Abstract
Although autopsy studies have documented that heart is affected in most of systemic lupus erythematosus (SLE) patients, clinical manifestations occur in less than 10%. QT dispersion, a new parameter that can be used to assess homogeneity of cardiac repolarization and autonomic function, has not been studied in SLE patients. The aim of our study was to evaluate the QT dispersion (QTd) in SLE patients without overt cardiac involvement. Eighty-three patients with a diagnosis of SLE (mean age 41±13) and age- and sex-matched 77 healthy control subjects (mean age 43±10) were enrolled in the study. All subjects had their complete history taken, laboratory examination, and transthoracic echocardiography (ECG). Patients with cardiac disease, hypertension, diabetes, or taking medications that may effect QTd or any ECG abnormalities were excluded. Resting 12-lead ECG were recorded for measurement of QTd. None of the patients and control subjects had overt cardiac involvement. The mean SLE duration was 86.5±15.4 months. QT dispersion was significantly greater in SLE patients than incontrol subjects (55.2±24.7 vs 20.7±5.3 ms, respectively; p<0.001). There was no correlation between QTd and duration of SLE, SLEDAI-K score, corticosteroid usage, and presence of anti SS-A antibody. QT dispersion is significantly increased in SLE patients without overt cardiac involvement. Our result suggests that prolonged QT dispersion can be a useful noninvasive and simple method for early detection of cardiac involvement in SLE patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Systemic lupus erythematosus (SLE) is a connective tissue disease characterized by the formation of autoantibodies and immune complexes. Cardiovascular involvement is now considered as the third leading cause of death among patients with SLE. Autopsy studies have documented that heart is affected in most patients [1]. Pericarditis and premature coronary atherosclerosis are the most prevalent cardiac manifestations. Other rare associations include myocarditis, coronary arteritis, Libman–Sacks endocarditis, constrictive pericarditis, cardiomyopathy, congenital heart block, and rhythm abnormalities. However, clinical manifestations occur in less than 10% of SLE patients [1, 2].
Interlead variability of the duration of the QT interval in the 12-lead echocardiography (ECG) is defined as QT dispersion (QTd). It is a new parameter that can be used to assess the homogeneity of cardiac repolarization and autonomic function [3]. Increased heterogeneity of repolarization was shown in several heart diseases and also associated with increased risk of ventricular tachyarrhythmias [4]. Prolonged QTd was also shown in rheumatoid arthritis and ankylosing spondylitis [5–7]. However, to our knowledge, QTd has not been studied in SLE patients. The purpose of our study was to examine whether QT dispersion increases in SLE patients without overt cardiac involvement.
Materials and methods
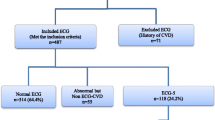
Patients with diagnosis of SLE according to the revised criteria of the American Collage of Rheumatology were selected from the rheumatology outpatient clinic of our university hospital [8]. The healthy control subjects were recruited from our internal medicine and cardiology outpatient clinics. The study patients and control subjects fulfilled all of the following inclusion criteria: (1) no administration of drugs that would potentially influence QT duration except hydroxycholoroquine (HCQ); (2) no history of ischemic heart disease, congestive heart failure, atrial fibrillation, bundle branch block, or abnormal serum electrolytes; (3) normal rest ECG; and (4) a good quality ECG recording for measurement of the QT interval. The exclusion criteria were: (1) moderate or severe valve disease; (2) atrial fibrillation and other ECG abnormalities; (3) systolic LV dysfunction (ejection fraction <50% or an LV end-diastolic dimension >5.5 mm); (4) if the end of the T wave of a patient’s ECG could not be determined reliably; and (5) known presence of cardiac disease including hypertension, diabetes, and coronary artery disease. SLE disease activity was detected by erythrocyte sedimentation rate (ESR) and SLEDAI-2K score [9]. All patients gave written informed consent to take part in the study, which was approved by the local ethics committee. All subjects had their complete history taken, laboratory examination, ECG, and transthoracic echocardiography. Treadmill exercise test with Bruce protocol was performed to rule out coronary artery disease.
Electrocardiography
All SLE patients and controls had a rest 12-lead ECG recorded at 25 mm/s paper speed. QT intervals were measured manually from the onset of QRS to the end of the T wave defined as a return to the T–P baseline. If U waves were present, the subjects were excluded from the study. Three consecutive cycles in each of the 12 leads were measured. All measurements were made blindly (without knowledge of the subjects’ clinical status) by two experienced cardiologist. From the three cycles, QT intervals were calculated. Dispersion parameters were calculated as the difference between maximal and minimal values of QT. The blinded inter- and intra-observer variability of QT measurements were both <5%.
In this study, corrected QTd was not calculated because in previous studies it has been shown that a rate correction of parameters of dispersion of repolarization is probably unnecessary and may even distort the values and predictive value of QTd [10, 11].
Transthoracic echocardiography
Transthoracic echocardiographic examination was performed on all subjects by using a System Five (GE Vingmed Ultrasound, Horten, Norway) cardiac ultrasound scanner and 2.5–3.5 MHz transducers. Left ventricular end-diastolic and end-systolic diameter (cm), ejection fraction (%) were measured by M-mode echocardiography. Color Doppler and continuous and pulsed Dopler were performed to evaluate LV and valvular functions.
Statistical analysis
The skewed data are expressed as median; min–max and normally distributed data are expressed as mean±SD. As the data of QT dispersion were distributed normally, parametric tests were utilized to evaluate differences among the study groups. Means were compared by analysis of variance. Spearman’s correlation rank test was used for the correlation of the parameters. A p value below 0.05 was considered as statistically significant. All analyses were performed by using SPSS 10.0 software.
Results
We studied 83 SLE patients (mean age 41±13) and 77 healthy control subjects (mean age 43±10, p=NS). The baseline characteristics of the patients and of the control group are shown in Table 1. There were no significant differences with respect to sex, age, systolic and diastolic blood pressure, and heart rate. All patients and control subjects had normal ejection fraction (66.9±3.5 vs 65.9±3.3, respectively). Anti-nuclear antibody was positive in all patients except in one, and anti-ds-DNA was positive in 22 patients. Anti-SS-A antibody was positive in 23 patients. In the patient group, mean disease duration was 86.5±15.4 months and the mean value of cumulative prednisolone dose was 17.4±1.9 g. Forty patients were receiving hydroxychloroquine, and 22 patients were under corticosteroid treatment (Table 2). The minimum–maximum and median values of ESR in SLE patients were 3–120 and 15.0 mm/h, respectively; those values of SLEDAI-2K score of SLE patients were 0–18 and 2.0, respectively. No subject had significant valvular heart disease and cardiac complaints. Treadmill exercise test result was negative in patients and controls.
We found that QT dispersion value is significantly higher in SLE patients than in control subjects (55.2±24.7 vs 20.7±5.3 ms, respectively; p<0.001) (Fig. 1). The mean QTd of patients receiving corticosteroids or other anti-inflammatory regimens and those who were not at the time of examination was similar. The mean QTd in patients who have not received hydroxychloroquine was 53.7±19.2 ms, and it was 56.6±29.0 ms in patients who have received HCQ (p=NS). Similar to HCQ, corticosteroid did not give statistically significant results. In patients who have not received corticosteroid, mean QTd was 56.1±27.0 ms, and it was 52.5±17.2 ms in patients who have received corticosteroid (p=NS). There was no correlation between the QTd and the baseline characteristics of the subjects including disease duration, ESR, and SLEDAI-2K score, the presence of any of the diagnostic criteria for SLE, and also the presence of anti-SS-A antibody and QTd.
Discussion
QT dispersion has been shown to be increased and an important prognostic factor in several cardiovascular conditions such as coronary artery disease, congestive heart failure, and cardiomyopathies [12–16]. Although increased QT dispersion has been shown in various rheumatic diseases [5–7, 17], QTd has not been examined in SLE patients yet. To the best of our knowledge, this is the first study evaluating the QT dispersion in patients with SLE. We found that QT dispersion is significantly higher in patients with SLE than in control subjects.
Myocardial involvement can be seen in SLE patients even in the absence of clinical cardiac manifestations. Previous studies using Tc-99 m sestamibi myocardial perfusion single-photon emission computed tomography (SPECT) showed high incidence of myocardial perfusion abnormalities in asymptomatic lupus patients without any clinical signs of cardiac involvement [18–20]. Schillaci et al. found that eight patients with positive SPECT had normal epicardial coronary vessels documented with coronary angiography [18]. In patients without clinical cardiac manifestations, those perfusion defects were probably due to the primary immunological damage and small focal cardiofibrosis of this autoimmune disease. The areas of myocardial fibrosis in SLE may disrupt the course of ventricular repolarization and lead to increase the dispersion of recovery time throughout the ventricle. As QT dispersion proves useful information of heterogeneity of ventricular repolarization, prolonged QTd that we found in our study may reflect silent myocardial involvement in SLE patients. Therefore, QT dispersion may be a useful and simple marker to identify subclinical myocardial involvement in SLE patients.
Heart rate variability (HRV) is one of the methods in evaluating autonomic function which was found to be significantly impaired in patients with SLE than in control subjects [21]. QT dispersion has been shown to increase in patients with autonomic dysfunction [22]. Therefore, another possible explanation of prolonged QTd in SLE patients may be related to the autonomic dysfunction, which can be present in the SLE patients.
The potential limitations of this study should be addressed. HRV measurements and myocardial perfusion SPECT analysis in association with QTd may give more information about the etiology of prolonged QTd in SLE patients, but these tests are more expensive and complex and may not be necessary in patients without overt heart disease. Therefore, QTd which has not been studied in SLE patients was examined alone in this present study.
Conclusion
QT dispersion is significantly increased in SLE patients without overt cardiac involvement. Our result may indicate that prolonged QT dispersion can be a useful noninvasive and simple method of early detection of subclinical cardiac involvement in SLE patients. Further studies are needed to evaluate the prognostic significance of QT dispersion and to clarify the mechanism of increased QT dispersion in SLE.
References
Mandell BF (1987) Cardiovascular involvement in systemic lupus erythematosus. Semin Arthritis Rheum 17:126–141
Hejtmancik MR, Wright JC, Quint R, Jennings FL (1964) The cardiovascular manifestations of systemic lupus erythematosus. Am Heart J 68:119–130
Kautzner J, Malik M (1997) QT interval dispersion and its clinical utility. PACE 20:2625–2640
Zabel M, Portnoy S, Franz MR (1995) Electrocardiographic indexes of dispersion of ventricular repolarization: an isolated heart validation study. J Am Coll Cardiol 25:746
Yildirir A, Aksoyek S, Calguneri M et al (2000) QT dispersion as a predictor of arrhythmic events in patients with ankylosing spondylitis. Rheumatology (Oxford) 39(8):875–879
Pırıldar T, Sekuri C, Utuk O, Kemal Tezcan U (2003) QT dispersion in rheumatoid arthritis patients with and without Sjögren’s syndrome. Clin Rheumatol 22:225–228
Cindas A, Gokce-Kutsal Y, Tokgozoglu L, Karanfil A (2002) QT dispersion and cardiac involvement in patients with rheumatoid arthritis. Scand J Rheumatol 31(1):22–26
Tan EM, Cohen AS, Fries JF et al (1982) The 1982 revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 25:1271–1277
Gladman DD, Ibanez D, Urowitz MB (2002) Systemic lupus erythematosus disease activity index 2000. J Rheumatol 29(2):288–291
Marek M, Camm AJ (1997) Mystery of QTc interval dispersion. Am J Cardiol 79:785–787
Zabel M, Woosly RL, Franz MR (1997) Is dispersion of ventricular repolarisation rate dependent? PACE 20(Part I):2405–2411
Perkiomaki JS, Koistien J, Yli-Mary S, Huikuri HV (1995) Dispersion of QT interval in patients with and without susceptibility to ventricular tachyarhythmias after previous myocardial infarction. J Am Coll Cardiol 26:174–179
Statters DJ, Malik M,Ward DE, Camm AJ (1994) QT dispersion: problems of methodology and clinical significance. J Cardiovasc Electrophysiol 5:672–685
Glancy JM, Garratt CJ, Woods KI, de Bono DP (1995) QT dispersion and mortality after myocardial infarction. Lancet 345:945–948
Tieleman RG, Crijns HJ, Wiesfeld AC, Posma J, Hamer HM, Lie KI (1995) Increased dispersion of recractoriness in the absence of QT prolongation in patients with mitral valve prolapse and ventricular arrhythmias. Br Heart J 73:37–40
Barr CS, Naas A, Freeman M, Lang CC, Struthers AD (1994) QT dispersion and sudden unexpected death in chronic heart failure. Lancet 343:327–329
Sgreccia A, Morelli S, Ferrante L et al (1998) QT interval and QT dispersion in systemic sclerosis (scleroderma). J Int Med 243:127–132
Schillaci O, Lagana B, Danieli R et al (1999) Technetium-99 m sestamibi single-photon emission tomography detects subclinical myocardial perfusion abnormalities in patients with systemic lupus erythematosus. Eur J Nucl Med 26(7):713–717
Lin CC, Ding HJ, Chen YW, Wang JJ, Ho ST, Kao A (2003) Usefulness of technetium-99 m sestamibi myocardial perfusion SPECT in detection of cardiovascular involvement in patients with systemic lupus erythematosus or systemic sclerosis. Int J Cardiol 92:157–161
Sun SS, Shiau YC, Tsai SC, Lin CC, Kao A, Lee CC (2001) The role of technetium-99 m sestamibi myocardial perfusion single-photon emission computed tomography (SPECT) in the detection of cardiovascular involvement in systemic lupus erythematosus patients with non-specific chest complaints. Rheumatology 40:1106–1111
Lagana B, Tubani L, Maffeo N et al (1996) Heart rate variability and cardiac autonomic function in systemic lupus erythematosus. Lupus 1:49–55
Wei K, Dorian P, Newman D, Langer A (1995) Association between QT dispersion and autonomic dysfunction in patients with diabetes mellitus. J Am Coll Cardiol 26:859–863
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yavuz, B., Atalar, E., Karadag, O. et al. QT dispersion increases in patients with systemic lupus erythematosus. Clin Rheumatol 26, 376–379 (2007). https://doi.org/10.1007/s10067-006-0364-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-006-0364-5