Abstract
We analysed the impact of fibromyalgia (FM) on the functional capacity of patients suffering this syndrome and identified factors that are associated with greater disease impact. We performed a cross-sectional descriptive telephone survey on all patients diagnosed with fibromyalgia during 2003 in a university hospital in Spain. Variables studied were socio-demographic, job, clinical, health and psycho-social characteristics of patients diagnosed with FM and impact of FM on them. Disease impact was measured by means of the Fibromyalgia Impact Questionnaire (FIQ). The rest of variables were collected by means of an expressly designed questionnaire. The relation between FIQ score and the other variables was performed with a bivariate analysis, using several tests depending on the variables involved. To analyse the factors associated with greatest disease impact, a multivariate linear regression model was designed. The average FIQ score for the sample was 63.6. Having a larger number of children, being tired and being in a depressed mood were the symptoms that most affected activities of daily living. A diagnosis of any mental illness, reference to repercussion on the family environment, a lower self-rated health and having consulted more specialists before FM diagnosis were associated with a higher impact after adjusting according to all the variables in the model. It can be confirmed that the FIQ is a useful instrument for measuring the impact of FM on quality of life. Identifying factors that determine the extent of its impact will enable more effective therapeutic strategies to be designed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fibromyalgia (FM) is a chronic non-articular rheumatic disease of unknown aetiology. It is characterised by diffuse musculoskeletal pain, sleep disorder, fatigue and the presence of multiple tender points. The American College of Rheumatology (ACR) defined the diagnostic criteria of FM in 1990 [1]. In 1992, fibromyalgia was recognised by the World Health Organisation as a disease, and it was classified in the International Classification of Diseases (ICD-10) as code M79.03 [2]. Then, in 1994, the International Association for the Study of Pain (IASP) recognised FM as a disease and classified it as code X33.X8a.
The syndrome is highly prevalent, but despite this, there is very little information on its epidemiological characteristics. Some studies have estimated its prevalence in different populations. The pioneer study conducted by Wolfe et al in 1995 [3] estimated a 2% prevalence amongst the general population in the USA. Using a different methodology, prevalence was estimated at 3.3% in Canada [4] A higher prevalence is always found in women than in men. In Spain, prevalence has been estimated at between 1 and 4% [5, 6]. Specifically, the EPISER study found a 2.37% prevalence in the general population in Spain, with a women/men ratio of 21:1 (4.2/0.2%) [7, 8].
There is great controversy surrounding the syndrome and its therapeutic approach, and this is mainly due to lack of knowledge regarding its aetiology [9–12], its diverse clinical manifestations [13–15] and the presence of an associated psychiatric component [16–19], although it has been demonstrated that FM patients complain of greater disability than patients with other chronic pain disorders do [10, 20].
However, in the same way that little is known about the factors that intervene in its aetiology, little is also known about the impact of the disease, measured in terms of a patient’s altered functional capacity [21]. Different instruments have been used to assess functional disability and health status in FM patients, and the most common approach is to use a combination of the Short Form Health Survey (SF-36) and the Fibromyalgia Impact Questionnaire (FIQ) [22]. The FIQ is a specific questionnaire for FM, which was developed at the end of the 1980s [25, 26]. In the last few years, it has become the most commonly used measurement instrument to assess these patients. Its most notable advantages are that it is short, easy to use and score and it is sensitive to changes in a patient’s condition [27, 28]. In this paper, we will use the version validated by De Gracia et al. [29] in a Spanish population, which has shown operating characteristics similar to the English version.
The objective of this study is to analyse the impact of FM on the functional capacity of patients suffering this syndrome and to identify factors that are associated with greater disease impact.
Materials and methods
Patients
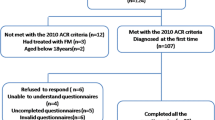
A cross-sectional, descriptive telephone survey was conducted during June, July and August 2004 on all patients diagnosed with FM during 2003 (in accordance with ACR criteria) at three offices in the rheumatology department of a university hospital Virgen de las Nieves (Granada, Spain). Patients were excluded if they were physically or mentally unable to respond to the telephone questionnaire and if they had suffered health problems apart from their FM that limited their normal activities of daily living during the week preceding the interview.
Variables studied and measuring instruments
-
FM impact, defined as alteration in the functional capacity of patients diagnosed with this disease.
-
Socio-demographic characteristics: sex, normal place of residence (urban/rural environment), marital status, employment status (working/not working), monthly household income (low = <900 €/medium = 900–1,200 €/high = >1,200 €), educational level (illiterate, low = no basic education/medium = primary education or vocational training/high = higher education), age and number of children. The categories in some variables were grouped according to analysis needs.
-
Job characteristics, present job situation (paid job/unpaid job/does not work), present type of job in the case of working persons (works at home/ manual work/non-manual work), present employment status (off-work/at work).
-
Clinical characteristics, initial symptom(s) of the disease, symptom(s) that most limit(s) activities of daily living, presence of associated illnesses (yes/no) and self-rated health (Likert type scale: very good/good/fair/poor/very poor).
-
Health characteristics: time from onset of symptoms to disease diagnosis, number of specialists consulted before and after FM diagnosis, current pharmacological and/or alternative FM treatment (and type of treatment where appropriate) and consultations with doctor since diagnosis.
-
Psycho-social characteristics: family and personal history of mental illness, current mental illnessFootnote 1 diagnosed by a doctor, occurrence of traumatic events during patient’s life, social support and type of support, repercussion of FM on the family environment and type of repercussion.
To collect this information, a questionnaire was expressly designed for this study. It consisted of 38 questions, 22 of which were open and 16 were closed. The questions were based on previous studies and were intended to be clear and concise to increase reliability.
Disease impact was measured by means of the FIQ. The FIQ is designed to assess and evaluate the health status of FM patients, their progress and results, using health status components that are most affected by FM. The questionnaire consists of a total of ten questions on activities of daily living, with a possible score of 0 to 10 for each one. The maximum score is 100, which corresponds to greatest disease impact. An average FM patient usually obtains a score of 50, and patients with a score of more than 70 are considered to be severely affected cases. Internal consistency α 0.93 and explained variance 81.36%. The FIQ contains questions on the patient’s ability to carry out certain tasks during the past week, which is why patients were excluded from the study if they had other health problems apart from FM that could limit their normal activities of daily living during the week before the interview.
Before the study was commenced, a pilot study was performed with several subjects who had been diagnosed with FM in 2002 (n = 15). Thus, it was possible to identify ambiguous aspects and some questions that were difficult for patients to understand. It also served to train the interviewers.
Statistical analysis
The relation between the FIQ score and the other variables was performed with a bivariate analysis, using contingency tables and the chi-square test, Student’s t test, analysis of variance (ANOVA), and non-parametric tests such as the Mann–Whitney and Kruskal–Wallis tests, depending on the variables involved.
To analyse the factors that were associated with greatest disease impact, a multivariate linear regression model was designed, where the dependent variable was the FIQ, and the independent variables were those that were significant in the bivariate analysis and others that were of interest for this study. Co-linearity between variables was verified with tolerance values. In all cases, statistical significance was defined as 5%.
Results
Two hundred and fifty-eight patients were identified, and information was finally collected on 214 of them (197 women and 17 men), representing a 82.95% response rate (18.69% could not be located and 1.64% did not wish to participate). All patients who agreed to participate in the study were guaranteed that data would be treated in confidence. The sociodemographic characteristics of the sample are shown in Table 1.
The average FIQ score for the sample was 63.6, and the score was lower in women (63.17) than in men (68.56), although this was not a statistically significant difference (p = 0.09). FM had a higher impact on patients with a low educational level, larger number of children and older age, and this difference was statistically significant (p < 0.05; Table 1).
With regard to job characteristics, FM had a greater impact on patients with unpaid jobs and those who did not work than in those with paid jobs. It also had a greater impact on patients who worked at home than in those with other types of jobs. Patients who were off-work also obtained a higher FIQ score, although the difference observed was not significant in any of these cases (Table 2).
FM had a greater impact on patients with initial symptoms of tiredness and paraesthesia than on those with bone and joint pain (p < 0.01). Similarly, patients who complained that tiredness and depressed mood were the symptoms that most affected their daily life (p < 0.01) and those that had a poor perception of their health had higher FIQ scores (p < 0.01). The impact was also greater on patients with comorbidity, although this case did not show a statistically significant difference (Table 3).
Patients who were on pharmacological treatment at the time of the questionnaire obtained a higher FIQ score than those who were not on pharmacological treatment (p < 0.01). Patients who were taking γ-aminobutyric acid (GABA) presented a higher impact (p < 0.01). To the contrary, patients treated with alternative methods presented a lower impact than those who were not receiving alternative treatment, and those who took physical exercise had a lower score than those who attended physiotherapy and rehabilitation or received alternative therapies (p = 0.02). Patients who had consulted a doctor after diagnosis had a higher score than those who did not, although this was not a significant difference (p = 0.09). Patients who consulted more specialists before diagnosis obtained a higher FIQ score (p < 0.01; Table 4).
With regard to the association between psycho-social characteristics and disease impact, it was observed that patients who presented psychiatric disorders at the time of the interview (p < 0.01), those who had been diagnosed with a mental illness at some time in their life (p < 0.01), those who had suffered traumatic events (p = 0.03), lacked social support (p < 0.01) or found that FM had a repercussion on their family environment (p < 0.01) had a higher FIQ score. There was a lower impact on patients who had family support than those who had support from friends or their partner. The greatest FM impact with regard to repercussion on the patient’s environment was found in exhaustion on the part of family members, followed by problems with partners, reduced social life and dependence on family, although these differences were not statistically significant (Table 5).
Finally, the multivariate analysis revealed that having a larger number of children, being tired and being in a depressed mood were the symptoms that most affected activities of daily living; a diagnosis of any mental illness, reference to repercussion on the family environment, a lower self-rated health, and having consulted more specialists before FM diagnosis were associated with a higher impact after adjusting according to all the variables in the model (Table 6). The model obtained explains 58.7% of variability in the degree of disease impact.
Discussion
FM is a chronic disease. Although it does not cause injuries or deformed joints, it does alter the patient’s functional capacity, and it may lead to considerable difficulties in carrying out activities of daily living. These difficulties may be even greater than those experienced by patients who suffer chronic pain from other diseases [10, 20, 27, 30, 31].
In recent years, there has been greater interest in analysing the relation between quality of life and FM patients’ health, although to date the study of factors associated with greater disease impact in these patients has hardly been addressed. The little evidence that is available indicates that the presence of a large number of symptoms, self-perception of a poor quality of life, the number of tender points and a high education level are highlighted as aspects that are associated with a higher FIQ score [32].
The average score obtained in the FIQ in this study was 63.6. This is higher than previous studies in which scores range from 43.2 to 61.3 [31, 33–35]. In our study, 41.6% of interviewees presented moderate to severe disease impact (values greater than 70).
The socio-demographic characteristics associated with greater disease impact are number of children, age and low educational level. There are two possible explanations. The first could be that patients with higher socio-economics level are associated with quality of life and coping skills. Secondly, it seems logical for the impact to be lower in patients with a higher educational level, as they have more resources for coping with the disease.
Clinical manifestations associated with greater disease impact are tiredness and depressed mood, and these come before pain, which is the most characteristic symptom of FM. The literature states that patients with fibromyalgia have a limited serotonin production rate, which could explain this characteristic symptomatology [36, 37]. Thus, when treating FM, it should be applied a broad therapeutic approach, taking into account non-physical symptoms that are related to the effects that the difficulties in the diagnosis of FM has on patients, such as reduced self-esteem, frustration and anxiety. This may be due to the larger number of recourses that are available now to alleviate pain in comparison with the other two symptoms.
Furthermore, coinciding with evidence available on FM patients’ lower quality of life in comparison with other patients with rheumatoid diseases [38], a reduced self-rated health is associated with a high FIQ score in this study.
Access to the health service and use of available resources are also related to FM impact; thus, there is a lower FM impact when more specialists are consulted. In this respect, some authors have found that one of the possible reasons for under-diagnosing all pathologies related to chronic pain is the patients’ lack of access to or use of the health system [39].
It is remarkable that there is greater FM impact in patients who are on pharmacological treatment than in those who are not. The therapeutic complexity inherent to FM treatment, with its multiple symptoms and drug interactions, may explain this apparent contradiction. Furthermore, patients receiving alternative treatment obtained a lower FIQ score than those who did not, although this was not a significant difference. This finding coincides with recent results on the beneficial effects of these alternative therapies [40, 41].
Finally, one of the issues that is subject to great debate in FM is its relation with psychological and psychiatric disorders. There was a 50% presence of a personal history of mental illness in this study; however, at the time of the questionnaire, current mental illness had fallen to 36.4%, which is similar to data obtained in previous studies and in other chronic pathologies [25, 42]. Possibly, when patients know that they are suffering a disease called fibromyalgia, the anxiety caused by their prior uncertainty returns to normal levels, which is verbalised by study patients as follows, “I felt better when I knew that I wasn’t inventing it.”
When analysing the above results, variability in the interpretation of diagnostic criteria should be taken into account because this often leads to under or over-diagnosis of the disease [17, 43, 44]. Furthermore, in view of the cross-sectional design of this study, interrelations can be observed between factors studied, but no causal relations can be established from this data. Bias from case losses (patients who could not be located and those who did not wish to answer the questions) was not relevant, considering the high response rate attained.
It can be confirmed that the FIQ is a useful instrument for measuring the impact of FM on quality of life. Identifying factors that determine the extent of its impact will enable more effective therapeutic strategies to be designed.
Notes
Mental illness is considered as any type of mental disorder (depression, anxiety, somatisation, phobias, etc.).
References
Wolfe F, Smythe HA, Yunnus MB et al (1990) The American College of Rheumatology (1990) criteria for the classification of fibromyalgia. Arthritis Rheum 33:160–172
WHO (1992) International statistical classification of diseases and related problems. ICD-10. WHO, Geneva
Wolfe F, Ross K, Anderson J et al (1995) The prevalence and characteristics of Fibromyalgia in the general population. Arthritis Rheum 38:19–28
White KP, Speechley M, Harth M et al (1999) The London Fibromyalgia Epidemiology Study: the prevalence of fibromyalgia syndrome in London, Ontario. J Rheumatol 26:1570–1576
Ballina FJ, Martín P, Iglesias A et al (1995) La fibromialgia. Revisión clínica. Rev Clin Esp 195:326–331
Mulero J (1997) Fibromialgia. Medicine 7:2682–2687
Valverde M, Juan A, Rivas B et al (2001) Fibromialgia. En: Estudio EPISER. Prevalencia e impacto de las enfermedades reumáticas en la población adulta española. Madrid: Msd y Sociedad Española de Reumatología 77–91
Ubago MC, Ruiz I, Bermejo MJ et al (2005) Características clínicas y psicosociales de personas con fibromialgia. Repercusión del diagnóstico sobre sus actividades. Rev Esp Salud Publica 79:683–695
Arnold LM, Keck PE, Welge JA (2000) Antidepressant treatment of fibromyalgia. A metaanalysis and review. Psychosomatics 41:104–13
Fernández MA (2000) Fibromialgia. Rev Esp Reumatol 27:442–446
Schochat T, Beckmann C (2003) Sociodemographic characteristics, risk factors and reproduced history in subjets whith fibromyalgia. Results of a population based case-control study. Z Rheumatol 62:46–59
Patkar AA, Biloll, Masand PS (2003) Management of fibromyalgia. Curr Psychiatry Rep 5:218–224
Wolfe F (1996) The fibromyalgia syndrome: a consensus report on fibromyalgia and disability. J Rheumatol 23:534–539
Wolfe F (1997) The relation between tender points and fibromyalgia symptom variables: evidence that fibromyalgia is not a discrete disorder in the clinic. Ann Rheum Dis 56:268–271
Fitzcharles MA, Esdaile JM (1997) The overdiagnosis of fibromyalgia syndrome. Am J Med 103:44–50
Edwards, Bingham C III, Bathon et al (2006) Catastrophizing and pain in arthritis, fibromyalgia, and other rheumatic diseases. Arthritis Care Research 55:325–332
Okifuji A, Turk DC, Sherman JJ (2000) Evaluation of the relation-ship between depression and fibromyalgia syndrome: why aren’t all patients depressed? J Rheumatol 27:212–219
Beth JM (2002) Does chronic pain predict future psychological distress? Pain 96:239–245
Suhr JA (2003) Neuropsychological impairment in fibromyalgia: relation to depression, fatigue and pain. J Psychosom Res 55:321–329
Martínez E, González O, Crespo JM (2003) Fibromialgia: definición, aspectos clínicos, psicológicos, psiquiátricos y terapéuticos. Salud Mental 4:2–7
Forseth KO, Husby G, Gran JT et al (1999) Prognostic Factors for the development of fibromyalgia in women with self-reported musculoskeletal pain. A prospective study. J Rheumatol 26:2458–2467
Rivera J, Alegre C, Ballina FJ et al (2006) Documento de consenso de la Sociedad Española de Reumatología sobre la fibromialgia. Reumatol Clin 2(Supl 1):S55–S66
Ware JE, Sherbourne CD (1992) The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 30:473–483
Alonso J, Prieto L, Antó JM (1995) La versión española del SF-36 Health Survey (Cuestionario de salud SF-36): un instrumento para la medida de los resultados clínicos. Med Clin (Barc) 104:771–776
Burckardt CS, Clark SR, Bennet RM (1991) The fibromyalgia impact questionnaire: development and validation. J Rheumatol 18:728–733
Bennet R (2005) The Fibromyalgia Impact Questionnaire (FIQ): a review of its development, current version, operating characteristics and uses. Clin Exp Rheumatol 23(Suppl 39):154–162
Rivera J, González T (2004) The Fibromyalgia Impact Questionnaire: a validated Spanish version to assess the health status in women with fibromyalgia. Clin Exp Rheumatol 22:554–560
Esteve-Vives J, Batlle-gualda E, Reig A (1993) Spanish version of the health assessment questionnaire: reliability, validity and transcultural equivalency. Grupo para la adaptación del HAQ a la población española. J Rheumatol 20:2216–2222
De Gracia M, Marco M, Ruiz J (2001) Evaluación de los aspectos psicológicos de la Fibromialgia. Anl Modif Conduct 21:959–980
Boonen A, van den Heuvel R, van Tubergen A et al (2005) Large differences in cost-of-illness and well being between patients with fibromyalgia, chronic low back pain or ankylosing spondylitis. Ann Rheum Dis 64:396–402
Dönmez A, Zeki Karagülle M, Tercan N et al (2005) SPA therapy in fibromyalgia: a randomised controlled clinic study. Rheumatol Int 26:168–172
Fallon J, Bujak DI, Guardino S et al (1999) The Fibromyalgia Impact Questionnaire: a useful tool in evaluating patients with post-Lyme disease syndrome. Arthritis Care Res 12:42–47
White K, Speechley M, Harth M et al (1999) Comparing self-reported function and work disability in 100 community cases of fibromyalgia syndrome versus controls in London (Ontario). Arthritis Rheum 42:76–83
Gowans SE, Dehueck A, Voss S et al (2004) Six-month and one-year follow up of 23 weeks of aerobic exercise for individuals with fibromyalgia. Arthritis Rheum 51:890–898
Zijlstra TR, van de Laar MA, Bernelot HJ et al (2005) Spa treatment for primary fibromyalgia syndrome: a combination of thalassotherapy, exercise and patient education improves symptoms and quality of life. Rheumatology 44:539–546
Yunus MB (1992) Plasma tryptophan and other amino acids in primary fibromyalgia: a controlled study. J Rheumatol 19:90–94
Bazzichi L, Giannaccini G, Betti L et al (2006) Alteration of serotonin transporter density and activity in fibromyalgia. Arthritis Res Ther 8:99
Birtane M, Uzunca K, Tastekin N et al (2007) The evaluation of quality of life in fibromyalgia syndrome: a comparison with rheumatoid arthritis by using SF-36 Health Survey. Clin Rheumatol 26:679–684
Salomon L, Reeves W (2004) Factors influencing the diagnosis of chronic fatigue syndrome. Arch Intern Med 164:2241–2245
Martin DP, Sletten CD, Williams BA et al (2006) Improvement in fibromyalgia symptoms with acupuncture: results of a randomized controlled trial. Mayo Clin Proc 81:749–757
Assis MR, Silva LE, Alves M et al (2006) A randomized controlled trial of deep water running: clinical effectiveness of aquatic exercise to treat fibromyalgia. Arthritis Rheum 55:57–65
Culos-Reed S, Brawley L (2000) Fibromyalgia, physical activity, and daily functioning: the importance of efficacy and health-related quality of life. Arthritis Care Res 13:343–351
Croft P (1994) Population study of tender points counts and pain as evidence of fibromyalgia. BMJ 309:696–699
O’Malley P (2000) Treatment of fibromyalgia with antidepressants: a meta-analysis. J Gen Inter Medicine 15:659–666
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ubago Linares, M.d.C., Ruiz-Pérez, I., Bermejo Pérez, M.J. et al. Analysis of the impact of fibromyalgia on quality of life: associated factors. Clin Rheumatol 27, 613–619 (2008). https://doi.org/10.1007/s10067-007-0756-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-007-0756-1