Abstract
To describe clinical and epidemiological data of Behçet’s disease (BD) in Brazil, we retrospectively reviewed records of all patients seen between 2006 and 2007 at the BD outpatient clinic of University of Sao Paulo. One hundred and six patients fulfilled the International Study Group for Behçet’s Disease diagnostic criteria and they were included in this study. There was a female/male ratio of 2.2:1 and mean age at diagnosis was 31.9 ± 9.2 years. In order of frequency, oral (100%) and genital ulcerations (92.5%), pseudofolliculitis (59.4%), erythema nodosum (49.1%), ocular lesions (47.2%), and musculoskeletal complaints (35.8%) were the most common manifestations. Blindness and major vessel involvement (18.2% vs. 5.5%, p = 0.038 and 27.3% vs. 9.6%, p = 0.019) were more frequent among male than female patients. We concluded that in Brazil, a South American country faraway from the Silk Route, BD follows the same pattern exhibited on its usual endemic area.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Behçet’s disease (BD) is a multisystemic inflammatory disorder characterized by recurrent oral and genital ulcerations, skin lesions, uveitis, and arthritis. The disease is distributed worldwide, but its prevalence and clinical features are strongly dependent on ethnic group and geographic area involved [1]. BD occurs endemically in the eastern Mediterranean area and in central and East Asian countries, coinciding with the “Silk Route”, an ancient trade route linking China to Italy. Higher prevalence rates are observed in Turkey: as high as 370 patients per 100,000 inhabitants in Anatolia [2] and 420 per 100,000 cases in Istanbul have been reported [3]. Iranian, Chinese, and Japanese prevalence rates are 16, 14, and 13 per 100,000, respectively, while USA and northern European countries have quite lower prevalence of BD, generally less than one case per 100,000 habitants [4]. In addition, familial occurrence of BD is higher in Asian countries than in Northern Europe, suggesting that in Western countries sporadic occurrence of BD is the rule, rather than the endemic form seen along the Silk Route [4].
Besides prevalence, some clinical patterns of BD may differ among populations. In Germany, patients with Turkish origin had more ocular lesions than German patients [5]. Gastrointestinal involvement is more frequent in Eastern Asia countries than in Turkey and also the aspect of intestinal lesions seems to be different: in Korea, large, isolated bowel ulcerations had been described, while multiple, shallow lesions were observed among Turkish patients[5]. Some authors have argued that such variations suggest that BD may be better described outside the Silk Route endemic area as a syndrome rather than a disease, unless pathologic expression of vasculitis is unequivocally demonstrated [6]. Brazil is a South American country with a multi-ethnic population, where BD is a rare disorder occurring as sporadic cases, similarly to other Western countries. Although national registry data about BD are not available, there are some referral centers that concentrate treatment of BD cases. Our aim in this study was to describe demographic and clinical features of the disease in Brazil through the analysis of BD patients observed in a university hospital in Sao Paulo, the largest city in the country.
Materials and methods
We performed a retrospective review of electronic records of all patients followed at the BD outpatient clinic of the Rheumatology Division at Sao Paulo University in Sao Paulo, Brazil over a 2-year period (2006 and 2007). In this period, data from medical routine interviews were inputted in a computer-based system specifically designed for BD clinical care. Records of patients were analyzed for demographic and clinical features, diagnostic criteria, complications, and treatment. We only included patients fulfilling the International Study Group for Behçet’s Disease (ISGBD) diagnostic criteria [7].
Mucocutaneous and articular involvements were systematically assessed at routine rheumatologist’s evaluation. Ocular involvement was considered only after ophthalmologic evaluation revealing uveitis or retinal vasculitis. Major vessel involvement (deep venous thrombosis, arterial thrombosis, or arterial aneurism) was evaluated by Doppler ultrasonography, computed tomography, or conventional angiography. Central nervous system (CNS) involvement was considered only in patients with objective neurological signs and neuroimaging findings or cerebrospinal fluid alterations (sporadic functional symptoms like headache or dizziness without objective abnormalities were not considered). Gastrointestinal (GI) involvement was only considered in patients with intestinal lesions demonstrated by upper or lower gastrointestinal endoscopy. Pathergy testing was performed in 21 patients presenting mucocutaneous or articular signs of disease activity at the time of the clinical interview. In these patients, overall BD activity was assessed by the validated Brazilian version [8] of the Behçet’s Disease Current Activity Form (BDCAF) [9].
Statistical analyses were performed by SPSS® 15.0 for Windows. Normal distribution was assessed by Shapiro–Wilk test. Results are expressed as mean ± standard deviation or median (range), for parametric and non-parametric distributions, respectively. Influence of gender on clinical features was assessed by comparing the proportion of affected male patients vs. the proportion of affected female patients by Pearson’s corrected chi-square test. Differences between groups were assessed by the Mann–Whitney test. A value of p < 0.05 was regarded as statistically significant.
Results
One hundred and twenty-eight patients were analyzed. ISGBD criteria were fulfilled by 106 patients who were included in this study. They were 73 females and 33 males (sex ratio female/male = 2.2/1). The mean age at BD diagnosis was 31.9 ± 9.2 years. Only two cases were from the same family. Delay between onset of symptoms and diagnosis of BD was 6.8 ± 8.0 years. There was a trend toward earlier diagnosis among male than female patients (29.0 ± 8.2 vs. 33.1 ± 9.4 years, p = 0.064). Clinical features are shown in Table 1.
Comparison of mucocutaneous signs according to patient’s gender demonstrated that erythema nodosum was more frequent in female than male patients (57.5% vs. 30.3%, p = 0.009) while pseudofoliculitis was more frequent in male patients than female (75.8% vs. 46.6%, p = 0.030). Genital ulceration was also more commonly observed among women (97.3% vs. 81.8%, p = 0.005).
Ocular findings were seen in 50 patients (47.2%), without significant gender influence. However, ten patients (9.4%) had irreversible visual impairment, leading to blindness, which was significantly more frequent among male patients (18.2% vs. 5.5%, p = 0.038). Musculoskeletal complaints occurred in 38 cases (35.8%), without significant gender influence, consisting mainly in recurrent episodes of inflammatory arthralgia or non-destructive oligoarthritis. Major vessel involvement, occurring in 17 patients (16.0%), was also more frequent among male than female patients (27.3% vs. 9.6%, p = 0.019) and deep venous thrombosis was the more frequent finding (ten cases); four patients had isolated arterial involvement and three had both arterial and venous findings. Neurological involvement, occurring in 19 patients (17.9%), consisted mainly of isolated cortical ischemic deficits (eight cases) and acute meningoencephalitis (six cases). Four cases had present combinations of diverse pyramidal, cranial nerve, and cortical findings with gradual evolution and only one had isolated cerebral vein thrombosis. Gastrointestinal findings were documented in seven cases (6.6%). Two patients had minor abdominal symptoms and multiple, shallow widespread aphtous ulcerations evidenced by gastroduodenal endoscopy studies. Chronic inflammatory findings at colonoscopy studies were observed in two cases, concentrated in ileocecal region with larger ulcers, and three had minor inflammatory findings on gastric or colonic mucosa associated with occasional bleeding. Of note, only three sacroiliitis were observed in this series, two of these occurring in the patients with chronic ileocecal inflammation.
Pathergy test was positive in five of 21 tested cases (23.8%). Remarkably, BDCAF scores of pathergy-positive patients (14.0 (12–23)) were significantly higher than BDCAF scores of pathergy-negative group (6 (1–24)), p = 0.031.
Beyond the 106 patients described above, there were other 22 patients attended on BD outpatient clinic who did not fulfill ISGBD diagnostic criteria at the time of this study. This group consisted of seven patients (31.8%) presenting recurrent oral ulcers and uveitis, six patients (27.2%) with oral and genital ulcers plus severe major vessel involvement (both venous and arterial) and three patients (13.6%) with oral and genital ulcers plus CNS involvement. Only six other patients (27.2%) suffered of recurrent oral and genital ulcers but did not develop any other systemic feature.
Discussion
We reported demographical and clinical features of 106 Brazilian patients classified according to ISGBD criteria [7] as BD patients. Brazil is a South American country located faraway from the Silk Route and has a multi-ethnic population. Prevalence of BD in Brazil cannot be assessed due to the lack of national epidemiologic surveys. However, our results resemble the low prevalence found in USA (0.12–0.33 per 100,000 habitants) [4], considering the ratio between the number of patients attending our outpatient clinic (106) and the population of Sao Paulo (more than 10 million people). Also, familial history was not a frequent finding. Therefore we hypothesize that BD in Brazil consists mainly of sporadic cases as occurs in different Western countries. Nevertheless, Brazilian BD cases show a similar clinical pattern to that one found in the endemic area of the disease.
Age of onset at the third decade is the most constant feature of disease around different populations [4] and it correlates well with our results. The female-to-male ratio in our series was 2.2:1. Similar results had been described in USA [10] and Western European countries. In Middle East countries, where previous reports described significant male predominance in BD cases, it has decreased until near 1:1 female-to-male ratios in more recent epidemiological studies [4]. Some authors have argued that male predominance in some Arabic countries was overestimated by the fact that women had less severe BD symptoms than men and used to seek medical assistance less frequently in these countries due to social restraints [11].
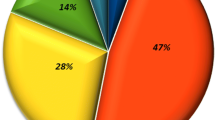
In order of frequency, oral ulcers (100%), genital ulcers (92.5%), pseudofolliculitis (59.4%), erythema nodosum (49.1%), ocular involvement (47.2%), and musculoskeletal complaints (35.8%) were the most common observed manifestations of BD in our series. Very similar values were shown in larger series in the Silk Route, as the multicenter Korean study (n = 1,527 patients with oral ulcers 98.8%, genital ulcers 83.2%, skin lesions 84.3%, ocular lesions 50.9%, and articular symptoms 38.4%) [12], the Iranian series (n = 4,900 patients with oral ulcers 97%, genital ulcers 65%, pseudofolliculitis 61%, erythema nodosum 22%, ocular lesions 56%, and arthropathy 35%) [13], and the Turkish series (n = 2,313 patients, with oral ulcers 100%, genital ulcers 88.1%, pseudofolliculitis 54%, erythema nodosum 47.6%, ocular lesions 29.1%, and arthropathy 11.6%) [14]. The frequency of major clinical manifestations in our series suggests that BD in Brazil follows the same pattern described in endemic area.
There is general agreement that gender influences BD expression. In the Turkish series, genital aphtae and erythema nodosum were more frequent among women, while papulopustular lesions in men [14], similar to our findings. Furthermore, severity of lesions seems to be greater in male patients: blindness occurred in 30% of male BD patients with uveitis vs. 17% of female BD patients with uveitis after 10 years of follow-up in Turkey [15]. We also found in Brazil significantly higher rates of blindness in male BD patients. We also observed that major vessel involvement was more frequently found in men, as it was described in Turkey [14] and Tunisia [11].
Pathergy test had positive reactions in 23.8% of cases. Curiously, we observed a relation between pathergy and BD activity. We assessed BD activity in these cases with the Brazilian version of BDCAF, which had shown reliable results on evaluation of BD mucocutaneous and articular manifestations [8] and observed that BDCAF scores were significantly higher in patients with positive pathergy reaction. In agreement to this evidence Chang and Cheon described that, of eleven patients with active BD and positive pathergy reaction, only two remained with positive pathergy during inactive phase of disease [16]. However, they and others [17] had found no difference in disease activity scores between groups with positive and negative pathergy reactions (probably because the scoring system used in these studies had not sufficient range of variability).
Visceral involvement in our population also had similar characteristics than Silk Route series. Particularly referring to gastrointestinal features, we observed that two main forms of involvement were present: shallow and widespread ulcerations (as the pattern described in Turkey) or large, isolated ulcers concentrated in ileocecal region (as described in Japan) [1, 4]. Remarkably, only three sacroiliitis were observed in our series and two of these were present in the two cases with ileocecal lesions, raising the possibility of inflammatory bowel disease as a differential diagnosis in such pattern of intestinal involvement, rather than BD. Unfortunately, in the present moment there is no information about prevalence of HLA-B51 in our series. HLA typing is a research goal for further characterizing Brazilian BD cases.
In conclusion, our study reveals that, in a relatively large sample of BD patients in Brazil, many similarities with the great series from the endemic area were found. It suggests that BD follows the same patterns even in a South American country with low rates of BD prevalence, faraway from the Silk Route. Therefore we conclude that clinical observation at presentation and follow-up of these patients, with reference to ISGBD diagnostic criteria (and careful evaluation of other inflammatory syndromes as differential diagnostic possibilities) may provide precise diagnosis of BD even in Western countries, with no need of pathologic demonstration of vasculitis.
References
Yurdakul S, Hamuryudan V, Yazici H (2004) Behçet Syndrome. Curr Opin Rheumatol 16:38–42
Yurdakul S, Günaydin I, Tüzün Y et al (1988) The prevalence of Behçet’s Syndrome in a rural area in northern Turkey. J Rheumatol 15:820–822
Azizlerli G, Köse AA, Sarica R et al (2003) Prevalence of Behçet’s disease in Istambul, Turkey. Int J Dermatol 42:803–806
Zouboulis CC (1999) Epidemiology of Adamantiades-Behçet’s disease. Ann Med Interne 150:488–498
Zoubolis CC, Kötter I, Djawari D et al (1997) Epidemiological features of Adamantiades-Behçet’s disease in Germany and Europe. Yonsei Med J 38:411–422
Ehrlich GE (1997) Vasculitis in Behçet’s disease. Int Rev Immunol 14:81–88
International Study Group for Behçet’s Disease (1990) Criteria for diagnosis of Behçet’s disease. Lancet 335:1078–1080
Neves FS, Moraes JC, Kowalski SC, Goldenstein-Shainberg C, Lage LV, Gonçalves CR (2007) Cross-cultural adaptation of the Behçet’s Disease Current Activity Form (BDCAF) to the Brazilian Portuguese language. Clin Rheumatol 26:1263–1267
Bhakta BB, Brennan P, James TE, Chamberlain MA, Noble BA, Silman AJ (1999) Behçet’s disease: evaluation of a new instrument to measure clinical activity. Rheumatology (Oxford) 38:728–733
Mangelsdorf HC, White WL, Jorizzo JL (1996) Report of twenty-five patients from the United States with prominent mucocutaneous involvement. J Am Acad Dermatol 34:745–750
Houman MH, Neffati H, Braman A et al (2007) Behçet’s disease in Tunísia. Demographic, clinical and genetic aspects in 260 patients. Clin Exp Rheumatol 4(Suppl 45):S58–S64
Bang D, Lee JH, Lee Es et al (2001) Epidemiologic and clinical survey of Behçet’s disease in Korea: the first multicenter study. J Korean Med Sci 16:615–618
Davatchi F, Sharam F, Kumar A et al (2004) Comparative analysis of Behçet’s disease in the APLAR region. APLAR Journal of Rheumatology 7:38–43
Tursen U, Gurler A, Boyvat A (2003) Evaluation of clinical findings according to sex in 2313 Turkish patients with Behçet’s disease. Int J Dermatol 42:346–351
Tugal-Tutkun I, Onal S, Altan-Yaycioglu R, Huseyin-Altunbas H, Urgancioglu M (2004) Uveitis in Behçet’s disease: an analysis of 880 patients. Am J Ophtalmol 138:373–380
Chang HK, Cheon KS (2002) The clinical significance of a pathergy reaction in patients with Behçet’s disease. J Korean Med Sci 17:371–374
Krause I, Moland Y, Mitrani M, Weinberger A (2000) Pathergy reaction in Behçet’s disease: lack of correlation with mucocutaneous manifestation and systemic disease expression. Clin Exp Rhematol 18:71–74
Disclosures
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Neves, F.S., Caldas, C.A.M., Lage, L.V. et al. Faraway from the Silk Route: demographic and clinical features of Behçet’s disease in 106 Brazilian patients. Clin Rheumatol 28, 543–546 (2009). https://doi.org/10.1007/s10067-008-1081-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-008-1081-z