Abstract
This is a cross-sectional study that analyzed the pattern and frequency of articular and ophthalmologic manifestations in patients with Crohn’s disease (CD) and ulcerative colitis (UC), with or without signs of active bowel inflammation. One hundred and thirty consecutive patients with CD (n = 71) and UC (n = 59) were examined. Simple X-rays of lumbar spine, sacroiliac joints, and calcaneal bone were performed and human leukocyte antigen (HLA)-B27 was typed. Joint manifestations occurred in 41 (31.5%) patients, 27 (38%) with CD and 14 (23.7%) with UC. Peripheral involvement occurred in 22 patients, axial involvement in five, and mixed involvement in 14. The most frequently involved joints were knees (56.1%), ankles (29.3%), and hips (29.3%), while the predominant pattern was oligoarticular (84.6%) and asymmetrical (65.6%). Enthesitis was identified in seven (5.4%) patients and inflammatory lumbar pain in 13 (10%). Eight of these patients fulfilled the diagnostic criteria for ankylosing spondylitis (6.2%). Radiographic sacroiliitis occurred in 12 patients (9.2%). Ocular abnormalities were present in six patients (6.2%), and HLA-B27 was positive in five (5.8%). In conclusion, the articular manifestations in the present study were predominantly oligoarticular and asymmetric, with a low frequency of ophthalmologic involvement and positive HLA-B27.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Articular involvement is the most common extraintestinal manifestation in patients with Crohn’s disease (CD) and ulcerative colitis (UC) [1–4]. It has been recognized since 1930 [5], but it was only in 1958 that Bywaters and Ansell [6] described the “colitic arthritis” as a specific condition, different from rheumatoid arthritis. It was lately called enteropathic arthritis [7] and classified as one of the diseases of the spondyloarthropathy group [8]. The diseases classified as spondyloarthropathies are quite frequent and, recently, their prevalence in the general population of Berlin, Germany was estimated as 1.9% [9], which could make these diseases, as a group, more prevalent than rheumatoid arthritis.
Historically, two principal patterns of arthritis in inflammatory bowel disease have been recognized: (1) peripheral arthritis, often asymmetric; and (2) axial involvement, including sacroiliitis with or without spondylitis similar to idiopathic ankylosing spondylitis (AS), which course is independent of the intestinal disease and has an association with human leukocyte antigen (HLA)-B27. More recently, in an Oxford study [10], it has been proposed that peripheral arthritis should be divided as: type I, a pauciarticular arthritis, acute and self-limiting, that usually occurs during exacerbations of the inflammatory bowel disease and is not associated with the antigen HLA-B27; and type II, a polyarthritis, which symptoms usually persist for months to years, with an independent course of the intestinal disease. Periarticular manifestations such as enthesitis, tendinitis, and periostitis may occur [11–13].
In the literature, the frequency of articular manifestations in CD and UC ranged from 2.8% to 62%, depending on the methodology of the study, the population assessed, and the duration of the intestinal disease [1–4, 6, 12, 14–26].
The information in the Brazilian population is sparse, as only two studies approached this issue: a retrospective one with 98 UC patients, published by Goldfarb et al. [26] in 1985; and a prevalence study of CD and UC and the extraintestinal manifestations by Souza et al. [2] in 2002. We evaluated the articular complaints in Brazilian patients with CD and UC, as well as the ophthalmologic abnormalities and the frequency of HLA-B27, in order to improve our knowledge of these characteristics.
Materials and methods
A cross-sectional study was conducted at the Bowel Outpatient Clinic of the Unit of Gastroenterology of the Hospital das Clínicas of Federal University of Minas Gerais, from August 2000 to March 2003, in order to investigate the pattern and frequency of joint manifestations in patients suffering from Crohn’s disease and ulcerative colitis, with or without signs of active bowel inflammation. One hundred and forty-four patients were examined, consecutively, by the same rheumatologist, and 130 agreed to participate in the study—71 with CD and 59 with UC. The frequencies of ocular manifestations and of HLA-B27 antigen were also investigated.
The diagnosis of CD and UC was made by a gastroenterologist and was based on clinical, endoscopic, and histological evaluation [27, 28]. The disease activity, assessed by a gastroenterologist, was based on clinical and inflammatory markers and, in some patients, also on endoscopic and histological evaluation. The extent and localization of intestinal disease were classified according to endoscopic findings: Vienna classification [29] was used for CD patients, and UC patients were classified as described by Farmer [30].
Patient evaluation
Patients were submitted to a complete clinical examination by a rheumatologist. Actual arthralgia or arthritis, the presence of inflammatory back pain, and the pattern of axial or peripheral joint involvement were defined by the rheumatologist during the clinical examination. They were also asked about the presence of ocular symptoms and skin lesions. Previous articular complaints were not analyzed. Inflammatory back pain was defined as proposed by Calin et al. [31]. Enthesitis was defined as Achilles tendinitis and/or plantar fasciitis and/or pain and/or swelling in tibial tubercle [32]. An ocular examination was performed by the same ophthalmologist, regardless of the presence of any signs or symptoms of ocular abnormalities.
Radiological evaluation
Anteroposterior view of the sacroiliac joints, in Ferguson incidence, was obtained. Sacroiliitis was classified according to the New York criteria [33]. Patients were also submitted to calcaneal and lumbar spine X-rays. Radiographs were analyzed independently by three investigators: the author, another rheumatologist, and a radiologist that did not know patients’ clinical complaints. The end result was defined by a consensus among the investigators.
HLA tissue typing
Eighty-six patients were typed for HLA-B27 antigen by polymerase chain reaction. HLA-B27 subtypes were not investigated.
Statistical Analysis
Student’s t test was used to compare continuous variables and the chi-squared test was used to compare the different groups. Yates’ correction was used if necessary. If one cell had an expected count less than one, Fischer’s exact test was used. P values of <0.05 were regarded as significant.
Ethics
The study was approved by the Ethics and Research Committee of the Federal University of Minas Gerais.
Results
One hundred and thirty consecutive patients with the diagnosis of CD (n = 71) and UC (n = 59) were submitted to a detailed examination by the same rheumatologist. Demographic features are shown in Table 1. Comparative analysis between the two groups showed no statistically significant differences.
Intestinal disease distribution in CD was: 16.9% ileitis, 18.3% colitis, 26.8% proximal small bowel disease, and 35.2% ileocolonic. The disease extent in UC patients was: 20.3% proctitis, 23.7% pancolitis, 25.4% left colon, and 30.5% proctosigmoiditis. Concomitant to the rheumatological evaluation, there was inflammatory activity of the bowel disease in 55.4% of the patients: 47.9% of CD patients and 64.4% of UC patients (p = 0.087).
Locomotor involvement
Joint manifestations were present in 41 (31.5%) patients, 27 (38%) being of the CD group and 14 (23.7%) of the UC group (p = 0.119; Table 2). Peripheral involvement—painful joint and/or arthritis and/or enthesitis—occurred in 22/41 (53.7%) patients, 13/27 (48.1%) being with CD and 9/14 (64.2%) with UC (p = 0.820). Five of 41 patients (12.2%) presented axial involvement: 4/27 (14.8%) with CD and 1/14 (7.1%) with UC (p = 0.376). Mixed involvement, i.e., peripheral and axial, was present in 14 (34.1%) patients: 10/27 (37.0%) with CD and 4/14 (28.6%) with UC (p = 0.292).
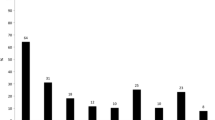
During the study, arthritis was identified by physical examination in 21 (16.2%) of the 130 patients: 14 (19.7%) of the CD group and seven (11.9%) of the UC group (p = 0.331), while inflammatory arthralgia, without swelling, was observed in seven patients with CD and in five patients with UC (p = 0.973). The most frequently involved peripheral joints were knees (56.1%), ankles (29.3%), and hips (29.3%), while the predominant pattern of joint involvement was oligoarticular (84.6%) and asymmetrical (65.6%). The median duration of arthritis was 8weeks in the individuals with CD and 4weeks in those with UC (p = 0.272).
Seven (5.4%) patients presented enthesitis, which was the only articular manifestation in three. The insertion of the Achilles tendon was most frequently involved (six patients). It predominated in CD (five patients), although there was no statistical significance (p = 0.219). One UC patient showed pain and swelling in the insertion of the patella tendon at the right tibial tubercle.
Inflammatory lumbar pain was present in 13 (10%) patients, eight (11.3%) being of the CD group and five (8.5%) of the UC group (p = 0.814). Eight of these patients fulfilled the diagnostic criteria for AS, corresponding to 6.2% of all patients studied; they were predominantly men (6/8) and presented CD (8/8).
Peripheral involvement was associated with episodes of activity of the bowel disease, in contrast to the axial involvement (p = 0.006). Articular manifestations were predominant in individuals with CD with colonic involvement but with no statistical significance. The bowel disease preceded the articular signs and symptoms in all patients with exclusive peripheral arthritis. In contrast, the articular manifestations preceded CD diagnosis in five of eight patients who fulfilled the diagnostic criteria for AS.
Radiographic abnormalities
Abnormalities of the sacroiliac joint X-rays were identified in 12/130 patients (9.2%): ten (14.1%) patients of the CD group and two (3.4%) of the UC group (p = 0.072), being bilateral in the majority of the cases (91.7%). Other characteristics of the sacroiliitis are shown in Table 3.
The analysis of lumbar spine X-rays showed a normal exam in all UC patients and some abnormalities in four CD patients, which fulfilled the criteria for AS. The abnormalities were sindesmophytes, Romanus sign, and squaring of vertebra. Calcaneal X-rays were normal in all 130 patients.
HLA-B27
Eighty-six patients were tested for the HLA-B27 antigen (50 CD and 36 UC), which was positive in five (5.8%). It was tested in 25 from 27 CD patients who had articular symptoms: six had axial symptoms, all of them fulfilled AS criteria, and only one patient had a positive test. Between UC patients, 12 were tested from 14 who had articular symptoms; two of them had axial symptoms, both were negative for HLA-B27. None fulfilled criteria for AS. All patients positive for HLA-B27 had CD (p = 0.071). Three female patients had articular manifestations (60%). One had only inflammatory back pain, another had enthesitis of Achilles tendon, and the other had inflammatory back pain, radiographic sacroiliitis, and peripheric arthritis. This last patient fulfilled criteria for AS. HLA-B27 was tested in six of the eight patients with AS and was positive in one (16.7%).
Ocular manifestations
Eye examination was performed in 96 patients (59 CD and 37 UC) and showed some type of involvement in six (6.2%): four with CD and three females. Anterior uveitis was identified in four (two females), being bilateral in two individuals. One of the two males with anterior uveitis had AS. None had the acute form and one had posterior synechias. A female with CD had unilateral anterior nodular scleritis while a male with CD had unilateral nodular episcleritis, recurrent peripheric arthritis, and psoriasis.
The frequency of eye involvement at the time of examination was similar between patients with CD (6.8%) and UC (5.4%; p = 1.000) and between sexes (p = 0.678). There was no statistical association with inflammatory activity of bowel disease or with arthritis. It was not possible to analyze the association between the HLA-B27 and ocular abnormalities because only three of the six patients had been tested for HLA-B27; all of them were negative for this antigen.
Discussion
The precise prevalence of articular manifestations of spondyloarthropathy in patients presenting inflammatory bowel disease has been difficult to determine because of methodological differences in the studies. Most of them were performed before the development of the European Spondyloarthropathy Study Group criteria [8]; some were conducted by gastroenterologists, others by rheumatologists, and some did not use routine radiographic studies to identify asymptomatic sacroiliitis [11, 22, 24]. Table 4 presents the frequency of articular manifestations and HLA-B27 in patients with Crohn’s disease and ulcerative colitis, according to different studies.
We studied a population of patients with CD and UC from a tertiary referral center, in a cross-sectional way, for the presence of articular manifestations. The frequency was higher than in previous studies performed in the general population [1, 22, 24, 34] and was similar to those which used a study methodology similar to ours [23]. The inclusion of patients from a tertiary referral center might reflect referral bias, as they might represent more severe and complicated cases.
The prevalence of the different musculoskeletal manifestations was similar in CD and UC patients, in accordance with many other studies [1, 15, 17, 22, 24]. An exception was AS-like involvement, which was observed only among patients with CD. The absence of such a manifestation in UC patients in the literature is uncommon.
The frequency of peripheral synovitis was high and comparable with other recent studies [18, 21]. The oligoarticular pattern was the predominant one, as described in many reports [1, 18, 19, 22, 23]. This pattern may resemble the type I arthropathy reported by Orchard et al. [10]. The type II arthropathy occurred in only one patient in this study. Interestingly, there was a high frequency of monoarticular involvement (36.3%), such as reported by De Vlam et al. [23] (50%). The high frequency of hip involvement is remarkable, which was as frequent as the ankles but less frequent than the knees. Among nine patients that had pain and/or limitation of the hips, five fulfilled the classification criteria for AS.
Enthesitis was found in a frequency similar to other studies [18, 23, 24]. Interestingly, it was the only rheumatological manifestation in three patients, a fact that has also been recognized by De Vlam et al. [23]. One of these patients was positive for HLA-B27. This is a relevant data as enthesitis is a specific manifestation of spondyloarthropathies and may be the sign of presentation of one of the diseases of this group, specially in young people [35, 36].
The frequency of AS-like involvement in this study is in accordance to several other authors that identified frequencies varying from 2.9% to 10% [12, 15, 19, 22–24]. Despite being more common in males, the association between axial AS-like involvement and sex was not statistically significant, probably due to the small number of patients with AS in this study. This issue is controversial in the literature. Some authors detected results similar to ours [22, 37], while others identified a predominance of male sex [24, 38].
It is difficult to compare the frequencies of radiographic sacroiliitis among the studies in the literature due to the differences in the methods used. Some authors analyzed only symptomatic patients, and another evaluated all patients by image. Evaluation of pelvic radiographs for the presence of sacroiliitis is difficult and is liable to interobserver variability. We agree with De Vlam et al. [23], who stated that although other techniques, such as computerized tomographic scans or magnetic resonance imaging, are superior in detecting sacroiliitis, they cannot be used for screening due to the high radiation exposure, high cost, and limited availability.
The extent of gastrointestinal inflammation was similar in patients with or without articular manifestations in both CD and UC groups and coincides with some studies [12, 16]. Previous studies have shown conflicting results; early reports indicated a correlation of the incidence of peripheral arthritis and the extent of bowel inflammation in UC [14]. A higher prevalence of arthritis with colonic involvement in CD patients was described by some authors [18, 22].
The frequency of HLA-B27 was low if compared to similar studies carried out in other countries [18, 23, 24] and similar to others [15, 16, 22]. They described frequencies between 3.6% and 24%. This might be related to the low frequency of this antigen in Brazilian population: 4% in one study [39] and 3.5% in another [40]. It is known that the strength of disease association with HLA-B27 varies markedly among the various diseases of spondyloarthropathy group as well as among different ethnic populations. In Brazil, there is no other study of HLA-B27 and articular manifestations in patients with inflammatory bowel disease. So, it is not possible to compare our data. The analysis of association between HLA-B27 with the type of articular involvement, with sex, and with ocular manifestations was not possible because of the reduced number of patients positive for this antigen (five patients of 86 tested). Otherwise, it is interesting to notice that the low frequency of HLA-B27 seemed not to influence the frequency of ocular and rheumatological manifestations in the studied gut diseases as the frequency of those manifestations was similar to various studies in the literature, as already reported.
The frequency of ocular abnormalities identified in our patients is in accordance with other authors, who showed a variation of 1.5% to 11.8% [12, 17, 25, 34]. The characteristics of the uveitis in individuals of our study were similar to those described by other investigators [40–44], which are insidious onset, chronic, and bilateral. It is interesting to notice that it is quite different from the uveitis associated to AS and to HLA-B27 [44–46]: anterior, acute, unilateral, and recurrent.
In conclusion, the analysis of this series of Brazilian patients with CD and UC showed us that the frequency of the articular manifestations was high in those patients and similar to other series studied all over the world. The pattern of the articular manifestations was also in accordance to studies carried out in other countries. The low frequency of HLA-B27 might be related to the low frequency of this antigen in our population. This seemed not to influence the frequency of ocular and rheumatological manifestations in the gut diseases studied. Physicians must pay attention to the presence of some rheumatological manifestations related to spondyloarthropathies in order to make a prompt and proper diagnosis and to initiate the specific therapy, which will certainly improve the prognosis.
References
Palm O, Moum B, Ongre A, Gran JT (2001) The prevalence and incidence of peripheral arthritis in patients of inflammatory bowel disease, a prospective population-based study (the IBSEN Study). Rheumatology 40(11):1256–1261
Souza MHLP, Troncon LEA, Rodríguez CM et al (2002) Evolução da ocorrência (1980–1999) da doença de Crohn e da retocolite ulcerativa idiopática e análise de suas características clínicas em um Hospital Universitário do sudeste do Brasil. Arq Bras Gastroenterol 339(2):98–105
Turkcapar N, Toruner M, Soykan I et al (2006) The prevalence of extraintestinal manifestations and HLA association in patients with inflammatory bowel disease. Rheumatol Int 26(7):663–668
Mendoza JL, Lana R, Taxonera C et al (2005) Extraintestinal manifestations in inflammatory bowel disease: differences between Crohn’s disease and ulcerative colitis. Med Clin (Barc) 25(8):297–300
Bargen JA (1930) Complications and sequelae of chronic ulcerative colitis. Ann Intern Med 3:335–352
Bywaters EGL, Ansell BM (1958) Arthritis associated with ulcerative colitis: a clinical and pathologic study. Ann Rheum Dis 17:169–183
Moll JMH, Haslock I, Macrae IF, Wright V (1974) Association between ankylosing spondylitis, psoriatic arthritis, Reiter’s disease, the intestinal arthropathies, and Behçet’s syndrome. Medicine 53(5):343–463
Dougados M, Van der Linden SR et al (1991) The European Spondyloarthropathy Study Group: the European Spondyloarthropathy Study Group preliminary criteria for the classification of spondyloarthropathy. Arthritis Rheum 34:1218–1227
Braun J, Bollow M, Remlinger G et al (1998) Prevalence of spondyloarthropathies in HLA-B27 positive and negative blood donors. Arthritis Rheum 41(1):58–67
Orchard TR, Wordsworth BP, Jewell DP (1998) Peripheral arthropathies in inflammatory bowel disease: their articular distribution and natural history. Gut 42(3):387–391
Smale S, Natt RS, Orchard TR, Russell AS, Bjarnason I (2001) Inflammatory bowel disease and spondyloarthropathy. Arthritis Rheum 44:2728–2736
Veloso FT, Carvalho J, Magro F (1996) Immune-related systemic manifestations of inflammatory bowel disease. A prospective study of 792 patients. J Clin Gastroenterol 23(1):29–34
Holden W, Orchard T, Wordsworth P (2003) Enteropathic arthritis. Rheum Dis Clin North Am 29:513–530
Haslock I, Wright V (1973) The musculo-esqueletal complications of Crohn’s disease. Medicine 52(3):217–225
Dekker-Saeys BJ, Meuwiessen SGM, Van der Bergen-Loonen EM et al (1978) Prevalence of peripheral arthritis, sacroiliitis and ankylosing spondylitis in patients suffering from inflammatory bowel disease. Ann Rheum Dis 37:33–35
Münch H, Purrmann J, Reis HE et al (1986) Clinical features of inflammatory joint and spine manifestations in Crohn’s disease. Hepatogastroenterology 33:123–127
Danzi JT (1988) Extraintestinal manifestations of idiopathic inflammatory bowel disease. Arch Intern Med 148:297–302
Scarpa R, Del Puente A, D’Arienzo A et al (1992) The arthritis of ulcerative colitis: clinical and genetics aspects. J Rheumatol 19(3):373–376
Maeda K, Okada M, Yao T et al (1994) Intestinal and extraintestinal complications of Crohn’s disease: predictors and cumulative probability of complications. J Gastroenterol 29:577–582
Mielants H, De Vos M, Cuvelier C, Veys EM (1996) The role of gut inflammation in the pathogenesis of spondyloarthropathies. Acta Clin Belg 51(5):340–349
Triantafillidis JK, Emmanouilidis A, Manousos O et al (2000) Clinical patterns of Crohn’s disease in Greece: a follow-up study of 155 cases. Digestion 61:121–128
Salvarani C, Vlachonikolis IG, Van der Heidje DM et al (2001) Musculoskeletal manifestations in a population-based cohort of inflammatory bowel disease patients. Scand J Gastroenterol 12:1307–1313
De Vlam K, Mielants H, Cuvelier C et al (2000) Spondyloarthropathy is underestimated in inflammatory bowel disease: prevalence and HLA association. J Rheumatol 27(12):2860–2865
Palm O, Moum B, Ongre A, Gran JT (2002) Prevalence of ankylosing spondylitis and other spondyloarthropathies among patients with inflammatory bowel disease: a population study (the IBSEN Study). J Rheumatol 29(3):511–515
Christodoulou DK, Katsanos KH, Kitsanou M et al (2002) Frequency of extraintestinal manifestations in patients with inflammatory bowel disease in northwest Greece and review of the literature. Dig Liver Dis 34(11):781–786
Goldfarb M, Leite N, Rubistein J et al (1985) Manifestações reumáticas na retocolite ulcerativa idiopática. Estudo de 98 casos no HSE e revisão da literatura. Rev Bras Reumatol 25(2):53–56
Sands BE (2002) Crohn’s disease. In: Feldman M, Friedman LS, Sleisenger MH (eds) Gastrointestinal and liver disease pathophysiology diagnosis/management. 7th edn. Saunders, Philadelphia, pp 2005–2038
Jewell DP (2002) Ulcerative colitis. In: Feldman M, Friedman LS, Sleisenger MH (eds) Gastrointestinal and liver disease pathophysiology diagnosis/management. 7th edn. Saunders, Philadelphia, pp 2039–2067
Gasche C, Scholmerich J, Brynskov J et al (2000) A simple classification of Crohn’s disease: report of the working party of the World Congress of Gastroenterology, Vienna 1998. Inflamm Bowel Dis 6(1):8–15
Farmer RG (1987) Nonspecific ulcerative proctitis. Gastroenterol Clin North Am 16:154–174
Calin A, Porta J, Fries JF, Schurman DJ (1977) Clinical history as a screening test for ankylosing spondylitis. JAMA 237(24):2613–2614
Van der Linden S (2001) Ankylosing spondylitis. In: Kelley WN, Harris ED, Rudy S, Sledge CB (eds) Textbook of rheumatology. 5th edn. Saunders, Philadelphia, pp 1039–1069
Van der Linden S, Valkenburg HA, Cats A (1984) Evaluation of diagnostic criteria for ankylosing spondylitis: a proposal for modification of the New York criteria. Arthritis Rheum 27:361–368
Bernstein CN, Blanchard JF, Rawsthorne P, Yu N (2001) the prevalence of extraintestinal diseases in inflammatory bowel disease: a population-based study. Am J Gastroenterol 96(4):1116–1121
Mielants H, Veys EM, Cuvelier C et al (1995) The evolution of spondyloarthropathies in relation to gut histology: III relation between gut and joint. J Rheumatol 22(12):2279–2284
De Keyser F, Elewaut D, De Vos M et al (1998) Bowel inflammation and spondyloarthropathies. Rheum Dis Clin North Am 24(4):785–812
Edmunds L, Elswood J, Kennedy LG, Calin A (1991) Primary ankylosing spondylitis, psoriatic and entheropathic spondyloarthropathy: a controlled analysis. J Rheumatol 18(5):696–698
Dekker-Saeys BJ, Meuwiessen SGM, Van der Bergen-Loonen EM et al (1978) Clinical characteristics and results of histocompatibility typing (HLA B27) in 50 patients with both ankylosing spondylitis and inflammatory bowel disease. Ann Rheum Dis 37:36–41
Ferreira E, Ward FE, Amos DB (1975) HL-A in a Brazilian population: evidence for new HL-A specificities. In: Kissmeyer-Nielsen G (ed) Histocompatibility testing. Munksgaard, Copenhagen
Moraes HV Jr (1996) Uveíte anterior aguda e HLA-B27: valor diagnóstico e prognóstico. Rev Bras Oftalmol 55:53–62
Salmon JF, Wright JP, Murray AD (1991) Ocular inflammation in Crohn’s disease. Ophthalmology 98:480–484
Lyons JL, Rosenbaun JT (1997) Uveitis associated with inflammatory bowel disease compared with uveitis associated with spondyloarthropathy. Arch Ophthalmol 115(1):61–64
Pato E, Bañares A, Jover JÁ et al (2000) Undiagnosed spondyloarthropathy in patients presenting with anterior uveitis. J Rheumatol 27(9):2198–2202
Rosenbaun JT (1989) Characterization of uveitis associated with spondyloarthritis. J Rheumatol 16(6):792–796
Linssen A, Meenken C (1995) Outcomes of HLA B27-positive and HLA B27-negative acute anterior uveitis. Am J Ophthalmol 120:351–361
Carvalho MAP, Campos WR, Araujo CAA et al (1999) Uveítes anteriores não granulomatosas, espondiloartropatias e HLA B27. Rev Bras Reumatol 39(4):195–202
Acknowledgments
The authors wish to thank Dr. Percival Degrava Sampaio-Barros for his aid in the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lanna, C.C.D., Ferrari, M.d.L.A., Rocha, S.L. et al. A cross-sectional study of 130 Brazilian patients with Crohn’s disease and ulcerative colitis: analysis of articular and ophthalmologic manifestations. Clin Rheumatol 27, 503–509 (2008). https://doi.org/10.1007/s10067-007-0797-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-007-0797-5