Abstract
The objective of this study was to determine bone mineral density (BMD) distribution in ankylosing spondylitis (AS) using quantitative computed tomography (QCT), to study bone turnover and anterior pituitary and gonadal hormonal axis in AS, and to look for correlations between BMD, bone remodeling markers and gonadal and anterior pituitary hormones. Forty-three male consecutive patients with AS were enrolled prospectively [mean (SD) age of 36.4 (11.3) years (range: 17–67) and mean disease duration of 6.8 (5.2) years (range: 0.4–19)]. Spine BMD was measured in all patients by QCT, and the results were compared to 29 male patients undergoing lumbar CT scan for sciatica. Bone turnover and anterior pituitary and gonadal axis were assessed in 29 patients, and the results were compared to 30 male healthy blood donors. The mean (SD) BMD was 127.7 mg/cm3 (48.9) (range: 8.8–265.7) and 152.1 (25.3) (range: 34.2–190.4) in patients and controls, respectively (p=0.018). Patients had lower serum levels of osteocalcin and higher levels of serum testosterone, luteinizing hormone (LH), and prolactin than controls with a significant statistical difference. There was a positive significant statistical correlation between BMD and chest expansion, Schober’s test, C7-wall distance, and negative significant statistical correlation with age, disease duration, Bath Ankylosing Spondylitis Metrology Index (BASMI), Bath Ankylosing Spondylitis Radiology Index (BASRI), and serum prolactin. No correlation was observed between bone turnover parameters and AS symptomatic and structural severity indexes. BMD is lower with increasing age and late and severe disease. Decreased bone formation with normal resorption and increased levels of serum prolactin may be involved in its pathophysiology.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ankylosing spondylitis (AS) is a chronic rheumatic disorder affecting with predilection young males and characterized by inflammation of the enthesis (especially of the axial skeleton) and sometimes the joints, which may lead to ankylosis [1–5]. Extra-articular manifestations may involve in particular the eyes, heart, gut, and lungs [6, 7]. Osteoporosis (OP) has been described in AS even in early stages of the disease and may be responsible for vertebral fractures, especially late in the course of the disease [8–12]. Fractures of the spine occur with relatively minor trauma and are associated with substantial mortality and neurological morbidity [13–16]. The severity of this OP has been difficult to characterize using older bone mineral density (BMD) measurement techniques. Single photon BMD studies failed to show appendicular OP. Dual energy X-ray absorptiometry (DXA) studies revealed loss of BMD of the vertebrae in early disease but not in advanced disease. DXA is a safe and accurate tool to measure BMD at different skeletal sites. However, it provides information on bone mineral content (g) using a single projection and the content is adjusted to the area of the visualized vertebral bodies to give an estimate of apparent areal density (g/cm2). As a consequence, the lumbar spine BMD increases with the disease duration, which was explained by the appearance of syndesmophytes following advanced enthesopathy and interapophyseal joint and interpedicular ankylosis. By contrast, quantitative computed tomography (QCT) permits assessment of BMD of purely trabecular components of vertebral bone, independent of the cortical shell, the lateral or posterior element, or calcification artefacts. Therefore, QCT remains the only method able to accurately assess spine OP in patients with advanced AS [17, 18].
However, the mechanism and etiology of this OP are still controversial. The study of bone turnover parameters also led to controversial results and it has still not been clarified whether this OP is related to increased bone resorption, decreased bone formation, or both. Among the multiple etiological factors suggested in AS OP, hormonal dysfunction especially of the gonadal axis has been incriminated. It is also well known that several endocrinopathies may induce OP (e.g., hyperprolactinemia). To test the hypotheses that patients with AS have a lower BMD than normal and that this low BMD may be related to hormonal dysfunction, we carried out this study with the objectives of determining BMD distribution in AS using QCT, studying bone turnover and anterior pituitary and gonadal hormonal axis in AS, and looking for correlations between BMD, bone remodeling markers, and gonadal and anterior pituitary hormones.
Material and methods
Patients
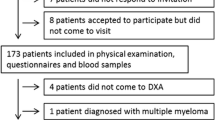
Consecutive male patients meeting the modified New York criteria for AS [19] and attending our department in a 1-year period were enrolled. Consent was obtained from all patients. Exclusion criteria were liver and kidney diseases, renal stones, diabetes, alcoholism, parathyroid and thyroid diseases, and treatment with anticonvulsants. Clinical assessment included demographic data [age, gender, weight, height, body mass index (BMI: kg/m2)], and duration of disease defined as the time between the date of first symptoms and patient enrolment. Disease symptomatic severity was measured by Schober’s index, Bath Ankylosing Spondylitis Metrology Index (BASMI) [20], Bath Ankylosing Spondylitis Functional Index (BASFI) [21], and Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) [22]. Data on treatment with nonsteroidal anti-inflammatory drugs (NSAIDs) and/or steroids were collected.
BMD assessment
Vertebral trabecular BMD (mg/cm3) was determined for the lumbar spine using QCT (Siemens Somatom, Siemens, Erlangen, Germany). Four scans of 10-mm thickness were carried out through the L1–L4 vertebral bodies at the midportions parallel to the end-plates. Simultaneous pixel calibration was performed using a mineral-equivalent reference phantom placed beneath the patient during scanning. In our hands, short-term in vivo coefficient of variation of BMD measurements in young subjects is 1% (data not shown).
Radiological assessment
X-rays of the pelvis and lumbar spine were read by one of us (AEM). Sacroiliitis and hip involvement were assessed on anteroposterior pelvic X-rays and graded respectively on New York and Bath Ankylosing Spondylitis Radiology Index (BASRI) hip scales [23, 24]. Global spine radiological involvement was measured by the Bath Ankylosing Spondylitis Radiological Score (BASRI-spine) [25].
Biological assessment
Biological and clinical assessments were performed on the same day. All samples were taken in the early morning. Blood was collected in vacutainers without additive. After centrifugation at 1500 g for 10 min, serum was aliquoted and stored at −20°C. Serum concentrations of calcium, phosphorus, alkaline phosphatases, serum albumin, and erythrocyte sedimentation rate (ESR) were measured by standard methods. Serum osteocalcin, crosslaps (C-telopeptide, CTx), parathyroid hormone (PTH), total testosterone, estrogen, prolactin, follicle-stimulating hormone (FSH), and luteinizing hormone (LH) were measured in 29 patients and 30 controls using electrochemiluminescence on an Elecsys 2010 analyzer (Roche Diagnostics, Mannheim, Germany).
Controls
The control group for BMD measurement consisted of 29 young male patients who underwent lumbar spine CT scan for sciatica [mean age 36.2 (SD 10.7), range: 26–47] and for biological exams of 30 young male blood donors [mean age 35.9 (SD 10.2), range: 20–45]. The controls were age matched to the patients. The exclusion criteria were the same as for the patient group. None of them had a history of inflammatory rheumatic disease or a condition responsible for bone loss.
Statistical analysis
This cross-sectional study was conducted in different steps. The first step consisted of the description of the study population. In the second step, we compared BMD and biological data in patients and controls using Student’s t-test as all data had a normal distribution. In the third step, we looked for correlations between BMD and age, disease duration, AS symptomatic and structural severity parameters, and biological data using Pearson’s correlation coefficient. Results were considered to be significant when p values were less than 0.05.
Results
Forty-three male patients were recruited. Results are expressed as mean (SD) and range. The mean age of the study population was 36.4 (11.3) years (range: 17–67) and the mean disease duration was 6.8 (5.2) years (range: 0.4–19). Demographic, clinical, and radiological variables for the 43 patients are shown in Table 1. All patients had AS without an associated condition. None of the patients had taken steroids in the 6 months before the study.
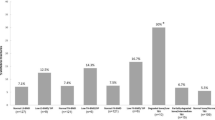
The mean (SD) BMD was 127.7 mg/cm3 (48.9) (range: 8.8–265.7) and 152.1 (25.3) (range: 34.2–190.4) in patients and controls, respectively (p=0.018) as shown in Fig. 1. No differences between patients and controls were observed in serum calcium, phosphorus, creatinine, albumin, PTH, CTx, estrogen, FSH, and urinary calcium. Patients had lower serum levels of osteocalcin and higher levels of serum testosterone, LH, and prolactin than controls with a significant statistical difference (Table 2).
There was a positive significant statistical correlation between BMD and chest expansion, Schober’s test, C7-wall distance, and negative significant statistical correlation with age, disease duration, BASMI, BASRI, and serum prolactin (Table 3). No correlation was observed between bone turnover parameters and AS symptomatic and structural severity indexes.
Discussion
Our study confirms that a high proportion of patients with AS have lumbar spine low bone mass. It showed that BMD is lower with increasing age and in patients with late and severe disease. Our patients were young adults with early disease (36 years old and 6 years of disease duration on average), and this low BMD is a relevant risk factor for fractures with increasing age. In this study, none of our patients had vertebral compression fracture. However, only lumbar spine X-rays were studied and were assessed without any morphometric method as it has been done in some studies. In the literature, fracture frequency ranges from 0 to 19%. The risk of spinal fracture is increased in long-standing AS because the fused spine has often become osteoporotic and is vulnerable to trauma. The risk of severe neurological impairment (and thus mortality) is related to the site of the fracture.
In contrast with most of the studies on the same topic, we used QCT to assess the lumbar spine OP. It is now well established that DXA is not useful for evaluating axial bone mass in patients with advanced AS as BMD increases with the appearance of bridging syndesmophytes and facet joint and interpedicular ankylosis. Our study demonstrated clearly that BMD is lower in patients with higher BASRI-spine scores and confirms that QCT is the best technique for assessing OP in patients with advanced AS as it has already been shown by Devogelaer et al. [17] and Lee et al. [11]. QCT was among the earliest BMD measurements to become widely available for diagnostic and serial assessment of OP. The technique has a good reproducibility (1–5%) and may be performed using standard body CT scanners [26]. However, high costs and particularly high radiation dose (100–1000 mRem) are generally regarded as disadvantages.
Osteoporosis is now a well-recognized feature of AS. One of us, using DXA, has already demonstrated evident OP and/or osteopenia in about half of a group of patients with AS [27]. The follow-up of these patients showed that loss of bone continued only in those with persistent active disease [28] as has been communicated by Gratacos et al. [29]. However, the etiology of this OP is still the subject of discussion. The studies of bone turnover parameters led to controversial results [30, 31]. The noninvasive assessment of bone turnover has improved markedly in the past few years with the development of specific and sensitive markers such as serum bone-specific alkaline phosphatase and osteocalcin for bone formation and urinary excretion of bone type I collagen degradation products: pyridinium crosslink (pyridinoline and deoxypyridinoline)-associated peptides for bone resorption [32, 33]. Recently, serum C-telopeptide levels have been shown to be effective in evaluating bone resorption. In our study, we used serum osteocalcin to assess bone formation and serum CTx levels to determine resorption. The results were in favor of decreased bone formation with normal bone resorption.
Osteoporosis has been observed in other inflammatory diseases, without steroid use, such as rheumatoid arthritis [34, 35]. Moreover, significant statistical correlations have been observed between bone remodeling markers and inflammation, as assessed by ESR or C-reactive protein (CRP). The inflammatory mediators, several of which have a local or systemic action on bone turnover, have been incriminated. Enthesis and synovial inflammation in active AS may lead to the release of cytokines [interleukin (IL)-1, IL-6, tumor necrosis factor (TNF)] and nitric oxide, which have recently been shown to induce OP in an animal model [36]. Recently, subclinical gut inflammation was pointed out as a possible participating factor in the pathophysiology of OP in AS [37, 38]. Deficits in sex hormone secretion have been suggested by some authors as a possible etiology, but our study revealed higher levels of testosterone in patients than in controls as was the case in several studies [39–43]. Conflicting reports of testosterone levels in AS have been published, and it seems that NSAIDs, especially phenylbutazone, may cause spurious elevation in testosterone levels [44]. In our study, all of the patients were using NSAIDs but no one was taking phenylbutazone. It is fair to say that the present data in patients with AS are too limited to suggest a role for androgens in the pathophysiology of the OP observed in AS, but a role in the initiation and the early stages of AS cannot be excluded. Cross-sectional studies cannot clearly distinguish causal relation from secondary disease effects, because blood sampling to test these hypotheses only takes place many years after the onset of disease.
High serum levels of prolactin have never been incriminated in the pathophysiology of OP in AS. Our study suggests that it can play a role in bone loss in AS as it was more frequently observed in patients than in controls and was negatively correlated to BMD. None of our patients used antipsychotics or had adenoma or any condition able to explain the high levels of serum prolactin. Hyperprolactinemia has been reported in Reiter’s disease and other spondyloarthropathies [45]. In autoimmune diseases, it is not clear whether prolactin has a causal role or whether the elevation of prolactin in some patients is a sort of stress response secondary to the disease. It has been demonstrated that proinflammatory stimulation of the central nervous system by circulating cytokines or depressed mood can increase serum prolactin [46–48]. The common denominator is increased hypothalamic serotonin secretion which stimulates pituitary prolactin release [49, 50]. Due to its many immunostimulatory effects in vivo and in vitro, this hormone could play a proinflammatory role in autoimmune diseases [51–56] and AS. Some reported positive effects of prolactin antagonistic therapy with bromocriptine, which may indicate that prolactin has a role for disease modulation [57–60]. The cause of OP is most likely multifactorial with contributions from genetics, inflammation, medications, subclinical gut inflammation, hormonal dysfunction, and limited mobility as the disease progresses.
In summary, our study confirms that patients with AS have lower spine bone mass than age-matched controls. This OP which is more pronounced in patients with advanced disease can be evaluated accurately only by QCT in these types of patients. It also suggests that this OP may be related to decreased bone formation rather than increased bone resorption and points out the role of hyperprolactinemia in its pathophysiology. However, further studies including larger series are needed to better clarify the mechanisms of OP involved in AS.
Take home message
In AS, BMD is lower with increasing age and late and severe disease. Decreased bone formation with normal resorption and increased levels of serum prolactin may be involved in its pathophysiology.
References
Calin A, Taurog J (1998) Spondylarthritides. Oxford University Press, New York, pp 1–347
van der Linden SJ, van der Heijde D (1998) Ankylosing spondylitis. Rheum Dis Clin North Am 24:663–915
Yu D (2000) Spondylarthropathies. In: Ruddy S, Harris ED, Sledge CB (eds) Kelley’s textbook of rheumatology, 6th edn. W.B. Saunders, Philadelphia, pp 1039–1053
Khan MA (ed) (1992) Spondyloarthropathies. W.B. Saunders, Philadelphia
El Maghraoui A, Bensabbah R, Bahiri R, Bezza A, Guédira N, Hajjaj-Hassouni N (2003) Cervical spine involvement in ankylosing spondylitis. Clin Rheumatol 22:94–98
El Maghraoui A, Chaouir S, Tabache F, Abouzahir A, Bezza A, Ghafir D, Ohayon V, Archane MI (2003) High resolution thoracic CT in ankylosing spondylitis. Ann Rheum Dis 62:185–186
Bezza A, El Maghraoui A, Ghadouane M, Tabache F, Abouzahir A, Abbar M, Ghafir D, Ohayon V, Archane MI (2002) Idiopathic retroperitoneal fibrosis and ankylosing spondylitis. A new case report. Joint Bone Spine 69:502–505
Will R, Palmer R, Bhalla AK, Ring F, Calin A (1989) Osteoporosis in early ankylosing spondylitis. A primary pathological event? Lancet 2:1483–1485
Hansen CA, Shagrin JW, Duncan H (1971) Vertebral osteoporosis in ankylosing spondylitis. Clin Orthop 74:59–64
Raltson SH, Urquhart GDK, Bzeski M, Sturrock RD (1990) Prevalence of vertebral compression fractures due to osteoporosis in ankylosing spondylitis. Br Med J 300:563–565
Lee YSL, Schlotzhauer T, Ott SM, van Vollenhoven RF, Hunter J, Shapiro J, Marcus R, McGuire JL (1997) Skeletal status of men with early and late ankylosing spondylitis. Am J Med 103:233–241
Donnelly S, Doyle DV, Denton A, Rolfe J, McCloskey EV, Spector TD (1994) Bone mineral density and vertebral compression fracture rates in ankylosing spondylitis. Ann Rheum Dis 53:117–121
Cooper C, Carbone L, Michet CJ, Atkinson EJ, O’Fallon WM, Melton LJ (1994) Fracture risk in patients with ankylosing spondylitis: a population based study. J Rheumatol 21:1877–1882
Khan MA, Lai J-H, Chang D-M, Liu H-C (1993) Recognizing and managing fractures in ankylosing spondylitis. J Musculoskelet Med 1:45–57
Fox MW, Onofrio BM, Kilgore JE (1993) Neurological complications of ankylosing spondylitis. J Neurosurg 78:871–878
Lehtilen K (1993) Mortality and causes of death in 398 patients admitted to hospital with ankylosing spondylitis. Ann Rheum Dis 52:174–176
Devogelaer J-P, Maldague B, Malghem J, Nagant de Deuxchaisnes C (1992) Appendicular and vertebral bone mass in ankylosing spondylitis. Arthritis Rheum 35:1062–1067
El Maghraoui A (2004) Osteoporosis and ankylosing spondylitis. Bone Joint Spine 71:573–578
Van der Linden S, Valkenburg HA, Cats A (1984) Evaluation of diagnostic criteria for ankylosing spondylitis. A proposal for modification of the New York criteria. Arthritis Rheum 4:361–368
Jenkinson TR, Mallorie PA, Whitelock HC, Kennedy LG, Garrett SL, Calin A (1994) Defining spinal mobility in ankylosing spondylitis. The Bath Ankylosing Spondylitis Metrology Index (BASMI). J Rheumatol 21:1694–1698
Calin A, Garrett S, Whitelock HC et al (1994) A new approach to defining functional ability in ankylosing spondylitis: the development of the Bath Ankylosing Spondylitis Functional Index. J Rheumatol 21:2281–2285
Garrett SL, Jenkinson T, Kennedy LG, Whitelock HC, Gaisford P, Calin A (1994) A new approach to defining disease status in ankylosing spondylitis: the Bath Ankylosing Spondylitis Disease Activity Index. J Rheumatol 21:2286–2291
Bennet PH, Burch TA (1967) New York symposium on population studies in the rheumatic diseases: new diagnostic criteria. Bull Rheum Dis 28:453–458
MacKay K, Brophy S, Mack C, Doran M, Calin A (2000) The development and validation of a radiographic grading system for the hip in ankylosing spondylitis: the bath ankylosing spondylitis radiology hip index. J Rheumatol 27:2866–2872
MacKay K, Mack C, Brophy S, Calin A (1998) The Bath Ankylosing Spondylitis Radiology Index (BASRI): a new, validated approach to disease assessment. Arthritis Rheum 41:2263–2270
Lang TF, Li J, Harris ST, Genant HK (1999) Assessment of vertebral bone mineral density using volumetric quantitative CT. J Comput Assist Tomogr 23:130–137
El Maghraoui A, Borderie D, Edouard R, Roux C, Dougados M (1999) Osteoporosis, body composition and bone turnover in ankylosing spondylitis. J Rheumatol 26:2205–2209
Maillefert JF, Aho S, El Maghraoui A, Dougados M, Roux C (2001) Changes in bone density in patients with ankylosing spondylitis: a two year follow-up study. Osteoporos Int 12:605–609
Gratacos J, Collado A, Pons F, Osaba M, Sanmarti R, Roqué M, Larroza M, Munoz-Gomez J (1999) Significant loss of bone mass in patient with early, active ankylosing spondylitis. A follow-up study. Arthritis Rheum 42:2319–2324
Marhoffer W, Stracke H, Masoud H et al (1995) Evidence of impaired cartilage/bone turnover in patients with active ankylosing spondylitis. Ann Rheum Dis 54:556–559
MacDonald AG, Birkinshaw G, Durham B, Bucknall RC, Fraser WD (1997) Biochemical markers of bone turnover in seronegative spondylarthropathy: relationship to disease activity. Br J Rheumatol 36:50–53
Brandt J, Frederiksen JK, Jensen CH, Teisner B (2001) The N– and C-telopeptides of human procollagen type I (PINP and PICP): molecular heterogeneity and assay technology. In: Eastell R, Baumann M, Hoyle NR, Wieczorek L (eds) Bone markers. Biochemical and clinical perspectives. Martin Dunitz, London, pp 73–82
Yilmaz N, Ozaslan J (2000) Biochemical bone turnover markers in patients with ankylosing spondylitis. Clin Rheumatol 19:92–98
Gough A, Lilley J, Eyre S, Holder RL, Emery P (1994) Generalized bone loss in patients with early rheumatoid arthritis. Lancet 344:23–27
Laan RFJM, Buijs WCAM, Verbeek ACM et al (1993) Bone mineral density in patients with recent onset rheumatoid arthritis: influence of disease activity and functional capacity. Ann Rheum Dis 52:21–26
Armour KE, Van’T Hof RJ, Grabowski PS, Reid DM, Ralston SH (1999) Evidence for a pathogenic role of nitric oxide in inflammation-induced osteoporosis. J Bone Miner Res 14:2137–2142
Szeijfeld VL, Moniier-Faugere MC, Bognar BJ, Ferraz MB, Malluche BJ (1997) Systemic osteopenia and mineralization defect in ankylosing spondylitis. J Rheumatol 24:683–688
El Maghraoui A, Dougados M, Freneaux E, Chaussade S, Amor B, Breban M (1999) Concordance between abdominal scintigraphy using technetium-99m hexamethylpropylene amine oxime-labelled leucocytes and ileocolonoscopy in patients with spondyloarthropathies and without clinical evidence of inflammatory bowel disease. Rheumatology 38:543–546
Gooren LJ, Giltay EJ, van Schaardenburg D, Dijkmans BA (2000) Gonadal and adrenal sex steroids in ankylosing spondylitis. Rheum Dis Clin North Am 26:969–987
Mitra D, Elvins DM, Collins AJ (1999) Testosterone and testosterone free index in mild ankylosing spondylitis: relationship with bone mineral density and vertebral fractures. J Rheumatol 26:2414–2417
Straub RH, Struharova S, Scholmerich J, Harle P (2002) No alterations of serum levels of adrenal and gonadal hormones in patients with ankylosing spondylitis. Clin Exp Rheumatol 20 [6 Suppl 28]:S52–S59
Giltay EJ, Popp-Snijders C, van Schaardenburg D, Dekker-Saeys BJ, Gooren LJ, Dijkmans BA (1998) Serum testosterone levels are not elevated in patients with ankylosing spondylitis. J Rheumatol 25:2389–2394
Giltay EJ, van Schaardenburg D, Gooren LJ, Popp-Snijders C, Dijkmans BA (1999) Androgens and ankylosing spondylitis: a role in the pathogenesis? Ann N Y Acad Sci 876:340–364
Giltay EJ, Popp-Snijders C, van Denderen JC, van Schaardenburg D, Gooren LJ, Dijkmans BA (2000) Phenylbutazone can spuriously elevate unextracted testosterone assay results in patients with ankylosing spondylitis. J Clin Endocrinol Metab 85:4923–4924
Tapia-Serrano R, Jimenez-Balderas FJ, Murrieta S, Bravo-Gatica C, Guerra R, Mintz G (1991) Testicular function in active ankylosing spondylitis. Therapeutic response to human chorionic gonadotrophin. J Rheumatol 18:841–848
Jara LJ, Silveira LH, Cuellar ML, Pineda CJ, Scopelitis E, Espinoza LR (1994) Hyperprolactinemia in Reiter’s syndrome. J Rheumatol 21:1292–1297
Spangelo BL, Judd AM, Isakson PC, MacLeod RM (1989) Interleukin-6 stimulates anterior pituitary hormone release in vitro. Endocrinology 125:575–577
el Halawani ME, Youngren OM, Silsby JL, Phillips RE (1988) Involvement of serotonin in prolactin release induced by electrical stimulation of the hypothalamus of the turkey (Meleagris gallopavo). Gen Comp Endocrinol 72:323–328
Willoughby JO, Menadue MF, Liebelt HJ (1988) Activation of 5-HT 1 serotonin receptors in the medial basal hypothalamus stimulates prolactin secretion in the unanaesthetized rat. Neuroendocrinology 47:83–87
Pavasuthipaisit K, Norman RL, Spies HG (1980) Evidence that serotonin is involved in prolactin release by electrical stimulation of the medial basal hypothalamus in the rhesus monkey. Neuroendocrinology 31:256–260
Athreya BH, Rafferty JH, Sehgal GS, Lahita RG (1993) Adenohypophyseal and sex hormones in pediatric rheumatic diseases. J Rheumatol 20:725–730
Pauzner R, Urowitz MB, Gladman DD, Gough JM (1994) Prolactin in systemic lupus erythematosus. J Rheumatol 21:2064–2067
Ostendorf B, Fischer R, Santen R, Schmitz-Linneweber B, Specker C, Schneider M (1996) Hyperprolactinemia in systemic lupus erythematosus? Scand J Rheumatol 25:97–102
Buskila D, Lorber M, Neumann L, Flusser D, Shoenfeld Y (1996) No correlation between prolactin levels and clinical activity in patients with systemic lupus erythematosus. J Rheumatol 23:629–632
Neidhart M (1996) Elevated serum prolactin or elevated prolactin/cortisol ratio are associated with autoimmune processes in systemic lupus erythematosus and other connective tissue diseases. J Rheumatol 23:476–481
Blanco-Favela F, Quintal-Alvarez G, Leanos-Miranda A (1999) Association between prolactin and disease activity in systemic lupus erythematosus. Influence of statistical power. J Rheumatol 26:55–59
McMurray RW, Weidensaul D, Allen SH, Walker SE (1995) Efficacy of bromocriptine in an open label therapeutic trial for systemic lupus erythematosus. J Rheumatol 22:2084–2091
Blank M, Krause I, Buskila D et al (1995) Bromocriptine immunomodulation of experimental SLE and primary antiphospholipid syndrome via induction of nonspecific T suppressor cells. Cell Immunol 162:114–122
Figueroa FE, Carrion F, Martinez ME, Rivero S, Mamani I (1997) Bromocriptine induces immunological changes related to disease parameters in rheumatoid arthritis. Br J Rheumatol 36:1022–1023
Alvarez-Nemegyei J, Cobarrubias-Cobos A, Escalante-Triay F, Sosa-Munoz J, Miranda JM, Jara LJ (1998) Bromocriptine in systemic lupus erythematosus: a double-blind, randomized, placebo-controlled study. Lupus 7:414–419
Eulry F, Mayaudon H, Bauduceau B, Lechevalier D, Crozes P, Magnin J, Claude-Berthelot C (1996) Prolactine sérique sous l’effet de la protireline au cours des spondylarthropathies. Essai de traitement de 4 cas d’arthrite réactionnelle et 2 cas de rhumatisme psoriasique par la bromocriptine. Ann Med Interne (Paris) 147:15–19
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
El Maghraoui, A., Tellal, S., Chaouir, S. et al. Bone turnover markers, anterior pituitary and gonadal hormones, and bone mass evaluation using quantitative computed tomography in ankylosing spondylitis. Clin Rheumatol 24, 346–351 (2005). https://doi.org/10.1007/s10067-004-1039-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-004-1039-8