Abstract
To examine the expression of the apoptosis regulatory protein, Bcl-xL, in the synovium of patients with rheumatoid arthritis (RA) and osteoarthritis (OA). Immunohistochemistry for Bcl-xL was carried out on synovial samples from patients with RA and OA. Reverse transcriptase polymerase chain reaction (RT-PCR) and Western blot analysis were performed to qualitatively examine the expression of Bcl-xL. Bcl-xL expression was detected in the lining, endothelium and inflammatory cells of both RA (n=20) and OA (n=10) samples. However, there was significantly more expression in the lining of RA synovium compared to OA (77 vs 61%, p<0.05). Many of the positive cells in the RA subsynovium were noted to be plasma cells. There was a significant correlation between Bcl-xL expression and the number of inflammatory cells in the subsynovium of RA and OA patients (r s=0.376, p<0.05, n=30). Age and disease duration did not correlate with Bcl-xL expression in rheumatoid patients. Bcl-xL may play a role in the extended survival of synoviocytes and inflammatory cells in rheumatoid synovium.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rheumatoid arthritis (RA) is an autoimmune condition characterised by a florid inflammatory infiltrate of the synovial tissue in response to an unknown antigen [1]. The pathological hallmark of the disease is synovial hyperplasia with infiltration by inflammatory cells, ultimately leading to invasion of local cartilage and bone by synovial overgrowth (pannus) [2]. Apoptosis is a means of ‘programmed cell death’, which is necessary in many physiological processes; for example, the elimination of immunocytes at the end of immune responses [3, 4]. Dysregulation of apoptosis has been implicated in many disease processes, in particular, cancer and autoimmunity [5]. In RA, there is excessive proliferation of synoviocytes as well as accumulation of inflammatory cells. Fas-mediated apoptosis has been shown to occur in rheumatoid synovial cells [6]. However, the relative sparing of lymphocytes from apoptosis in RA synovium [7] suggests that the control of the apoptotic pathway may be dysfunctional.
Members of the Bcl-2 family regulate apoptosis by altering mitochondrial permeability and the release of apaf-1 and cytochrome c [8, 9]. It is postulated that the control of apoptosis depends on the ratio of pro- and anti-apoptotic Bcl-2 proteins [10]. Bcl-2 is overexpressed in RA synovial tissue compared to osteoarthritis (OA), and Bcl-2 expression has also been shown to be critical in mitochondrial homeostasis and cell survival in RA synovial fibroblasts [11]. Bcl-xL is an anti-apoptotic homologue of Bcl-2 [12] and has been shown to enhance the survival of immature B cells in transgenic mice [13]. Human peripheral blood memory B cells have been found to co-express high levels of Bcl-2 and Bcl-xL, and this may contribute to B-cell survival [14]. There is also evidence that Bcl-xL plays a role in the protection of synovial cells from apoptosis [15]. Human peripheral B cells were found to up-regulate expression of Bcl-xL when co-cultured with a stromal cell line derived from RA synovium and, consequently, were protected from apoptosis. This protection of B cells from apoptosis was blocked by the use of antibodies to vascular cell adhesion molecule 1 (VCAM-1), which is expressed on the stromal cells. Hence, signals from stromal cells appear to regulate B-cell apoptosis in the microenvironment of the rheumatoid joint. CD40-activated human B cells have also been found to up-regulate Bcl-xL expression, protecting the cells from Fas-mediated apoptosis [16]. More recent work has demonstrated that Bcl-xL also plays a part in the survival of activated macrophages in inflammatory conditions [17].
The aim of this study is to compare the expression of Bcl-xL in RA and OA synovium in vivo, and to determine the relationship, if any, between Bcl-xL expression and other variables such as patient age and disease duration.
Materials and methods
Tissues
Synovial tissue was obtained from RA (n=20) and OA (n=10) patients who were undergoing elective joint replacement, after a protocol approved by the Ethics Committee of Cork University Hospital. Informed consent was obtained and patients fulfilled American College of Rheumatology criteria. Synovium for reverse transcriptase polymerase chain reaction (RT-PCR) and Western blot analysis was flash-frozen in liquid nitrogen and stored at −80°C. Synovium for immunohistochemistry was placed in formaldehyde before processing. Sixteen of 17 patients in the RA group were seropositive (rheumatoid factor status not recorded in three cases). The median disease duration was 11 years (range 6 months–40 years), and the median number of DMARDs used was 2 (range 0–4).
Histology and immunohistochemistry
Using a microtome, 5-μm-thick sections were cut from blocks of paraffin-embedded synovium. Sections were deparaffinised in xylene for 10 min and were rehydrated in an alcohol gradient. Antigen retrieval was by microwave irradiation at 750 W in citrate buffer, pH 6.0, until it boiled and then at 100 W for 15 min. Sections were immunostained with a Bcl-xL-specific rabbit polyclonal antibody (Oncogene, CN Biosciences, Nottingham, UK) at a dilution of 1:1,000, followed by incubation with a biotinylated goat anti-rabbit secondary antibody (Vector, Burlingame, CA, USA). Slides were then incubated with an avidin–biotin–peroxidase complex (Vector) for 30 min at room temperature. Antibody binding was localised using diaminobenzidine and sections were counterstained with Mayer’s haematoxylin (Sigma, St. Louis. MO, USA). Negative controls were performed by omitting the primary antibody. Consecutive sections were stained for plasma cells with a monoclonal antibody specific for CD138 at a 1:1,000 dilution.
The immunostained sections were examined to determine the distribution of Bcl-xL staining. Samples were initially examined to quantify the degree of lining hyperplasia. To examine the relationship between Bcl-xL expression and synovial inflammation, an inflammatory score (0–5) was assigned to each sample on the basis of the number of inflammatory infiltrates seen in each biopsy specimen under ×10 magnification. Tissue characteristics and inflammatory scores are shown in Table 1. The number of positive-staining cells in the synovial lining was quantified for both RA and OA and expressed as a percentage of the total lining cells. Subsynovial expression of Bcl-xL was graded using a modified Lindblad–Hedfors scoring system [18].
Reverse transcriptase polymerase chain reaction
Bcl-xL mRNA was detected using RT-PCR. RT-PCR for the housekeeping gene β-actin was performed as a positive control. RNA was extracted using an RNA extraction kit (Qiagen, West Sussex, UK). Complementary DNA (cDNA) was synthesised using random hexamer primers and AMV reverse transcriptase (both Promega, Madison, WI, USA). PCR was performed using the following sense and antisense primers: Bcl-xL—ACAGCCCCGCGGTGAATGG and TGCCCCGCCGAAGGAGAAA, and β-actin—GTGGGGCGCCCCAGGCACCA and CTCCTTAATGTCACGCACGATTTC. The PCR products for Bcl-xL and β-actin were 593 and 560 bp, respectively. Thermal cycling was as follows: denaturation at 96°C for 15 s, annealing at 55°C for 30 s and extension at 72°C for 3 min. Thirty-two cycles were performed for the Bcl-xL PCR and 35 cycles for the β-actin control. Primers were used at a final concentration of 0.1 μM, deoxynucleotide tri-phosphates at 50 μM and MgCl2 at 1.5 mM. One unit of Taq DNA polymerase was used per 50 μl of reaction mixture. PCR products were resolved by electrophoresis on a 2% agarose gel and viewed under ultraviolet illumination after staining with ethidium bromide. A 100-bp DNA size ladder (Promega) was used to establish product size.
Western blot analysis
Frozen synovial tissue was placed in a lysis buffer containing 50 mM Tris (pH 8.0), 5 mM EDTA, 1% Nonidet P-40, 0.5 mM phenylmethyl sulphonyl fluoride, 0.25% sodium dodecyl sulphate, 0.5 mM dithriothreitol, 1 μg/ml leupeptin, 10 u/ml aprotinin and 10 μg/μl of soyabean trypsin inhibitor, and was then immediately homogenised with a probe sonicator. Samples were centrifuged to remove particulate debris. Protein concentrations of the lysates were determined using the bicinchoninic acid protein assay (Pierce, Rockford, IL, USA). Equivalent amounts of protein for each specimen were electrophoresed through a 12% sodium dodecyl sulphate (SDS)-polyacrylamide gel and transferred by a semi-dry method (Hoefer SemiPhor, Pharmacia Biotech, San Francisco, CA, USA) onto a nitrocellulose membrane. The membranes were immersed in blocking buffer (5% dried milk to 0.1% TBS-Tween) overnight at 4°C and were then incubated with a Bcl-xL-specific goat polyclonal IgG antibody (Santa Cruz Biotechnology, CA) at a dilution of 1:100 for 3 h at room temperature. Washed membranes were incubated with a horseradish peroxidase-conjugated secondary anti-goat IgG antibody (1:2,000, Dako, Carpenteria, CA, USA). Washing between incubations was carried out using 0.1% TBS-Tween. Immunoreactive products were detected using chemiluminescence reagent (Amersham Pharmacia Biotech, Buckinghamshire, UK) and exposed to autoradiography film. Pre-stained low range molecular weight sodium dodecyl sulphate-polyacrylamide gel electrophoresis standards were used to determine protein size (Bio-rad, Hercules, CA, USA).
Statistical analysis
Differences between the RA and OA groups were examined for statistical significance using the Mann–Whitney two-sample test. Correlations were determined using Spearman’s correlation coefficient (r s). p<0.05 was considered to be significant.
Results
Bcl-xL was expressed in the synovial lining of both RA and OA, but there was significantly more Bcl-xL expression in the rheumatoid synovial lining. There was no significant difference, however, in the degree of Bcl-xL expression between the subsynovium in RA samples and that in OA samples. There was a significant correlation between the subsynovial expression of Bcl-xL and the number of inflammatory cells in the subsynovium (r s=0.376, p< 0.05). Age and disease duration did not correlate with Bcl-xL expression. Subsynovial Bcl-xL was found predominantly in the mononuclear inflammatory infiltrates. Histological examination (×100) showed many of these positive cells to be plasma cells. CD138 staining for plasma cells on consecutive sections confirmed that plasma cells accounted for much of the positive Bcl-xL staining seen in the RA samples (Fig. 1). Expression of Bcl-xL was also noted in endothelial cells in both RA and OA samples (Fig. 1).
Bcl-xL expression in OA and RA synovium. Sections of synovium were stained with a Bcl-xL-specific polyclonal antibody at a dilution of 1:1,000. Positively stained cells are brown (arrowed). Negative controls were performed by omitting the primary antibody (not shown). a and b Bcl-xL staining in OA and RA (×20 ). c and d Expression of Bcl-xL in plasma cells in RA synovium. CD138 staining for plasma cells in RA synovium is shown in c (×10) with Bcl-xL staining in a consecutive section in d (×100). e and f Endothelial staining for Bcl-xL in RA and OA synovium (×100 and ×63, respectively)
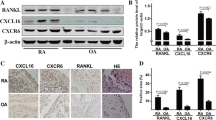
Expression of Bcl-xL mRNA in synovial samples from RA (n=7) and OA (n=7) patients was analysed using RT-PCR. Bcl-xL mRNA was expressed in all synovial samples, and there was no significant difference in the level of Bcl-xL mRNA expression between specimens derived from patients with RA and OA (Fig. 2). Western blot analysis was performed to qualitatively assess the expression of Bcl-xL protein in both RA and OA. Western blotting revealed significant expression of Bcl-xL at the protein level in three out of four RA samples, with no Bcl-xL protein detected in the three OA specimens at equivalent protein loading concentrations (Fig. 3).
Western blot analysis for Bcl-xL. Immunoblotting was carried out using a Bcl-xL-specific IgG antibody. Bcl-xL expression was demonstrated in three out of the four RA samples (lanes 1, 3, 5 and 7), but there was no detectable Bcl-xL expression in the three OA samples at equivalent protein concentrations (lanes 2, 4 and 6)
Discussion
Defects in apoptosis in RA have been detected in the signalling molecules (Fas, TNF and p53) [19, 20] and also in the regulatory pathways; for example, the Bcl-2 family [20]. Increased Bcl-2 expression in RA synovial fibroblasts, for example, is associated with reduced apoptosis and enhanced fibroblast survival [21]. Fas and FasL are expressed in synoviocytes, monocytes and lymphocytes in rheumatoid synovium; however, despite coexpression of Fas and FasL, apoptosis is detected in only 1% of these cells in RA [21].
In the present study, Bcl-xL expression was detected in RA and OA in the synovial lining and stroma, and also in inflammatory cells and endothelial cells, using immunohistochemistry. There was significantly more Bcl-xL protein expressed in the synovial lining in the RA samples compared to OA synovium. There was also a significant correlation between the expression of subsynovial Bcl-xL and the number of inflammatory cells in the subsynovium. Disease duration or patient age did not correlate with the amount of Bcl-xL expressed. Qualitative evaluation using Western blotting showed increased Bcl-xL protein expression in the RA samples relative to OA controls (Fig. 3), which correlates with the higher inflammatory score for the RA samples. Immunohistochemistry for CD138 revealed that a large proportion of the Bcl-xL-positive cells were plasma cells (Fig. 2).
Evidence from in vitro work supports the hypothesis that Bcl-xL contributes to the survival of cells in RA synovium. Stromal cells isolated from RA synovium have been shown to protect co-cultured B cells from cell death by up-regulating Bcl-xL expression in the B cells [15]. This up-regulation of Bcl-xL appears to be mediated by the expression of VCAM-1 on the stromal cells, which cross-links with VLA-4 (very late antigen 4) on the B cells. It has been shown that synoviocytes cultured in vitro support the survival of co-cultured B cells and also induce the terminal differentiation of B cells into plasma cells, with high levels of intracytoplasmic immunoglobulins [22]. Up to 2% of synovial plasma cells in RA are bilobed [23], suggesting local proliferation of plasma cells; there is also evidence that plasma cells have a prolonged survival time in rheumatoid synovium [24]. In this study, many of the Bcl-xL-expressing cells were noted to be plasma cells morphologically and by staining of consecutive sections with an antibody for the plasma cell marker CD138. Up-regulation of Bcl-xL may be a mechanism by which plasma cell survival is prolonged in rheumatoid synovium.
Plasma cells in the synovial fluid of patients with seropositive RA have been found to produce IgM rheumatoid factor (RF), and the microenvironment in the joint is thought to favour RF production [25]. Although the precise role of RF in the aetiology of RA is not clear, there is an association between high-titre RF and disease severity [26, 27]. As well as producing autoantibodies, IgG-producing plasma cells have been found to secrete TNF-α in chronic diseases such as rheumatoid arthritis and polyarteritis nodosa [28]. Bcl-xL is up-regulated in malignant plasma cells in patients with myeloma [29], and a similar mechanism may account for the abnormal persistence of plasma cells in rheumatoid synovium.
Synovial fluid T cells have been found to up-regulate the expression of Bcl-xL, possibly contributing to their longevity in synovial fluid. It has also been found that the pro-apoptotic protein Bax is overexpressed relative to Bcl-xL in the synovium of patients with numerous apoptotic cells; however, this was not the case in synovium with few apoptotic cells, as detected using terminal deoxynucleotidyl transferase-mediated dUTP nick-end labelling technique [30]. A further study found marked colocalization of Bax and Bcl-xL in RA synovium which was associated with a low rate of apoptotic cells, again suggesting that the ratio of Bcl-2 homologues is important in RA synovium [31].
In conclusion, our results show that RA is associated with elevated expression of the anti-apoptotic protein, Bcl-xL, in the synovial lining and also in inflammatory cells, particularly plasma cells. Increased expression of Bcl-xL may contribute to the survival and proliferation of inflammatory cells, including plasma cells, in rheumatoid synovium, and Bcl-xL may be a potential therapeutic target in RA.
References
Yamamura Y, Gupta R, Morita Y et al (2001) Effector function of resting T cells: activation of synovial fibroblasts. J Immunol 166:2270–2275
Zvaifler NJ, Boyle D, Firestein GS (1994) Early synovitis-synoviocytes and mononuclear cells. Semin Arthritis Rheum 23:11–16
Rudin CM, Thompson CB (1997) Apoptosis and disease: regulation and clinical relevance of programmed cell death. Annu Rev Med 48:267–281
Kerr JF, Wyllie AH, Currie AR (1972) Apoptosis: a basic biological phenomenon with wide-ranging implications in tissue kinetics. Br J Cancer 26:239–257
Nagata S, Golstein P (1995) The Fas death factor. Science 267:1449–1456
Nakajima T, Aono H, Hasunuma T et al (1995) Apoptosis and functional Fas antigen in rheumatoid arthritis synoviocytes. Arthritis Rheum 38:485–491
Firestein GS, Yeo M, Zvaifler NJ (1995) Apoptosis in rheumatoid arthritis synovium. J Clin Invest 96:1631–1638
Gross A, McDonnell JM, Korsmeyer SJ (1999) BCL-2 family members and the mitochondria in apoptosis. Genes Dev 13:1899–1911
Basanez G, Zhang J, Chau BN et al (2001) Pro-apoptotic cleavage products of Bcl-xL form cytochrome c-conducting pores in pure lipid membranes. J Biol Chem 276:31083–31091
Korsmeyer SJ (1999) BCL-2 gene family and the regulation of programmed cell death. Cancer Res 59:1693s–1700s
Perlman H, Georganas C, Pagliari LJ, Koch AE, Haines K 3rd, Pope RM (2000) Bcl-2 expression in synovial fibroblasts is essential for maintaining mitochondrial homeostasis and cell viability. J Immunol 164:5227–5235
Kharbanda S, Pandey P, Schofield L et al (1997) Role for Bcl-xL as an inhibitor of cytosolic cytochrome C accumulation in DNA damage-induced apoptosis. Proc Natl Acad Sci U S A 94:6939–6942
Fang W, Weintraub BC, Dunlap B et al (1998) Self-reactive B lymphocytes overexpressing Bcl-xL escape negative selection and are tolerized by clonal anergy and receptor editing. Immunity 9:35–45
Bovia F, Nabili-Tehrani AC, Werner-Favre C, Barnet M, Kindler V, Zubler RH (1998) Quiescent memory B cells in human peripheral blood co-express bcl-2 and bcl-x(L) anti-apoptotic proteins at high levels. Eur J Immunol 28:4418–4423
Hayashida K, Shimaoka Y, Ochi T, Lipsky PE (2000) Rheumatoid arthritis synovial stromal cells inhibit apoptosis and up-regulate Bcl-xL expression by B cells in a CD49/CD29-CD106-dependent mechanism. J Immunol 164:1110–1116
Zhang X, Li L, Choe J et al (1996) Up-regulation of Bcl-xL expression protects CD40-activated human B cells from Fas-mediated apoptosis. Cell Immunol 173:149–154
Lakics V, Medvedev AE, Okada S, Vogel SN (2000) Inhibition of LPS-induced cytokines by Bcl-xL in a murine macrophage cell line. J Immunol 165:2729–2737
Lindblad S, Hedfors E (1985) Intraarticular variation in synovitis. Local macroscopic and microscopic signs of inflammatory activity are significantly correlated. Arthritis Rheum 28:977–986
Yamanishi Y, Firestein GS (2001) Pathogenesis of rheumatoid arthritis: the role of synoviocytes. Rheum Dis Clin North Am 27:355–371
Mountz JD, Hsu H, Matsuki Y, Zhang H (2001) Apoptosis and rheumatoid arthritis: past, present, and future directions. Curr Rheumatol Rep 3:70–78
Matsumoto S, Muller-Ladner U, Gay RE, Nishioka K, Gay S (1996) Ultrastructural demonstration of apoptosis, Fas and Bcl-2 expression of rheumatoid synovial fibroblasts. J Rheumatol 23:1345–1352
Dechanet J, Merville P, Durand I, Banchereau J, Miossec P (1995) The ability of synoviocytes to support terminal differentiation of activated B cells may explain plasma cell accumulation in rheumatoid synovium. J Clin Invest 95:456–463
Perry ME, Mustafa Y, Wood SK, Cawley MI, Dumonde DC, Brown KA (1997) Binucleated and multinucleated forms of plasma cells in synovia from patients with rheumatoid arthritis. Rheumatol Int 17:169–174
Berek C, Kim HJ (1997) B-cell activation and development within chronically inflamed synovium in rheumatoid and reactive arthritis. Semin Immunol 9:261–268
Reparon-Schuijt CC, van Esch WJ, van Kooten C, Levarht EW, Breedveld FC, Verweij CL (1998) Functional analysis of rheumatoid factor-producing B cells from the synovial fluid of rheumatoid arthritis patients. Arthritis Rheum 41:2211–2220
Drossaers-Bakker KW, Zwinderman AH, Vlieland TP et al (2002) Long-term outcome in rheumatoid arthritis: a simple algorithm of baseline parameters can predict radiographic damage, disability, and disease course at 12-year followup. Arthritis Rheum 47:383–390
Bukhari M, Lunt M, Harrison BJ, Scott DG, Symmons DP, Silman AJ (2002) Rheumatoid factor is the major predictor of increasing severity of radiographic erosions in rheumatoid arthritis: results from the Norfolk Arthritis Register Study, a large inception cohort. Arthritis Rheum 46:906–912
Di Girolamo N, Visvanathan K, Lloyd A, Wakefield D (1997) Expression of TNF-alpha by human plasma cells in chronic inflammation. J Leukoc Biol 61:667–678
Tu Y, Renner S, Xu F et al (1998) BCL-X expression in multiple myeloma: possible indicator of chemoresistance. Cancer Res 58:256–262
Sioud M, Mellbye O, Forre O (1998) Analysis of the NF-kappa B p65 subunit, Fas antigen, Fas ligand and Bcl-2-related proteins in the synovium of RA and polyarticular JRA. Clin Exp Rheumatol 16:125–134
Hilbers I, Hansen T, Petrow PK et al (2003) Expression of the apoptosis accelerator Bax in rheumatoid arthritis synovium. Rheumatol Int 23:75–81
Acknowledgement
The authors have declared no competing interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Busteed, S., Bennett, M.W., Molloy, C. et al. Bcl-xL expression in vivo in rheumatoid synovium. Clin Rheumatol 25, 789–793 (2006). https://doi.org/10.1007/s10067-005-0191-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-005-0191-0