Abstract
Kawasaki disease (KD) produces endothelial inflammation, which may lead to dilatation and aneurysms of coronary and peripheral arteries. Previous studies have suggested that these patients can present endothelial dysfunction that can predispose to coronary vascular events late after KD. The purpose of this study was to determine the cardiovascular risk profile and endothelial function of Chilean children with history of KD. In a prospective case-control study, 11 patients with history of KD (age 10.6 ± 2.0 years, interval from initial episode 8.1 ± 3.6 years) and 11 healthy, age-, gender-, and BMI z score-matched controls were evaluated with blood pressure (BP), a fasting lipid profile, high sensitivity C-reactive protein (hsCRP), and flow-mediated dilatation of the brachial artery (FMD). One KD patient (9.1%) had persistent coronary aneurysms. There was a significant difference of mean and log-transformed concentrations of hsCRP between case and control groups (2.3 ± 3.0 vs 0.5 ± 0.3 mg/l, P = 0.045). None of the patients with elevated hsCRP had persistent coronary arterial lesions. No difference was found in systolic BP z score between the case and control groups. Diastolic BP z score was significantly higher in cases than controls (P = 0.039). There were no significant differences of FMD between cases and controls. Mean fasting total cholesterol, high-density and low-density lipoprotein, and triglycerides in cases were normal, with no significant difference vs controls. This study shows that Chilean children with history of KD have increased levels of hsCRP, possibly reflecting persistent low-grade inflammation. The prognostic value of hsCRP in KD patients deserves further investigation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Kawasaki disease (KD) has become the first cause of acquired heart disease in children of developed countries. In its initial episode, patients present inflammation of medium-sized vessels, being coronary arteries (CAs) the most affected. About 15 to 25% of affected patients can develop aneurysms and/or coronary dilatation unless they receive timely treatment with intravenous immunoglobulin (IVIG) and aspirin [1]. It has been well documented that patients who develop severe dilatation or large aneurysms of CAs have a higher rate of morbidity and mortality due to obstruction or rupture of these arteries [2]. However, growing concern exists that the characteristic vasculitis of KD causes endothelial dysfunction (ED) on both coronary and peripheral arteries, which could be an early precursor of atherosclerosis and lead to coronary vascular events in these patients later in adulthood. The ED of these patients has been shown to be independent of treatment with IVIG [3] and the presence of coronary aneurysms or dilatation in the acute phase of the disease [4]. Since the first case of KD was reported in 1967 [5], the follow-up of these patients has not been long enough to define the natural history of this disease.
Recently, considerable interest has arisen in the study of traditional and novel cardiovascular risk factors in patients with history of KD to identify what patients could have a higher risk of coronary events. Alterations of endothelial function (EF) measured by flow-mediated dilatation (FMD) of the brachial artery [3, 4, 6–8], carotid intima-media thickness [9], arterial stiffness [9–11], lipids [7, 9, 10, 12], high sensitivity C-reactive protein (hsCRP) [10, 13], and serum amyloid A [13] have been documented as risk markers in investigations from Japan, China, and Western developed countries.
The purpose of this study was to determine the cardiovascular risk profile and EF of Chilean children with history of KD through the evaluation of endothelium-dependent FMD of the brachial artery, hsCRP as a novel risk marker, and lipid profile.
Materials and methods
A prospective case-control study was conducted at our university hospital. Eleven patients of age 8 years or older with history of Kawasaki disease more than 12 months before study initiation were recruited. All patients were Chilean, a blend of European, mainly Spaniard, and American Indian ethnicities. Kawasaki disease was diagnosed by standard criteria [1]. All patients had at least three bidimensional echocardiograms at the time of the initial episode of KD. Subjects with evidence of smoking, diabetes mellitus, renal failure (serum creatinine greater than 1.5 mg/dl), and users of EF modifying drugs, such as statins, angiotensin-converting enzyme inhibitors, or calcium channel blockers, were excluded from the study.
Clinical characteristics and pharmacological treatment of the initial episode and current cardiovascular risk factors were registered. Physical examination was performed by a pediatrician and included weight, height, blood pressure (BP), and heart rate. Blood pressure was measured as suggested by The Fourth Report on the Diagnosis, Evaluation, and Treatment of High Blood Pressure in Children and Adolescents [14].
Eleven healthy, age-, gender-, and body mass index (BMI) z score-matched control patients without known cardiovascular risk factors were recruited as controls.
All cases and controls were evaluated with endothelium-dependent FMD of brachial artery, hsCRP, total cholesterol (TC), low-density lipoprotein (LDL), high-density lipoprotein cholesterol (HDL), and triglycerides (TG).
This study was approved by the Ethics Committee of the Faculty of Medicine at the Pontificia Universidad Católica de Chile. Informed consent was obtained from children and their parents or guardians.
Ultrasound assessment of endothelial function
Assessments were performed after 12-h fasting overnight. FMD was evaluated by an experienced cardiologist from the Department of Cardiovascular Diseases of our institution in all patients. High-resolution vascular ultrasound method was used based on the protocol suggested by the International Brachial Artery Reactivity Task Force [15]. The subject lay down in supine position, with the non-dominant arm in a comfortable position before the exam. Brachial artery was visualized in a longitudinal view of approximately 5 cm over the antecubital fold. Ultrasound gain was adjusted to obtain optimal delineation of the intima in both anterior and posterior vessel walls. Three baseline arterial diameter measurements were done at end of diastole from intima to intima with an electronic calyper. After measuring baseline diameter of the artery, reactive hyperemia was induced by occluding arterial blood flow for 5 min by using a sphygmomanometer inflated to 50 mmHg over systolic BP of the subject, after which cuff was rapidly deflated. One minute later, three measurements of arterial diameter were done and averaged. FMD is expressed as percentage of change in arterial diameter and was calculated by dividing the average arterial diameter after cuff deflation by the baseline diameter.
Laboratory assays
Overnight fasting venous samples were drawn in all subjects. High sensitivity CRP was measured by a nephelometric method (Dade Behring, Deerfield, IL, USA). Lipid profile was measured using a homogenous enzymatic colorimetric test (Hitachi, Tokyo, Japan). LDL cholesterol was calculated using the Friedwald formula. Cut-off points for lipid levels were defined according to the National Cholesterol Education Program guidelines for children [16].
Statistical analysis
Sample size was calculated in a two-tailed analysis to determine a difference in FMD of 5% with a SD of 4% with 80% power at a 5% significance level. Z score was used for standardizing values of body mass index and blood pressure. The latter was calculated as suggested by The Fourth Report on the Diagnosis, Evaluation, and Treatment of High Blood Pressure in Children and Adolescents [14]. Differences in risk factors between case and control subjects were analyzed by using Mann–Whitney U tests for non-parametric variables. The distribution of hsCRP is asymmetric, so a logarithmic transformation (log) of hsCRP was used for comparing cases and controls. Pearson bivariate correlation was used to determine the association between FMD, hsCRP, TC, and other variables such as age, gender, and time since acute disease. Statistical significance was assumed at P < 0.05. All values are expressed as mean ± standard deviation (SD) unless specified otherwise. In the case of hsCRP, due to asymmetry of samples and to reduce effect of outliers, we also report median and interquartile distance. The data were analyzed by using Statistical Package for the Social Sciences software version 13.0.
Results
Eleven patients (seven boys) aged 10.6 ± 2.0 years (range, 8–14 years) were recruited into the study. Clinical characteristics of cases and control groups are shown in Table 1. There was no significant difference in age, gender, or BMI z score between patients and control subjects. Age of presentation of KD was 2.53 ± 1.8 years (range, 3 months–6 years). Study follow-up assessment occurred at a mean interval after the initial KD episode of 8.1 ± 3.6 years. All patients received IVIG and aspirin in the acute phase of disease. Only one patient had two persistent small coronary aneurysms at the time of enrollment. All patients currently had normal functional capacity according to New York Heart Association classification and a normal cardiovascular physical examination. In each group, eight patients (73%) had normal BMI, and three patients (27%) had BMI > p95.
Results of BP z score, lipid profile, hsCRP, and FMD in cases and controls are shown in Table 1. There was no significant difference between cases and controls regarding mean systolic BP z score (0.14 ± 0.76 vs 0.16 ± 1.15, P = 0.948). Cases had significantly higher mean diastolic BP z score than controls (0.41 ± 1.07 vs −0.14 ± 0.33, P = 0.039). Only one patient in the KD group had diastolic BP over percentile 95 for gender, age, and height.
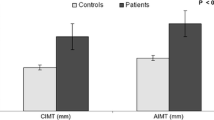
There was a significant difference of mean concentrations of hsCRP between case and control groups (2.3 ± 3.0 vs 0.5 ± 0.3 mg/l, P = 0.045; Fig. 1). Log-transformed concentrations of hsCRP were also significantly different between groups (0.05 ± 0.55 vs −0.38 ± 0.3 mg/l, P = 0.045). The median and interquartile distance of hsCRP in cases were 1.18 ± 2.58 mg/l and in controls 0.43 ± 0.58 mg/l. There was one KD patient with a very high level of hsCRP (10.40 mg/l). At the moment of evaluation, she had no clinical evidence of infection or other inflammatory process. No significant correlations were found between hsCRP and age, gender, BMI z score, TC, HDL, LDL, TG, or FMD.
Mean fasting TC, HDL, LDL, and TG in the case group were normal. Only one patient had a mild elevation of TC over 200 mg/dl. All other individual values were within normal limits. There was no significant difference between cases and controls in fasting lipid profile values.
There was no significant difference between cases and controls regarding mean endothelium-dependent FMD (11.1 ± 5.7 vs 8.0 ± 2.9%, respectively; P = 0.12; Fig. 2). There were no significant correlations between FMD and age, gender, BMI z score, TC, HDL, LDL, TG, or hsCRP.
The only patient with persistent coronary aneurysms had FMD, hsCRP, and lipid profile within normal limits.
Discussion
The findings of this study demonstrate that Chilean children with history of KD have significantly higher hsCRP and diastolic BP compared to healthy children. EF and lipid profile were not significantly different between groups. These results suggest that KD patients may have low-grade inflammation years after initial episode of the disease.
To date, there is no clear cut-off point for hsCRP in children. High sensitivity CRP above 3.0 mg/l has been categorized as high risk in adults according to a CDC/AHA statement [17] and has been used previously as the cut-off point in studies done in adolescents [18]. Three of our KD patients (27%) had hsCRP above this value. In a study of 112 healthy Chilean children without cardiovascular risk factors, the mean of hsCRP was 0.9 ± 1.5 mg/l and the median was 0.43 mg/l [19]. Eighty-two percent of the cases in our study were above this median and above the median of 0.4 mg/l reported by Ford et al. [20] in the National Health and Nutrition Examination Survey, 1999–2000.
Our results are in agreement with previous reports, which have shown that patients with history of KD have increased hsCRP plasma levels. However, in contrast with a previous study, which showed increased hsCRP only in patients with history of coronary arterial lesions (CALs) [13], our patients with elevated hsCRP did not have persistent CALs, suggesting that low-grade inflammation may also be present in the large subgroup of children who have had KD without persistent CALs.
High sensitivity CRP is currently the most extensively studied and validated measure of vascular inflammation [21]. Levels of hsCRP can predict the risk of future vascular disease in adults. In a perspective article published in 2004, Ridker et al. [22] proposed CRP to be added to the assessment of global cardiovascular risk in adult subjects without coronary heart disease, as CRP measurement is a well-standardized and inexpensive determination method, which is widely available, and practical to use in outpatient clinical settings.
The cases in our study also had significantly higher diastolic BP z score than controls. A previous case-control study that analyzed cardiovascular risk after KD found significantly higher systolic and diastolic BP in KD patients than in healthy children [7]. We believe hypertension should be actively sought in KD patients, as it is a treatable cardiovascular risk factor of growing concern in pediatric population.
Several studies have also shown alterations of lipid profile (especially low HDL) late after KD [7, 9, 10, 12]. Lipids in our patients revealed no difference compared to control subjects. Specifically, none of our patients had low HDL as demonstrated in previous studies. This could be explained by the small sample of patients, and also by racial or nutritional differences between our populations.
In our study, FMD was not significantly different between cases and control subjects. As it was designed to detect differences in mean FMD of 5% with a SD of 4%, it is likely that power was not enough to detect smaller differences between groups. In addition, dispersion of values in other reports is high, making it harder to interpret small series.
Other studies have shown alterations in endothelium-dependent FMD in both patients that suffered dilatation and/or aneurysms in the acute phase of KD and in those who did not present macroscopic alterations of CAs [4]. In addition, ED has been observed in a similar pattern in patients that received IVIG as in those who did not receive this treatment [3]. This suggests that treatment in the initial episode of the disease can prevent macroscopic alterations from occurring, but not ED.
Another study of 27 patients, 15 years after the acute phase of KD, has largely increased our knowledge about the relationship between ED and coronary disease in KD [23]. This investigation directly correlated EF in CAs with myocardial flow reserve. Similar to the ED that has been demonstrated in peripheral arteries, significant alterations were observed in coronary territories in regions with regressed aneurysms and in those with no evidence of having suffered changes in coronary anatomy. This implies that KD could also leave functional sequelae in CAs of patients with no acute macroscopic alterations of these vessels. Deng et al. [3] have also demonstrated that ED of the brachial artery in KD patients, in spite of being persistent in time, is not a fixed alteration because a marked improvement of endothelium-dependent FMD has been registered with the administration of intravenous ascorbic acid.
A recent scientific statement from the American Heart Association Expert Panel on Population and Prevention Science and other organizations developed practical recommendations for the management of cardiovascular risk in patients with history of KD [24]. Patient stratification was based on the status of CAs: patients with persistent aneurysms, high risk; patients with regressed aneurysms, moderate risk; and patients without detected abnormalities, at risk. The statement encouraged all KD patients to exercise to the greatest extent possible given coronary artery status, in accordance with the 36th Bethesda Conference recommendations [25]. Although the statement recognized the presence of abnormal values of hsCRP, endothelial reactivity, and other cardiovascular risk markers after KD, it did not include any of them in the risk stratification of these patients and relied exclusively on the macroscopic alterations of CA.
Albeit small in size, up to our current knowledge, this is the first study in Latin America of cardiovascular risk factors, including a novel risk marker and EF in children with KD. The present study confirms that children with history of KD have increased levels of hsCRP, possibly reflecting low-grade inflammation, even in patients without persistent CALs. The prognostic value of hsCRP in KD patients deserves further investigation.
References
Newburger JW, Takahashi M, Gerber MA et al (2004) Diagnosis, treatment, and long-term management of Kawasaki disease: a statement for health professionals from the Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease, Council on Cardiovascular Disease in the Young, American Heart Association. Pediatrics 114:1708–1733
Kato H, Sugimura T, Akagi T et al (1996) Long-term consequences of Kawasaki disease. A 10-to 21-year follow-up study of 594 patients. Circulation 94:1379–1385
Deng YB, Li TL, Xiang HJ et al (2003) Impaired endothelial function in the brachial artery after Kawasaki disease and the effects of intravenous administration of vitamin C. Pediatr Infect Dis J 22:34–39
Dhillon R, Clarkson P, Donald AE et al (1996) Endothelial dysfunction late after Kawasaki disease. Circulation 94:2103–2106
Kawasaki T (1967) Acute febrile mucocutaneous syndrome with lymphoid involvement with specific desquamation of the fingers and toes in children [in Japanese]. Arerugi 16:178
Ikemoto Y, Ogino H, Teraguchi M et al (2005) Evaluation of preclinical atherosclerosis by flow-mediated dilatation of the brachial artery and carotid artery analysis in patients with a history of Kawasaki disease. Pediatr Cardiol 26:782–786
Silva AA, Maeno Y, Hashmi A et al (2001) Cardiovascular risk factors after Kawasaki disease: a case-control study. J Pediatr 138:400–405
Kadono T, Sugiyama H, Hoshiai M et al (2005) Endothelial function evaluated by flow-mediated dilatation in pediatric vascular disease. Pediatr Cardiol 26:385–390
Noto N, Okada T, Yamasuge M et al (2001) Noninvasive assessment of the early progression of atherosclerosis in adolescents with Kawasaki disease and coronary artery lesions. Pediatrics 107:1095–1099
Cheung YF, Ho MH, Tam SC et al (2004) Increased high sensitivity C reactive protein concentrations and increased arterial stiffness in children with a history of Kawasaki disease. Heart 90:1281–1285
Ooyanagi R, Fuse S, Tomita H et al (2004) Pulse wave velocity and ankle brachial index in patients with Kawasaki disease. Pediatr Int 46:398–402
Newburger JW, Burns JC, Beiser AS et al (1991) Altered lipid profile after Kawasaki syndrome. Circulation 84:625–631
Mitani Y, Sawada H, Hayakawa H et al (2005) Elevated levels of high-sensitivity C-reactive protein and serum amyloid-A late after Kawasaki disease: association between inflammation and late coronary sequelae in Kawasaki disease. Circulation 111:38–43
National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents (2004) The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics 114:555–576
Corretti MC, Anderson TJ, Benjamin EJ et al (2002) Guidelines for the ultrasound assessment of endothelial-dependent flow-mediated vasodilation of the brachial artery: a report of the International Brachial Artery Reactivity Task Force. J Am Coll Cardiol 39:257–265
National Cholesterol Education Program (1992) Report of the expert panel on blood cholesterol levels in children and adolescents. Pediatrics 89(Suppl):525–584
Pearson TA, Mensah GA, Alexander RW et al (2003) Markers of inflammation and cardiovascular disease: application to clinical and public health practice: a statement for healthcare professionals from the Centers for Disease Control and Prevention and the American Heart Association. Circulation 107:499–511
Ford ES, Ajani UA, Mokdad AH et al (2005) The metabolic syndrome and concentrations of C-reactive protein among U.S. youth. Diabetes Care 28:878–881
Acevedo M, Arnaiz P, Barja S et al (2007) Relationship of C-reactive protein to adiposity, cardiovascular risk factors and subclinical atherosclerosis in healthy children. Rev Esp Cardiol 60:1051–1058
Ford ES, Giles WH, Myers GL et al (2003) C-reactive protein concentration distribution among US children and young adults: findings from the National Health and Nutrition Examination Survey, 1999–2000. Clin Chem 49:1353–1357
Albert MA, Ridker PM (2006) C-reactive protein as a risk predictor: do race/ethnicity and gender make a difference? Circulation 114: e67–e74
Ridker PM, Wilson PW, Grundy SM (2004) Should C-reactive protein be added to metabolic syndrome and to assessment of global cardiovascular risk? Circulation 109:2818–2825
Furuyama H, Odagawa Y, Katoh C et al (2003) Altered myocardial flow reserve and endothelial function late after Kawasaki disease. J Pediatr 142:149–154
Kavey RE, Allada V, Daniels SR et al (2006) Cardiovascular risk reduction in high-risk pediatric patients: a scientific statement from the American Heart Association Expert Panel on Population and Prevention Science; the Councils on Cardiovascular Disease in the Young, Epidemiology and Prevention, Nutrition, Physical Activity and Metabolism, High Blood Pressure Research, Cardiovascular Nursing, and the Kidney in Heart Disease; and the Interdisciplinary Working Group on Quality of Care and Outcomes Research: endorsed by the American Academy of Pediatrics. Circulation 114:2710–2738
Graham TP Jr, Driscoll DJ, Gersony WM et al (2005) 36th Bethesda Conference: recommendations for competitive athletes with cardiovascular disease: Task Force 2. J Am Coll Cardiol 45:1326–1333
Acknowledgments
This study was funded by a Resident Project Grant PG29-05 of the Pontificia Universidad Católica de Chile School of Medicine.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Borzutzky, A., Gutiérrez, M., Talesnik, E. et al. High sensitivity C-reactive protein and endothelial function in Chilean patients with history of Kawasaki disease. Clin Rheumatol 27, 845–850 (2008). https://doi.org/10.1007/s10067-007-0808-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-007-0808-6