1995) Peripheral neural mechanisms of nociception. In: Wall PD, Melzack R (eds) Textbook of pain. third edn. Churchill Livingstone, Edinburgh, pp 13–44
Sterling M, Treleaven J, Edwards S, Jull G (2002) Pressure pain thresholds in chronic whiplash associated disorder: further evidence of altered central pain processing. J Musculoskel Pain 10:69–81
Curatolo M, Petersen-Felix S, Arendt-Nielsen L, Giani C, Zbinden AM, Radanov BP (2001) Central hypersensitivity in chronic pain after whiplash injury. Clin J Pain 17:306–315
Herren-Gerber R Weiss S, Arendt-Nielsen L, Petersen-Felix S, Di Stefano G, Radanov BP, Curatolo M (2004) Modulation of central hypersensitivity by nociceptive input in chronic pain after whiplash injury. Pain Med 5:366–376
Linnman C, Appel L, Söderlund A, Frans Ö, Engler H, Furmark T, Gordh T, Langström B, Fredrikson M (2008) Chronic whiplash symptoms are related to altered regional cerebral blood flow in the resting state. Eur J Pain doi:10.1016/j.ejpain.2008.03.001
Woolf CJ, Salter MW (2000) Neuronal plasticity: increasing the gain in pain. Science 288:1765–1769
Le Bars D, Villaneuva L (1988) Electrophysiological evidence for the activation of descending inhibitory controls by nociceptive afferent pathways. Prog Brain Res 77:275–299
Banic B, Petersen-Felix S, Andersen OK, Radanov BP, Villiger PM, Arendt-Nielsen L, Curatolo M (2004) Evidence for spinal cord hypersensitivity in chronic pain after whiplash injury and in fibromyalgia. Pain 107:7–15
Zhuo M (2007) A synaptic model for pain: long-term potentiation in the anterior cingulated cortex. Mol Cells 23:259–271
Davis CG (2000) Injury threshold: whiplash-associated disorders. J Manipulative Physiol Ther 23:420–427
Vierck CJ (2006) Mechanisms underlying development of spatial distributed chronic pain (fibromyalgia). Pain 124:242–263
Carstensen TBW, Frostholm L, Oernboel E, Kongsted A, Kasch H, Jensen TS, Fink P (2008) Post-trauma ratings of pre-collision pain and psychological distress predict poor outcome following acute whiplash trauma: a 12-month follow-up study. Pain 139:248–259 doi:10.1016/j.pain.2008.04.008
Kasch H, Querama E, Flemming WB, Jensen TS (2005) Reduced cold pressor pain tolerance in non-recovered whiplash patients: a 1-year prospective study. Eur J Pain 9:561–569
Jull G, Sterling M, Kenardy J, Beller E (2007) Does the presence of sensory hypersensitivity influence outcomes of physical rehabilitation for chronic whiplash? A preliminary RCT. Pain 129:28–34
Dommerholt J (2005) Persistent myalgia following whiplash. Curr Pain Headache Rep 9:326–330
Shah JP, Philips TM, Danoff JV, Gerber LH (2005) An in vivo microanalytical technique for measuring the local biochemical milieu of human skeletal muscle. J Appl Physiol 99:1977–1984
Benjamin PJ, Tappan FM (2005) Tappan’s handbook of healing massage techniques. Classic, holistic, and emerging methods. Pearson Prentice Hall, Englewood Cliffs, p 127
McCabe CS, Haigh RC, Halligan PW, Blake DR (2005) Simulating sensory-motor incongruence in healthy volunteers: implications for a cortical model of pain. Rheumatol 44:509–516
McCabe CS, Cohen H, Blake DR (2007) Somaesthetic disturbances in fibromyalgia are exaggerated by sensory-motor conflict: implications for chronicity of the disease. Rheumatol 46:1587–1592
Stewart MJ, Maher CG, Refshauge KM, Herbert RD, Bogduk N, Nicholas M (2007) Randomized controlled trial of exercise for chronic whiplash-associated disorders. Pain 128:59–68
Berglund A, Bodin L, Jensen I, Wiklund A, Alfredsson L (2006) The influence of prognostic factors on neck pain intensity, disability, anxiety and depression over a 2-year period in subjects with acute whiplash injury. Pain 125:244–256
Söderlund A, Lindberg P (2003) Whiplash-associated disorders—predicting disability from a process-oriented perspective of coping. Clinical Rehabilitation 17:101–107
Börsbo B, Peolsson M, Gerdle B (2008) Catastrophizing, depression, and pain: correlation with and influence on quality of life and health—a study of chronic whiplash-associated disorders. J Rehabil Med 40:562–569
Holm LW, Carroll LJ, Cassidy JD, Skillgate E, Ahlbom A (2008) Expectations for recovery important in the prognosis of whiplash injuries. PLoS Med 5:e105 doi:10.1371/journal.pmed.0050105
Seminowicz DA, Davies KD (2006) Cortical responses to pain in healthy individuals depends on pain catastrophizing. Pain 120:297–306
Zusman M (2002) Forebrain-mediated sensitization of central pain pathways: ‘non-specific’ pain and a new image for MT. Man Ther 7:80–88
Ursin H, Eriksen HR (2001) Sensitization, subjective health complaints, and sustained arousal. Annals N Y Acad Sci 933:119–129
Sullivan MJL, Adams H, Rhodenizer T, Stanish WD (2006) A psychosocial risk factor-targeted intervention for the prevention of chronic pain and disability following whiplash injury. Phys Ther 86:8–18
Geisser ME, Roth RS (1998) Knowledge of and agreement with chronic pain diagnosis: relation to affective distress, pain beliefs and coping, pain intensity and disability. J Occup Rehabil 8:73–88
Moseley GL (2002) Combined physiotherapy and education is efficacious for chronic low back pain. Austr J Physiother 48:297–302
Moseley GL, Nicholas MK, Hodges PW (2004) A randomized controlled trial of intensive neurophysiology education in chronic low back pain. Clin J Pain 20:324–330
Vendrig AA, van Akkerveeken PF, McWhorter KR (2000) Results of a multimodal treatment program for patients with chronic symptoms after a whiplash injury of the neck. Spine 25:238–244
Moseley GL (2005) Widespread brain activity during and abdominal task markedly reduced after pain physiology education: fMRI evaluation of a single patient with chronic low back pain. Austr J Physiother 51:49–52
Nijs J, Van de Putte K, Louckx F, Truijen S, De Meirleir K (2008) Exercise performance and chronic pain in chronic fatigue syndrome: the role of pain catastrophizing. Pain Med 9:1164–1172
Moseley GL (2004) Evidence for a direct relationship between cognitive and physical change during an education intervention in people with chronic low back pain. Eur J Pain 8:39–45
Acknowledgements
Jessica Van Oosterwijck is financially supported by grant no. OZR1596 from the research council of the Vrije Universiteit Brussel, Brussels, Belgium. Willem De Hertogh is financially supported by grant no. G815 from the research council of the Artesis University College of Antwerp, Antwerp, Belgium.
Disclosures
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nijs, J., Van Oosterwijck, J. & De Hertogh, W. Rehabilitation of chronic whiplash: treatment of cervical dysfunctions or chronic pain syndrome?. Clin Rheumatol 28, 243–251 (2009). https://doi.org/10.1007/s10067-008-1083-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-008-1083-x