Abstract
The Bath Ankylosing Spondylitis Disease Activity Index (BASDAI), Bath Ankylosing Spondylitis Functional Index (BASFI), and Bath Ankylosing Spondylitis Global Score (BAS-G) have been recommended for evaluating function and disability in patients with ankylosing spondylitis (AS). The aim of this study was to develop a Chinese version of the BASDAI, BASFI, and BAS-G and assess their reliability and validity. The Chinese version was obtained after a translation and back-translation process. A total of 447 patients with adult and juvenile AS were assessed using these three instruments. Reliability was tested by internal consistency and test–retest reliability. Internal consistency of the instrument was given as Cronbach’s alpha. Test–retest reliability was assessed by intraclass correlation coefficient. To assess the sensitivity to change, 153 patients were included in an 8-week follow-up study. In our analysis, the reliability of these three instruments—the BASDAI, BASFI, and BAS-G—for a 24-h test–retest showed acceptable intraclass correlation coefficients (0.92–0.94). Our Chinese versions of the BASDAI, BASFI, and BAS-G also showed 0.87, 0.94, and 0.90, respectively, with Cronbach’s alpha coefficient, indicating good reliability. For sensitivity to change in 8-week follow-up, all three instruments showed 5.0 to 5.4% changes. Our Chinese versions of the BASDAI, BASFI, and BAS-G showed adequate reliability, validity, and responsiveness to clinical change. Thus, disease activity and functional status in Chinese-speaking patients with AS may be adequately evaluated with these versions of the original instruments.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ankylosing spondylitis (AS) is a seronegative spondyloarthropathy characterized by inflammation and radiographic changes, mainly localized to the spinal column. Therapies are aimed at reducing inflammatory responses, spinal stiffness, and pain [1, 2]. Previous epidemiological studies have revealed that AS occurs predominantly in Caucasians and a small number of native American tribes [3]. The incidence of AS in Japan and Africa is considerably lower [4–6], whereas the prevalence of AS in the Taiwanese population is about 0.2 to 0.3%, similar to that in Caucasians [7, 8].
Furthermore, some patients with AS have juvenile onset disease (JAS), defined by onset at or before age 16 years. Characteristic clinical features distinguish JAS from adult onset disease (AAS) as follows: Patients with JAS have a higher frequency of extraspinal joint disease, whereas those with AAS have increased frequencies of radiographic abnormalities of the spine [9]. Persistent hip, knee, and ankle arthritis and dactylitis of the hands occur more frequently in juveniles [10]. Peripheral joint involvement as a mono- or oligoarthritis is significantly more frequent in juvenile onset patients, not only as a mode of onset but also during the course of the disease. Impairment of functional capacity is more severe in the juvenile onset group, and hip joint involvement is closely related to a poorer prognosis [11].
No gold standard exists for measuring disease activity in AS. Limited spinal mobility is a cardinal sign of AS. The assessment of spinal mobility assists in identifying patient sub-groups and predicts clinical outcome in AS [12, 13]. Consequently, the Assessment in AS international group (ASAS) has recommended spinal mobility as a core domain in the evaluation of patients in both clinical practice and trials [14], confirming its use in routine practice [15]. In addition, fatigue is reported to be a common complaint among patients with AS [16–18]. Previous studies have shown that fatigue in AS patients is associated with limitations in daily life functioning [16, 17], pain and stiffness [17], as well as with global well-being and mental health [19]. Therefore, many valid instruments have been developed to evaluate function and disability in recent years, such as the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) [20] and the Bath Ankylosing Spondylitis Functional Index (BASFI) [16]. In addition, a more global assessment is also desirable, and validation of a global measure by the Bath Ankylosing Spondylitis Global Score (BAS-G) was established to reflect the effect of AS on patients’ well-being [21]. These questionnaires can be completed quickly and easily and have good reproducibility, validity, and sensitivity to clinical change. The questionnaires also include the entire spectrum of AS symptoms related to fatigue, pain, swelling, and morning stiffness [20].
These instruments have been translated into several languages and have now been developed in Chinese. However, it remains unclear whether the index is an accurate expression of the component parts. Especially, it has not been determined whether there is a differential expression between JAS and AAS patients when evaluating them with established questionnaires such as the BASDAI, BASFI, and BAS-G. Therefore, this study aimed to translate the previously developed BASDAI, BASFI, and BAS-G to Chinese language and evaluate the reliability and validity of the translated versions among a sample of Taiwanese JAS and AAS patients.
Materials and methods
Developing the Chinese version of the BASDAI, BASFI, and BAS-G
The original versions of the BASDAI, BASFI, and BAS-G were obtained from Garrett et al. [20], Calin et al. [16], and Jones et al. [21], respectively. The BASDAI is a six-item self-administered questionnaire that measures symptoms such as fatigue, spinal pain, pain and/or swelling of the peripheral joints, localized tenderness, and morning stiffness during the last week. It also measures the severity and duration of morning stiffness (0 to 2 or more hours). The first five items are answered on 0-to-100-mm, unmarked, horizontal visual analogue scales (VAS) with “none” anchored at one extreme and “very severe” at the other. The scale for degree of morning stiffness is graded every 15 min between 0 and 2 h. The BASFI is also a self-administered questionnaire that measures the ability of the individual to perform ten items of daily living activities. Each item is answered on 0-to-100-mm VAS ranging from “easy” at one end to “impossible” at the other. The BAS-G is composed of two VAS (0 to 100 mm) with the end words “none” and “very severe.” The patients estimate the influence of the disease on their well-being over the previous week and the previous 6 months.
One professional translator and two bilingual physicians who were familiar with the medical aspects of AS translated the original version of BASDAI, BASFI, and BAS-G to Chinese then back to English (back-translation). They were unaware of the original version. Our researchers then examined discrepancies between (1) the original English version, (2) the initial Chinese version, and (3) the back-translated English version. Furthermore, we also decided on the most appropriate translation of each item and were resolved to develop a Chinese version that was linguistically and conceptually equivalent. A modified Chinese version was developed after a series of meetings. The modified Chinese versions of BASDAI, BASFI, and BAS-G were pilot tested with AS patients. Patients took an average of 10 min to complete the scale and demonstrated no difficulty in understanding and responding to the items of the scale. As a result, the pilot study did not lead to any changes to the final Chinese version of BASDAI, BASFI, and BAS-G.
Study subjects and data collection
Subsequently, for investigation of the reliability, validity, and sensitivity of the Chinese versions of BASDAI, BASFI, and BAS-G, our modified Chinese versions of the three instruments were administered to Taiwanese patients with AS for the purpose of validation. Sequential patients who were attending their follow-up appointments at the clinic at Chung Shan Medical University Hospital in Taichung, Taiwan from November 2002 to May 2004, and who met the selection criteria, were asked to participate in the study. Informed consent was obtained before any data were collected from the respondents. Four selection criteria were used to recruit subjects: (1) patients aged 18–65 years; (2) being diagnosed according to the modified New York criteria [22]; (3) Chinese language speakers (90% of Taiwanese speak Chinese, some speak one of the Chinese dialects, such as Fukienese; all dialects share the same writing system) without language problems; and (4) cognitive performance not being influenced by other diseases, e.g., dementia. A total of 447 patients with AS were included in our study. JAS was defined when joint symptoms occurred at or before age 16, and AAS was defined as occurring after age 16.
To ensure the privacy and convenience of respondents, the questionnaire was administrated in an interview room within the clinic. To avoid bias arising from social desirability in the data provided, at the beginning of the questionnaire administration, our researchers read a standardized statement to each respondent explaining the confidentiality and anonymity of data collected.
Additionally, test–retest reliability was further assessed in a random subset of 41 patients using the first and second questionnaire administration (24 h apart). Forty-one patients completed questionnaires on disease activity (BASDAI), functional ability (BASFI), and global well-being (BAS-G).
Statistical methods
SAS 9.1 for Windows was used for the statistical analyses. Comparisons among JAS and AAS groups for age at recruitment, erythrocyte sedimentation rate, C-reactive protein, occiput-wall distance, Schober test, chest expansion, and BASDAI, BASFI, and BAS-G were made using Student’s t test for continuous variables and the χ 2 test for discrete variables. Reliability of our Chinese versions of the BASDI, BASFI, and BAS-G was tested by internal consistency and test–retest reliability. Internal consistency of the instrument was given as Cronbach’s alpha. Internal reliability analyses (Cronbach’s alpha) were performed on scaled responses to multiple items (e.g., six items from BASDAI, ten items from BASFI, and two items from BAS-G). Test–retest reliability was assessed by intraclass correlation coefficient (ICC). Correlations between BASDAI, BASFI, and BAS-G with laboratory and clinical assessments were also evaluated with Spearman’s rank correlation coefficient. Significance was set at p < 0.05.
Results
One hundred and eighteen (26.4%) patients were enrolled in the JAS group and 329 (73.6%) in the AAS group (Table 1). Median age at onset of JAS was 11.2 years (range 5.3–15.9) and of AAS 30.4 years (range 16.2–72.4). No significant difference was found between the two groups in gender distribution (p = 0.45, χ 2 test). Duration of symptoms was 15.2 ± 6.9 (SD) years in the JAS group and 7.1 ± 6.0 years in AAS (p = 0.054, t test). Duration of spinal symptoms was 8.7 ± 6.1 years in JAS and 4.4 ± 5.1 years in AAS (p = 0.02). Laboratory studies including erythrocyte sedimentation rate (p < 0.001) and C-reactive protein (p < 0.001) were significantly different between the JAS and AAS groups. The AAS group had significantly higher level of erythrocyte sedimentation and lower level of C-reactive protein than the JAS group.
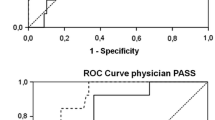
Results on the BASDAI, BASFI, and BAS-G indices for AS patients are shown in Table 2. The coefficient of internal consistency (Cronbach’s alpha) for BASDAI was 0.87, for BASFI 0.94, and for BAS-G 0.90. Additionally, test–retest reliability was further assessed in a random subset of 41 patients who self-reported that they did not experience major changes in symptoms within the 2-week period after the first administration of the questionnaires. The ICC of BASDAI, BASFI, and BAS-G also showed good reproducibility of results, ranging from 0.92 to 0.94. When comparing the scores of BASDAI (4.1 vs 3.9, p = 0.94), BASFI (2.5 vs 1.9, p = 0.22), and BAS-G (4.5 vs 3.9, p = 0.22), higher scores of BASDAI, BASFI, and BAS-G were observed in the JAS group than those in the AAS group; however, there was no significant difference in those scores between patient groups.
Furthermore, in all AS patients, significant correlations were detected between BASDAI, BASFI, and BAS-G (Table 3). Similarly, significant correlations were also detected between the BASFI and the BAS-G. We especially observed a negative correlation between BASDAI, BASFI, and BAS-G scores with age at onset, especially in AAS patients, but not in JAS patients. Both the duration of symptoms and duration from diagnosis also correlated positively with BASDAI, BASFI, and BAS-G scores in AAS patients, but not in JAS patients. However, no significant correlation was observed between erythrocyte sedimentation rate and C-reactive protein levels and BASDAI, BASFI, and BAS-G scores in either AAS or JAS patients. To assess the sensitivity to change, 153 patients were included in an 8-week follow-up study. Results measured by all three instruments showed 5.0 to 5.4% change in all patients (Table 4). The BASFI value showed a significant improvement in JAS group (p = 0.04, pair t test), whereas there were no correlations between the changes in BASFI in the AAS group and BASDAI and BAS-G scores in either group (p > 0.05).
Discussion
AS limits the mobility of the spine and other joints and leads to increasing functional impairment. The level of functional impairment is accepted as an important outcome parameter besides clinical measurements, and laboratory and radiological changes, which were found to be insufficient for monitoring patients with AS [14]. In particular, physical function can be quantified by using self-administered questionnaires and indices. The use of many functional indices both for clinical assessment and trials has been increasing in recent years. However, these indices must be tested in several countries to be sure that cultural or language differences do not interfere with results of the assessments and so that the trials in which these indices are used can be easily compared. The ASAS working group has recommended the use of BASDAI and BASFI to obtain outcome measures in AS patients participating in clinical trials [23]. In addition, a more global assessment is also desirable, and validation of a global measure by the BAS-G was established to reflect the effect of AS on patients’ well-being [21]. We chose to test the BASDAI and BASFI or BAS-G, and our study contributes to AS assessment by providing reliable and valid cross-culturally adapted Chinese-language versions for the three most important instruments of disease activity and functioning in use thus far.
In our observation, the reliability of these three instruments of BASDAI and BASFI, and BAS-G for the 24-h test–retest showed acceptable ICCs (0.92–0.94). Our Chinese versions of the BASDAI and BASFI and BAS-G also showed good reliability with Cronbach’s alpha coefficient of 0.87, 0.94, and 0.90, respectively. When Cronbach’s alpha was calculated, we can identify problem items that should be excluded from the scale. After removing each item and recalculating the Cronbach’s alpha, we observed that the Cronbach’s alpha of BASDAI (range 0.83–0.86) and BASFI (range 0.93–0.94) were not significantly changed. Thus, our modified Chinese versions of BASDAI, BASFI, and BAS-G were very feasible for evaluating AS patients. In addition, the distribution of the BASDAI (0–10), BASFI (0–9), and BAS-G (0–10) total score ranges indicated that Chinese BASDAI, BASFI, and BAS-G scales were used effectively. Previously, the BASDAI was developed for evaluating the disease activity of AS patients [20]. After the original English version, several European-language versions were also published, including French [24], Swedish [25], and Spanish [26] versions. Until this study, however, an eastern-language version has not been reported. The original BASFI has also been demonstrated to be valid and reliable among English and other western patient populations [27–29]. In a study by Haywood et al. [30], the BASDAI showed a good level of responsiveness for self-perceived improvement and deterioration in both AS and general health. As with the previous western versions of BASDAI, reproducibility over 2 weeks was good for the total Chinese BASDAI.
Sensitivity to change is a very important property for a functional index. The original English BASDAI was sensitive to change, reflecting 16% mean improvement in inpatient scores after 3 weeks of treatment [20]. The Swedish BASDAI was also found sensitive to intensive inpatient rehabilitation [25], but there were no significant changes after a twice-weekly outpatient exercise program. Similarly, in our observation, 153 outpatients were included in a period of 8 weeks of study in which there were no significant changes in the BASDAI value. Disease duration was significantly longer in our study subjects; therefore, this could be a factor contributing to our results. In addition, our study subjects mainly consisted of outpatients by chance, who are typically in better functional status, and the difference would be small between our first and second observations.
Some limitations must be considered to interpret our data. In the present investigation, there is only one blood sample from which to assess both erythrocyte sedimentation rate and C-reactive protein levels. Erythrocyte sedimentation rate and C-reactive protein are the two widely used acute phase reactants [31]. However, a single baseline measure of both serum erythrocyte sedimentation rate and C-reactive protein might misclassify individuals with respect to long-term status. Especially, disease activity of AS is intermittently high or low or even in momentary spontaneous remission. Selection bias could be resulted when AS patients with either active or inactive disease were enrolled as our study subjects. It would seem likely that this was the reason that we observed no significant correlation between erythrocyte sedimentation rate and C-reactive protein levels and BASDAI, BASFI, and BAS-G scores in either AAS or JAS patients. In addition, our study might have inevitable referral biases because the data were collected from a single medical center. Although recall bias could be a potential problem, the administration of three different instruments made it unlikely that they would remember specific items on all of them.
The cross-culturally adapted versions of the BASDAI, BASFI, and BAS-G produced in this study maintained all the properties of the original English-language versions of the instruments, and our Chinese versions of the BASDAI, BASFI, and BAS-G showed adequate reliability and validity. Thus, disease activity and functional status in Chinese-speaking patients with AS may be adequately evaluated with these adapted versions of the original instruments.
Abbreviations
- AS:
-
ankylosing spondylitis
- JAS:
-
juvenile onset disease
- AAS:
-
adult onset disease
- BASDAI:
-
Bath Ankylosing Spondylitis Disease Activity Index
- BASFI:
-
Bath Ankylosing Spondylitis Functional Index
- BAS-G:
-
Bath Ankylosing Spondylitis Global Score
- VAS:
-
visual analogue scales
- ESR:
-
erythrocyte sedimentation rate
- CRP:
-
C-reactive protein
References
Cuellar ML, Espinoza LR (1996) Management of spondyloarthropathies. Curr Opin Rheumatol 8:288–295
Leirisalo-Repo M (1998) Therapeutic aspects of spondyloarthropathies—a review. Scand J Rheumatol 27:323–328
Khan MA, van der Linden SM (1990) Ankylosing spondylitis and other spondyloarthropathies. Rheum Dis Clin North Am 16:551–579
Brown MA, Jepson A, Young A, Whittle HC, Greenwood BM, Wordsworth BP (1997) Ankylosing spondylitis in West Africans—evidence for a non-HLA-B27 protective effect. Ann Rheum Dis 56:68–70
Khan MA, Braun WE, Kushner I, Grecek DE, Muir WA, Steinberg AG (1977) HLA B27 in ankylosing spondylitis: differences in frequency and relative risk in American Blacks and Caucasians. J Rheumatol Suppl 3:39–43
Gonzalez-Roces S, Alvarez MV, Gonzalez S, Dieye A, Makni H, Woodfield DG et al (1997) HLA-B27 polymorphism and worldwide susceptibility to ankylosing spondylitis. Tissue Antigens 49:116–123
Chou CT, Pei L, Chang DM, Lee CF, Schumacher HR, Liang MH (1994) Prevalence of rheumatic diseases in Taiwan: a population study of urban, suburban, rural differences. J Rheumatol 21:302–306
Chou CT, Chen JM, Hsu CM, Chen SJ (2003) HLA-B27 and its subtypes in 4 Taiwanese aborigine tribes: a comparison to Han Chinese patients with ankylosing spondylitis. J Rheumatol 30:321–325
Riley MJ, Ansell BM, Bywaters EG (1971) Radiological manifestations of ankylosing spondylitis according to age at onset. Ann Rheum Dis 30:138–148
Marks SH, Barnett M, Calin A (1982) A case-control study of juvenile- and adult-onset ankylosing spondylitis. J Rheumatol 9:739–741
Garcia-Morteo O, Maldonado-Cocco JA, Suarez-Almazor ME, Garay E (1983) Ankylosing spondylitis of juvenile onset: comparison with adult onset disease. Scand J Rheumatol 12:246–248
Dawes PT (1999) Stoke ankylosing spondylitis spine score. J Rheumatol 26:993–996
van der Heijde D, Spoorenberg A (1999) Plain radiographs as an outcome measure in ankylosing spondylitis. J Rheumatol 26:985–987
van der Heijde D, Calin A, Dougados M, Khan MA, van der Linden S, Bellamy N (1999) Selection of instruments in the core set for DC-ART, SMARD, physical therapy, and clinical record keeping in ankylosing spondylitis. Progress report of the ASAS Working Group. Assessments in Ankylosing Spondylitis. J Rheumatol 26:951–954
Bellamy N, Muirden KD, Brooks PM, Barraclough D, Tellus MM, Campbell J (1999) A survey of outcome measurement procedures in routine rheumatology outpatient practice in Australia. J Rheumatol 26:1593–1599
Calin A, Edmunds L, Kennedy LG (1993) Fatigue in ankylosing spondylitis—why is it ignored? J Rheumatol 20:991–995
Jones SD, Koh WH, Steiner A, Garrett SL, Calin A (1996) Fatigue in ankylosing spondylitis: its prevalence and relationship to disease activity, sleep, and other factors. J Rheumatol 23:487–490
Ward MM (1999) Health-related quality of life in ankylosing spondylitis: a survey of 175 patients. Arthritis Care Res 12:247–255
van Tubergen A, Coenen J, Landewe R, Spoorenberg A, Chorus A, Boonen A et al (2002) Assessment of fatigue in patients with ankylosing spondylitis: a psychometric analysis. Arthritis Rheum 47:8–16
Garrett S, Jenkinson T, Kennedy LG, Whitelock H, Gaisford P, Calin A (1994) A new approach to defining disease status in ankylosing spondylitis: the Bath Ankylosing Spondylitis Disease Activity Index. J Rheumatol 21:2286–2291
Jones SD, Steiner A, Garrett SL, Calin A (1996) The Bath Ankylosing Spondylitis Patient Global Score (BAS-G). Br J Rheumatol 35:66–71
van der Linden S, Valkenburg HA, Cats A (1984) Evaluation of diagnostic criteria for ankylosing spondylitis. A proposal for modification of the New York criteria. Arthritis Rheum 27:361–368
Khan MA (2002) Update on spondyloarthropathies. Ann Intern Med 136:896–907
Claudepierre P, Sibilia J, Goupille P, Flipo RM, Wendling D, Eulry F et al (1997) Evaluation of a French version of the Bath Ankylosing Spondylitis Disease Activity Index in patients with spondyloarthropathy. J Rheumatol 24:1954–1958
Waldner A, Cronstedt H, Stenstrom CH (1999) The Swedish version of the Bath Ankylosing Spondylitis Disease Activity Index. Reliability and validity. Scand J Rheumatol Suppl 111:10–16
Cardiel MH, Londono JD, Gutierrez E, Pacheco-Tena C, Vazquez-Mellado J, Burgos-Vargas R (2003) Translation, cross-cultural adaptation, and validation of the Bath Ankylosing Spondylitis Functional Index (BASFI), the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) and the Dougados Functional Index (DFI) in a Spanish speaking population with spondyloarthropathies. Clin Exp Rheumatol 21:451–458
Calin A, Garrett S, Whitelock H, Kennedy LG, O’Hea J, Mallorie P et al (1994) A new approach to defining functional ability in ankylosing spondylitis: the development of the Bath Ankylosing Spondylitis Functional Index. J Rheumatol 21:2281–2285
Cronstedt H, Waldner A, Stenstrom CH (1999) The Swedish version of the Bath Ankylosing Spondylitis Functional Index. Reliability and validity. Scand J Rheumatol Suppl 111:1–9
Heikkila S, Viitanen JV, Kautianen H, Kauppi M (2000) Evaluation of the Finnish versions of the functional indices BASFI and DFI in spondylarthropathy. Clin Rheumatol 19:464–469
Haywood KL, Garratt AM, Jordan K, Dziedzic K, Dawes PT (2002) Disease-specific, patient-assessed measures of health outcome in ankylosing spondylitis: reliability, validity and responsiveness. Rheumatol 41:1295–1302
Ruof J, Stucki G (1999) Validity aspects of erythrocyte sedimentation rate and C-reactive protein in ankylosing spondylitis: a literature review. J Rheumatol 26:966–970
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wei, J.CC., Wong, RH., Huang, JH. et al. Evaluation of internal consistency and re-test reliability of Bath ankylosing spondylitis indices in a large cohort of adult and juvenile spondylitis patients in Taiwan. Clin Rheumatol 26, 1685–1691 (2007). https://doi.org/10.1007/s10067-007-0573-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-007-0573-6