Abstract
The objective of this study is to evaluate the efficacy, toxicity, and long-term outcome of low-dose IV cyclophosphamid therapy with repeated frequent intervals in combination with oral and IV methylprednisolone in patients with SLE nephritis. In this study, 113 patients diagnosed as having SLE and glomerulonephritis were assessed in between 1993 and 2002, with a median follow-up of 44.1±41.2 months. The patients were treated with 500 mg IV cyclophosphamide and 1 g IV methylprednisolone together with 60 mg/alternate-day oral methylprednisolone in a given schedule. The clinical and laboratory data were evaluated. There were significant improvements in the clinical and the laboratory parameters. Six patients died shortly after being hospitalized due to the disease activity itself. Eight patients were excluded from the study because of low compliance. The renal functions of the patients remained stable throughout the therapy; only 16/99 patients needed one or two additional pulses. Temporary leukopenia developed in 18/99 patients and diminished with the suspension or prolongation of the IV cyclophosphamide administration. Gastrointestinal side effects, which needed extra medication, developed in 20 patients. Hematuria was observed in 6/99 patients. Menstrual abnormalities were seen in 7/99 patients. No serious infections due to immunosuppression were observed with the given regimen. Hypertension was observed in 13 patients (minimum of 140/90 mmHg, maximum of 190/110 mmHg) and controlled with angiotensine-converting enzyme inhibitors. Mild central obesity was observed in 15 of the patients. Leimyosarcoma was observed in one patient who died during the follow-up period. Therapy starting with the weekly low-dose IV cyclophosphamide to induce remission together with IV and oral steroids, followed by prolonged intervals with the same doses for 2 years, appears to be useful in preserving renal function without major side effects in patients with lupus nephritis, in comparison to other studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Systemic lupus erythematosus (SLE) is a multisystemic autoimmune disease that may affect virtually every organ of the body. Renal involvement is one of the most frequent and serious manifestations of the disease. Nephritis in SLE carries significant morbidity and mortality and is an important determinant for survival [1–3]. Various studies have described a 5-year cumulative probability of 11% to 48% for end-stage renal disease in patients with SLE nephritis [4–6]. High-dose intravenous (IV) cyclophosphamide, in combination with glucocorticosteroids, has become the standard treatment of lupus nephritis because of the results of the National Institute of Health (NIH) that demonstrated the superiority of this regimen over oral or IV glucocorticoid therapy alone [7–11]. Although safer alternatives, including mycophenolate mofetil and rituximab, have been recently introduced for the treatment of renal involvement in SLE, the long-term efficacies of these agents have not been determined yet, and cyclophosphamide plus glucocorticosteroids still remain the standard therapy for lupus nephritis [12, 13].
Moreover, the comparison of the efficacy of different routes of cyclophosphamide administration in the treatment of SLE nephritis in particular was not feasible for this study because the study sample consisted of patients with lupus nephritis of all WHO classes and the number of patients in each treatment arm was too small. Also, in previous reports, high-dose IV cyclophosphamide treatment was discussed as being highly toxic because of opportunistic infections and ovarian failure [7–9, 14].
In this open study we evaluate the efficacy, toxicity, and outcome of an intensified, intermittent low-dose IV cyclophosphamide and IV methylprednisolone combination, together with oral alternate-day methylprednisolone therapy with standard doses in a given schedule.
Patients and methods
In this open study, 113 patients, who were diagnosed as having both SLE and glomerulonephritis and hospitalized in the Rheumatology Department of Hacettepe University Faculty of Medicine between 1993 and 2002, were included consecutively during 2 years. SLE was diagnosed among the patients who fulfilled the four of the criteria defined by the American College of Rheumatology [15], and glomerulonephritis was defined as a sediment on two or more urinalyses that showed either more than nine erythrocytes per HPF or erythrocyte or leukocyte, or both, casts (without evidence of infection), plus proteinuria of more than 500 mg/day repeated twice. Patients who had been treated with cyclophosphamide or other immunosuppressive drugs or had taken >15 mg/day prednisolone (or equivalent) during the previous month were excluded because this high dose of prednisolone could affect the renal outcome before starting the therapy. Patients who were also excluded from the study were those who had been suffering from active or chronic infections, renal thrombotic microangiopathy, or pre-existing chronic renal failure (to see the therapy benefits on active lupus nephritis), or pregnant patients or those with only one kidney, previous malignancies, or established diabetes mellitus. Also, those patients with previously documented severe toxicity to immunosuppressive drugs and glucocorticoids, and those in whom we anticipated poor compliance with the protocol, were excluded from the study. Demographical data and information regarding disease diagnosis and manifestations were obtained from the patients. The same physician examined all patients. Renal biopsies were, unfortunately, not performed on any of the patients before starting the therapy. Intensified, intermittent low-dose (500 mg) IV pulse cyclophosphamide plus glucocorticoids has been the standard treatment for lupus nephritis in our clinic since 1990. Hence, all patients were treated according to this standard protocol (see below). All patients were also informed regarding the benefits and possible toxicities of this regimen.
Demographical properties of the patients and the following parameters were collected at the beginning and at the end of the study: serum blood urea nitrogen and creatinine levels, calculated creatinine clearance, erythrocyte sedimentation rates, C-reactive protein levels, anti-double stranded DNA (anti-DNA) antibody levels, compleman 3 and 4 (C3 and C4) levels, complete blood count, total serum protein and albumin levels, 24-h proteinuria levels, urinary analysis, and the calculated SLE diseases activity index (SLEDAI) [16].
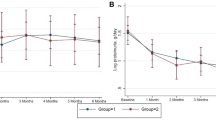
All patients were treated with pulse methyl-prednisolone (1 g/day) followed by pulse cyclophosphamide (500 mg/day) and oral prednisolone therapy. The pulse treatment with cyclophosphamide and methylprednisolone, and the oral prednisolone schedules, are given in Table 1. After starting with three consecutive methylprednisolone pulses, one cyclophosphamide pulse followed; in continuation, each cyclophosphamide pulse was administered after every methyl prednisolone pulse. This interval schedule is schematized in Fig. 1. If, according to the clinical status of each patient, an unexpected activation of the disease or drug-related leukopenia or hematuria occurred, further administrations of the pulse therapies were added and, if needed, the durations of the intervals were lengthened. During 24 months each patient was treated with a mean of 14.1±2.6 g cyclophosphamide and 7.6±3.6 g methyl prednisolone. We performed a leukocyte count before every pulse therapy to guide subsequent cyclophosphamide dose adjustments. IV mesna (400 mg/day) was given together with IV pulse cyclophosphamide administrations to prevent the patients from hemorrhagic cyctitis resulting from bladder malignancies. Also, patients were instructed to continue oral hydration to maintain a dilute and frequent diuresis for at least 24 h after the infusion of cyclophosphamide. Urine analysis was repeated every 2 weeks. Patients were followed closely for the expected side effects of the cyclophosphamide. The development of leukopenia [white blood cell (WBC) counts <3,500/mm3], serious gastrointestinal intolerance, or dysuria and hematuria (>5 red blood cells/HPF) due to cyclophosphamide use were considered reasons to temporarily suspend cyclophosphamide treatment for 1–2 weeks. After the patient’s WBC count recovered or the hematuria diminished, the drug treatment was continued at the breaking-up dosage, or if the patient did not recover, the treatment with cyclophosphamide was planned to switch to oral azathiopyrin. We planned to continue the IV cyclophosphamide therapy after remission was achieved, without changing the therapy to other disease-modifying antirheumatic drugs like azathiopyrin, but after the first year we decided to lengthen the intervals from 1 month to 2 months in need of the patients.
Administration interval schedule of the given IV therapies. The X-axis shows the time intervals as three consecutive days, three times in 1-week intervals, three times in 10-day intervals, and three times in 15-day intervals (this pattern continues). The Y-axis shows the same dose IV methylprednisolone (1 g) and IV cyclophosphamide (500 mg) pulses
Oral methyl prednisolone therapy was started in every patient as 60 mg/day, as an induction regimen. To avoid the side effects of the steroid, the dosage was decreased by 5 mg/day every other day until the dosage was 40 mg/day. Then, the regimen was switched to the alternate-day steroid regimen, as shown in Table 1, and continued to decrease until the end of the therapy (Table 1).
Prophylactic treatment against steroid-induced osteoporosis was started with biphosphonides as antiresorptive agents. Chloroquine was administered at 200 or 400 mg/day. Low-dosage acetyl salicylic acid (80 g/day) therapy was started for the endothelial functions, and proton-pump inhibitors were administered for gastro-protection. Hypertension (diastolic blood pressure ≥90 mmHg) was treated initially with angiotensin-converting enzyme inhibitors, unless contraindicated. Contraception was prescribed for all sexually active patients of childbearing potential. These patients were informed about the potential deleterious effects of their disease during pregnancy. In general, all patients were seen monthly during the first 6 months of the study, and later, every 3 months. Diets were strictly advised for all patients according to their body mass indexes and serum cholesterol and glucose levels.
Complete remission (CR), reactivation (flare), and nonresponse (NR) of nephritis after immunosuppressive treatment were defined as suggested by Boumpas and Balow [17]:
-
1.
CR was defined as stabilization or improvement of renal function with an erythrocyte count of less than ten cells per HPF in a centrifuged 50-ml urine sample, absence of cellular casts and reduction of proteinuria to 1 g/day of protein or less, and normalization of C3 level persistently for at least 6 months.
-
2.
Reactivation of glomerular disease was defined as new active nephritis with an increase of at least 50% (relative to the study) in at least two of the following: number of the dysmorphic erythrocytes (≥10/HPF), number of cellular casts, proteinuria (≥1g/day) and/or serum creatinine level, decreases in C3 and C4 levels, and elevation of anti-DNA. Reactivation was treated with an additional IV cyclophosphamide and methylprednisolone pulse. If more than two additional pulses were needed, this was also accepted as NR.
-
3.
NR was defined as deterioration in renal function after excluding other causes, such as sepsis, nephrotoxic agents, overdiuresis, and renal vein thrombosis; increase in proteinuria; or a reduction in proteinuria not to the extent of CR.
Laboratory evaluation
The anti-DNA antibody was assayed by enzyme-linked immunosorbant assay. Serum C3 level was measured by nepholometry. Urine protein was measured by a dye method using pyrogallol red. Serum and urine creatinine assays were performed by the Jaffe method. Creatinine clearance, expressed in milliliters per minute, was calculated based on the serum creatinine level and a 24-h urine creatinine assay using the formula UV/P, where U is the urinary creatinine concentration, V is the urine flow rate, and P is plasma creatinine level.
Statistical analysis
Unless otherwise stated, values are expressed as mean±SD. All data were collected in the Statistical Package for the Social Sciences version 11.0 (Chicago, IL). Variables within the group were analyzed by using the Wilcoxon test for nonparametric variables and a paired T test for parametric variables. A p value less than 0.05 was accepted as significant.
Results
The study included 96 female and 17 male patients. Six patients died shortly after being admitted to the hospital. They were followed for a median of 15 days (6–45 days) after hospitalization. Those six patients were not included in the study because of the short follow-up duration and the small number of given IV therapies (minimum–maximum of 0–3 pulses of cyclophosphamide 500 mg IV). Eight patients were excluded from the study because of low compliance. Four of those eight patients were taken off of the study because of a lack of compliance. The other four patients did not follow the study’s protocol and they did not use the medications as described, nor did they obey the time schedule they had to come to the center and make up the control group. Consequently, we did not get healthy data from those four patients either, and we excluded them from the study. The remaining 99 patients (88 females/11 males) were included in the study. The mean age of the patients when they were included in the study was 35.5±11.7 years. The given therapeutic regimen of cyclophosphamide and oral/IV steroids at the given doses was well tolerated by all patients. Descriptive changes in the clinical features of the patients due to therapy are given in Table 2 as pre- and posttreatment values. The mean SLEDAI index of all patients was 20±7.2; after the treatment, it decreased to 4.9±4.8 (p<0.05). The mean anti-DNA antibody level was 158.4±61.6; after treatment, it decreased to 19.2±30.5 (p<0.05). Changes of the collected pre- and posttreatment parameters included in the study are given in Table 3.
The most common side effects appeared to be leukopenia (in 18 patients) and microscopic hematuria (in 6 patients). Gastrointestinal intolerance, including nausea and vomiting, was also a common observed side effect of the therapy (in 20 patients). These side effects were manageable by dose adjustment, and the patients who suffered from gastrointestinal symptoms were prescribed ondansetron 8 mg Quaque (Latin: each, every; used in medical prescriptions) Q 4–8 h.
No patients needed to be hospitalized for severe bacterial or viral infections due to immunosuppression because WBC was closely followed and the results were guided for the immunosuppression as described above. Minor infections, like cyctitis, vaginitis, or upper-airway infections, were treated with antibiotics suitable for the culture results, but they were not noted if they were not severely affecting the disease progression and patients’ general healthy status. In seven patients, menstrual irregularities like oligomenorrhea or premature menopause were observed. The study’s follow-up duration was 24 months, but the patients were followed for 44.1±41.2 (mean±SD) months. Thirty-four patients were followed for more than 48 months (90.9±36.3 months). The mean duration of remission was 30±6 months. During the follow-up period, leimyosarcoma in the uterus developed in one patient, who died. Sixteen patients needed additional pulses, for what were accepted as reactivations of the renal flares, during the first year of the therapy. These patients did not reach the CR criteria. None of them needed dialysis. None of the patients’ treatments needed to be switched to azathiopyrin because of side effects of cyclophosphamide. Forty-seven patients reached CR at the end of the first year, and we continued to give them IV cyclophosphamide (500 mg IV—standard dose) in 2-month intervals during the second year. Twenty-four patients showed rapid improvements of their clinical and laboratory results during the first year of the therapy, but they did not completely reach the CR criteria. We accepted them in the partial-response group. We continued the monthly pulses (cyclophosphamide 500 mg in standard dose) for these patients and they achieved CR at the end of the second year.
Mild central obesity was observed in 15 patients. Hypertension was observed in 13 patients (minimum of 140/90 mmHg, maximum of 190/110 mmHg) and controlled with angiotensine-converting enzyme inhibitors. Nine patients showed elevations of fasting blood glucose. However, glycemic control was achieved by diet regulation only, and none of these patients were treated with insulin injections. Blood glucose values of these patients returned to normal levels during follow-up with reduction of glucocorticoids.
Discussion
This is an open 24-month prospective study determining the efficacy and toxicity of intensive, intermittent, low-dose (500 mg) IV cyclophosphamide boluses together with 1 g methylprednisolone boluses in combination with oral alternate-day prednisolone in the treatment of active SLE nephritis. The widespread use of pulse cyclophosphamide therapy in the treatment of lupus nephritis was stimulated by studies performed by the NIH [7–10]. The drug schedules used have been empiric and largely based on acceptable levels of bone marrow suppression. The most commonly used IV regimen consists of monthly infusions for a course of 6 months followed by infusions every several months [18, 19]. There are no good studies that provide guidelines to indicate when cyclophosphamide therapy should be discontinued. In lupus nephritis, it is commonly recommended that cyclophosphamide be continued for a period of 1 year after the nephritis has been judged to be in remission; however, there are no data to actually support this recommendation. Moreover, in some patients, even prolonged continuous therapy for up to 2 years is inadequate to achieve control of the disease [18, 19]. Intervals between the boluses and the duration of IV cyclophosphamide therapy in lupus nephritis have not been sufficiently studied to define the optimal regimen for IV treatment.
The most commonly used dose of IV cyclophosphamide is 500–750 mg/m2 given monthly, although reductions in dose are generally required in patients with impairments of renal function or pre-existent leukopenia. An IV dosage of 500 mg weekly has been reported to show comparable clinical effects compared with standard regimens with fewer adverse effects, although there are no direct comparative studies of regimens [18–24]. Recently, the Euro-Lupus Nephritis trial showed that low-dose IV cyclophosphamide regimens were effective in most lupus patients with diffuse proliferative glomerulonephritis [21]. In this study, we gave patients a smaller amount of cyclophosphamide/year but we gave cyclophosphamide in frequent intervals at the beginning of therapy when the disease was more active. Careful follow-up of WBC and adjustment of the cyclophosphamide dose was enough to control SLE and prevent relapse, with minimal adverse events. We did not perform kidney biopsies. The role of kidney biopsy in the assessment of lupus nephritis has been controversial. Several studies have supported the concept that diffuse proliferative lupus nephritis is associated with poor prognosis, both in terms of renal functions and in terms of the patient’s survival. Some other reports, however, have repudiated the usefulness of renal biopsy in predicting outcome and claimed that renal morphology does not add to the clinical information obtained before biopsy [25, 26].
In the study by Boumpas et al., long IV cyclophosphamide pulses were associated with more side effects. Also, the NIH regimen was associated with a high rate of infections and ovarian failure [9–11, 14]. In our study, no patients suffered from serious opportunistic infections, which may be due to the close follow-up of the WBC count. Of the 99 patients, 18 developed leukopenia after temporary suspension of the IV cyclophosphamide pulses; any infections were observed or a requirement for the drug therapy to be begun again was made. We feel that our regimen may reduce the risk of infections. Also, in our protocol, the IV 1 g methylprednisolone, given before the IV cyclophosphamide pulses, could prevent leukopenia caused by the cyclophosphamide itself. Boumpas et al. reported lower infection rates after short-course cyclophosphamide regimens than after long-course regimens, which is also comparable with our data. Gastrointestinal side effects, including nausea and vomiting, were the other most common side effects that were observed. Oral ondensetron gave relief and minimized these side effects. Our results were similar to those of D’Cruz et al. [20, 22]; they first used a low-dose weekly regimen in the treatment of lupus nephritis. They gave 500-mg weekly pulses of IV cyclophosphamide in a median of three times; later, they added oral azathioprine or oral cyclophosphamide. They reported NR to the therapy in 33% of their patients. This result was higher than that in our study. This could be due to the short-course administration of IV cyclophosphamide only for remission induction. Recently, Contreras et al. [27] reported that, after the induction of remission with monthly IV high-dose (1 g) cyclophosphamide, the continuing of quarterly IV cyclophosphamide (in the same dose) and therapy with oral azathiopyrine or mycofenolate mophetil both gave the same therapeutic results, but oral regimens were less toxic than IV cyclophosphamide. In our series with a longer follow-up period, we showed that low-dose IV cyclophosphamide administration in a given schedule is not as toxic as, and is more efficient than, Contreras et al. mentioned.
Seven of our patients suffered menstrual irregularities or ovarian failure from IV cyclophosphamide. Boumpas et al. noted that intermittent pulse cyclophosphamide therapy was associated with sustained amenorrhea in up to 39% of patients treated with prolonged monthly cyclophosphamide and in 12% of patients treated with seven monthly pulses of cyclophosphamide [9, 14]. In this respect, our results were worse than the results of D’Cruz et al., but were better than the results of the Boumpas et al.
Six of our patients suffered from hemorrhagic cyctitis. The incidence and severity of this complication is reduced by adequate hydration and frequent bladder emptying, and by the concomitant use of mesna. Previous studies of lupus nephritis showed that hemorrhagic cyctitis caused by bladder cancer is related with the oral use of cyclophosphamide rather than the IV use. Some authors have suggested an increased incidence of hematological malignancies following immunosuppressive therapy in patients with rheumatic diseases, such as an incidence of 10% following therapy with alkylating agents [28–30]. However, the role of these therapies in the development of malignancies is debatable. These malignancies could be associated with SLE itself rather than the immunosuppressive agents [27]. In our study, we observed leimyosarcoma in only one patient, and she died after long follow-up. No other hematopoietic or lymphoreticular system malignancies were observed. Slight central obesity and hypertension that was controlled with antihypertensive agents were observed in a minority of the patients. We thought that the administration of the oral steroids in alternate days may be risky for the disease flare, but intensified intervals and the low dosage of the IV cyclophosphamide therapy could prevent both the activation and more complications.
In the present study, only 16 (16.2%) of the patients developed flairs, in contrast with the results of Boumpas [9] and Belmont [31], who reported 35 and 30% failures, respectively, with monthly IV cyclophosphamide pulses. In a previous report with lupus nephritis, the relapse rate after 6 months of continuous monthly therapy is approximately 50%, with evidence to suggest that maintenance therapy with less frequent infusions of cyclophosphamide reduces the likelihood of relapse [9].
The scope of this study is limited by the lack of the randomization and a control group structured by the patients who were treated with monthly administrations of IV cyclophosphamide. Moreover, historical comparison with other studies may be difficult. Furthermore, the lack of histological information appears to be the major limitation of our study, and this weakness probably had an impact on the interpretation of our data. Nevertheless, this study represents the effects of intensive intermittent low-dose (500 mg) IV cyclophosphamide therapy together with 1 g IV methylprednisolone boluses and oral alternate-day steroid regimens in a given schedule, with high efficacy and a low incidence of complications. Prospective, randomized trials with histological classifications of nephritis are strictly needed to evaluate whether the feasibility, safety, and efficacy of our protocol are superior to those of similar protocols that are currently employed in other lupus centers.
References
Donadio JV, Hart GM, Bergstralh EJ, Holley KE (1995) Prognostic determinants in lupus nephritis: a long term clinicopathological study. Lupus 4:109–115
Ward MM, Pyun E, Studenski S (1996) Mortality risk associated with specific clinical manifestations of systemic lupus erythematosus. Arch Intern Med 156:1337–1344
Vu TV, Escalante A (1999) A comparison of the quality of life of patients with systemic lupus erythematosus with and without end-stage renal disease. J Rheumatol 26:2595–2601
Mok CC, Wong RWS, Lau CS (1999) Lupus nephritis in southern Chinese patients: clinicopathological findings and long-term outcome. Am J Kidney Dis 34:315–323
Appel GB, Valeri A (1994) The course and treatment of lupus nephritis. Annu Rev Med 45:525–537
Bakir AA, Levy PS, Dunea G (1994) The prognosis of lupus nephritis in African-Americans: a retrospective analysis. Am J Kidney Dis 24:159–171
Austin HA III, Klippel JH, Balow JE, le Riche NGH, Steinberg AD, Plotz PH, Decker JL (1986) Therapy of lupus nephritis: controlled trial of prednisone and cyctotoxic drugs. N Engl J Med 314:614–619
Steinberg AD, Steinberg SC (1991) Long-term preservation of renal function in patients with lupus nephritis receiving treatment that includes cyclophosphamide versus those threaded with prednisone only. Arthritis Rheum 34:945–950
Boumpas DT, Austin HA III, Voughan EM, Klippel JH, Steinberg AD, Yarboro CH et al (1992) Controlled trial of pulse methylprednisolone versus two regimens of pulse cyclophosphamide in severe lupus nephritis. Lancet 340:741–751
Gourley MF, Austin HA III, Scott D, Yarboro CH, Voughan EM, Muir J et al (1996) Methylprednisolone and cyclophosphamide, alone or in combination, in patients with lupus nephritis. Ann Intern Med 125:549–557
İllei GG, Austin HA, Crane M, Collins L, Gourley MF, Yarboro CH et al (2001) Combination therapy with pulse cyclophosphamide plus pulse methylprednisolone improves long-term renal outcome without adding toxicity in patients with lupus nephritis. Ann Intern Med 135:248–257
Pisoni CN, Karim Y, Cuadrado MJ (2005) Mycophenolate mofetil and systemic lupus erythematosus: an overview. Lupus 14(Suppl 1):9–11
Thatayatikom A, White AJ (2006) Rituximab: a promising therapy in systemic lupus erythematosus. Autoimmun Rev 5:18–24
Boumpas DT, Austin HA III, Vaughan EM, Yarboro CH, Klippel JH, Balow JE (1993) Risk for sustained amenorrhea in patients with systemic lupus erythematosus receiving intermittent pulse cyclophosphamide therapy. Ann Intern Med 119:366–369
Tan EM, Cohen AS, Fries JF, Masi AT, McShane DJ, Rothfield NF, Schaller JG, Talal N, Winchester RJ (1991) The 1982 revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 34:945–950
Gordon C (2003) Assessing disease activity and out come in systemic lupus erythematosus. In: Hochberg MC, Silman A, Smolen JS, Weinblatt ME, Weisman MH (eds) Rheumatology. Mosby, Edinburgh, pp 1389–1393
Boumpas DT, Balow JE (1998) Outcome criteria for lupus nephritis trials: a critical overview. Lupus 7:622–629
Austin HA, Balow JE (1999) Natural history and treatment of lupus nephritis. Semin Nephrol 19:2–11
Ortmann RA, Klippel JH (2000) Update on cyclophosphamide for systemic lupus erythematosus. Rheum Dis Clin North Am 26:363–375
D’Cruz D, Cuadrado MJ, Mujic F et al (1997) Immunosuppressive therapy in lupus nephritis. Clin Exp Rheumatol 15:275–282
Houssiau FA, Vasconcelos C, D’cruz D, Sebastiani GD, Garrido ER, Danieli MG, Abramovicz D et al (2002) Immunosuppressive therapy in lupus nephritis. The Euro-Lupus Nephritis Trial, a randomized trial of low-dose versus high-dose intravenous cyclophosphamide. Arthritis Rheum 46:2121–2131
Martin-Suarez I, D’Cruz D, Mansoor M et al (1997) Immunosuppressive treatment in severe connective tissue diseases: effects of low dose intravenous cyclophosphamide. Ann Rheum Dis 56:481–487
Mok CC, Kwan Ho CT, Siu YP, Chan KW, Kwan TH et al (2001) Treatment of diffuse proliferative lupus glomerulonephritis: a comparison of two cyclophosphamide-containing regimens. Am J Kidney Dis 38:256–264
Chan TM, Li FK, Wong RW et al (1995) Sequential therapy for diffuse proliferative and membranous lupus nephritis: cyclophosphamide and prednisolone followed by azathioprine and prednisolone. Nephron 71:321–327
Golbus J, Mc Cune WJ (1994) Lupus nephritis. Classification, prognosis, immunopathogenesis and treatment. Rheum Dis Clin North Am 20:213–242
Gladman DD, Krowitz MD (2000) Clinical features of SLE. Klippel Dieppe Sec. Edd. Mosby, London, pp 7.1.5–7.1.8
Contreras G, Pardo V, Leclercq B, Lenzo O, Tozman E, O’Nas P, Roth D (2004) Sequential therapies for proliferative lupus nephritis. N Engl J Med 350:971–980
Klinlen LJ (1985) Incidence of cancer in rheumatoid arthritis and other disorders after immunosuppressive treatment. Am J Med 78(Suppl 1A):44–49
Fox DA, McCune J (1994) Immunosuppressive therapy of systemic lupus erythematosus. Rheum Dis Clin North Am 20:265–299
Abu-Shakra M, Gladman DD, Urowitz MB (1996) Malignancy in systemic lupus erythematosus. Arthritis Rheum 39:1050–1054
Belmont HM, Storch M, Buyon J, Abramson S (1995) New York University/Hospital for joint disease experience with intravenous cyclophosphamide treatment: efficacy in steroid unresponsive lupus nephritis. Lupus 4:104–108
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Calguneri, M., Ozbalkan, Z., Ozturk, M.A. et al. Intensified, intermittent, low-dose intravenous cyclophosphamide together with oral alternate-day steroid therapy in lupus nephritis (long-term outcome). Clin Rheumatol 25, 782–788 (2006). https://doi.org/10.1007/s10067-006-0217-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-006-0217-2