Abstract
Patients suffering from hip osteoarthritis (OA) are frequently symptomatic, and the disease can result in significant limitation of patients’ activity and high social costs. Hip OA is generally managed with systemic treatments such as nonsteroidal anti-inflammatory drugs (NSAIDs) and/or symptomatic slow acting drugs. Viscosupplementation with hyaluronan (HA) or its derivatives, which aims to restore the physiological and rheological features of the synovial fluid to improve symptoms, is now a routinely prescribed treatment for OA of the knee. However, few data exist in the literature regarding the use of viscosupplementation in the treatment of hip OA. The objective of this prospective, open, uncontrolled pilot study was to investigate the safety and effectiveness of intra-articular injection, under ultrasound control, of hylan G-F 20 for the treatment of OA of the hip. Twelve patients (≥40 years old) with symptomatic hip OA were treated with one injection of 2 ml of hylan G-F 20 under ultrasound guidance. During the study, patients were evaluated for safety and efficacy using the Lequesne index, a visual analogue scale (VAS) measure of hip OA pain and analysis of NSAID consumption. Patients treated with hylan G-F 20 in this study showed clinically significant reductions in Lequesne and VAS scores and in the consumption of NSAIDs up to 3 months after the injection. In the 12 patients treated (total of 14 injections), no systemic adverse events were observed. Three patients reported mild, local pain post-injection. This study demonstrates the potential of ultrasound-guided intra-articular injections of a viscosupplement into the hip joint and gives positive preliminary information about the safety and efficacy of hylan G-F 20 for the treatment of symptomatic hip OA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
According to epidemiological and statistical data, osteoarthritis (OA) assumes the predominant social role amongst all rheumatic diseases. OA represents 9.4% of all pathologies and causes frequent transitory or permanent invalidity. The hip joint is often affected by the disease with an incidence estimated to be approximately equivalent to that of the knee, the most commonly affected joint in OA [1]. Patients suffering from hip OA are frequently symptomatic, and the disease causes significant limitations in individuals’ activities, and incurs high social costs. United States epidemiological studies reveal that total hip arthroplasty (THA) consumes approximately 2.5% of the total healthcare budget per year, without considering the costs associated with concurrent pharmacological medication [2]. This percentage grows significantly with the addition of costs associated with rehabilitation programmes and the management of complications.
Hip OA, according to the American College of Rheumatology (ACR) guidelines, is generally treated by systemic treatments such as nonsteroidal anti-inflammatory drugs (NSAIDs) and/or symptomatic slow acting drugs [2]. The ACR guidelines for the treatment of knee OA include the use of viscosupplementation, which aims to restore the physiological and rheological features of the synovial fluid [1]. Viscosupplementation involves the intra-articular (IA) injection of hyaluronan, a naturally occurring polymer present in the synovial fluid, or its derivatives. Hylan G-F 20 (Synvisc, Genzyme Biosurgery, Cambridge, Mass., USA) has been shown to have an excellent safety and efficacy profile as a viscosupplement for the symptoms associated with OA of the knee [3–7).
Few data exist in the literature on the use of viscosupplementation in the treatment of hip OA [8–11]. One of the limiting factors for this practice might be related to the injection procedure. Intra-articular injection of the hip is not as easy as for the knee, mainly due to the anatomical features of the joint and the proximity of “sensitive” structures such as the femoral artery and nerves. Even though hip injection may be performed “blindly” the failure rate is significant [12], and when using a slowly absorbed polymer such as hyaluronan the potential local complications may jeopardise the therapeutic benefit [13]. For these reasons, it has been recommended to perform IA injection of the hip under fluoroscopic or ultrasound control. Ultrasound guidance is used by us [14] and other authors [9]. The objective of this pilot study was to investigate the safety and the effectiveness of IA injection of hylan G-F 20 under ultrasound guidance for the treatment of the symptoms associated with OA of the hip.
Materials and methods
Study design
The trial was an open, prospective pilot study. All patients were required to sign a written informed consent form before entering the trial. Eligibility criteria:
-
Male or female of at least 40 years of age
-
Symptomatic hip OA according to ACR criteria [15] with Kellgren-Lawrence radiographic grades II, III or IV [16]
-
X-rays should have been taken not earlier than 2 months before patient enrollment
-
OA of at least 2 years duration
-
No previous IA injection
Exclusion criteria:
-
Concomitant anticoagulant therapy (to avoid potential haemorrhagic complications following the injection)
-
Absence of articular space on X-ray
-
Concomitant steroid therapy
-
Significant rheumatological comorbidity (e.g. connective tissue diseases)
-
Any previous history of hyaluronan therapy
Each patient was treated with one injection of 2 ml of hylan G-F 20 (a 6 million average molecular weight, cross-linked hyaluronan derivative). Each patient was followed up for 3 months from the IA injection, and he/she underwent four study visits; the first at baseline, the second at the time of injection, the third at 1 month after injection and the final visit at 3 months after the injection.
During each visit, patients were evaluated using:
-
1.
Lequesne index [17]
-
2.
Measure of individual hip OA pain in the previous week on a 100-mm visual analogue scale (VAS) [18]
-
3.
Consumption of NSAIDs by measuring the number of days a month the patient had used NSAIDs during the previous month
Throughout the study period, any adverse events reported by patients were registered and monitored.
Injection technique
Patients underwent hip injection under ultrasound control as described previously [14]. Briefly, the patient was examined supine with the hip in internal rotation of 15–20°. A 7.5-MHz linear or 3.5-MHz convex transducer (Star 256, Hitachi-Esaote, Genoa, Italy) was used with a sterile biopsy guide attached (Fig.1). The hip joint was scanned using an anterior parasagittal approach, lateral to the femoral vessels. The transducer was aligned with the long axis of the femoral neck, including the acetabulum and the femoral head.
Patient is examined supine with the hip in slight internal rotation (15–20°). A 7.5-MHz linear or 3.5-MHz convex transducer is used with a sterile biopsy guide attached. Hip joint is scanned by an anterior parasagittal approach, lateral to the femoral vessels. The transducer is aligned with the long axis of the femoral neck. Intra-articular injection is performed by inserting a 20 gauge (9 cm) spinal needle through the biopsy guide
IA injection was performed by inserting a 20 gauge (9 cm) spinal needle through the biopsy guide, using an anterosuperior approach. Then, utilising real-time biopsy guidance software, the needle was advanced into the anterior capsular recess, at the level of the femoral head. Once the needle came into contact with the femoral head, the needle was retracted by 1 mm. Then hylan G-F 20 was injected into the hip joint. IA placement was verified with real-time monitoring (direct visualisation of viscous fluid) (Fig.2) and power Doppler imaging (flow signals in the IA recess). The colour Doppler view prevented the inadvertent injection of blood vessels.
Statistics
The t-test was performed at month 1 and month 3 versus baseline.
Results
Patient population
Twelve patients were enrolled who met the inclusion criteria, ten of whom had unicompartmental OA and two of whom had bilateral OA. Patient baseline data are summarised in Table 1. The average age of the patients enrolled was 69.7 years and the average hip OA pain VAS score was 78 mm at baseline. Eleven patients were taking NSAIDs. Two patients suffered from concurrent depressive syndromes, one patient had knee OA and cognitive impairment and one had malignant haematological disease. A total of 14 injections were performed, as the two patients affected by bilateral OA received an injection in each hip.
Efficacy data
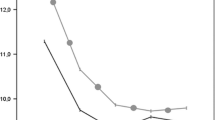
Eight subjects had a sustained improvement in Lequesne scores for more than 3 months with an average reduction of 15% at the 3rd month. Figure 3 shows the average Lequesne scores at each time point. A reduction of 2.7 points at the 1st month and 3.1 points at the 3rd month, equal to 12 and 15% respectively, was observed. These differences versus baseline were statistically significant.
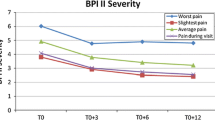
With regard to hip OA pain VAS scores, all patients reported a reduction of pain at 1 and 3 months after the IA injection, with the exception of one patient who did not experience any clinical benefit and whose VAS score increased at 3 months. A statistically significant difference was found at each time point compared to baseline, but there was no significant difference between the 1- and 3-month time points after injection (Fig. 4).
The consumption of NSAIDs reduced by 65.6% at 1 month and this effect was maintained at the 3-month visit with a reduction of 56.1% in comparison to the month before injection. These differences were statistically significant as shown in Fig. 5. Only one patient did not reduce NSAID consumption, potentially due to the pain of concurrent haemopathy. Two patients returned to baseline levels of NSAID consumption at 3 months and one patient maintained the decreased level of NSAID consumption at 3 months.
Safety data
No systemic adverse events were observed. Three local adverse events were reported and described as a mild, transient sensation of pain and heaviness in the injected joint. These complications lasted for an average of 2–4 days; no medication was required and daily activity was unaffected. No septic complications were reported.
Discussion
In the last 10 years rigorous clinical studies have demonstrated the safety and efficacy of IA injections of hyaluronan in symptomatic knee OA. High molecular weight hyaluronan derivatives (hylan G-F 20) were shown to bear greater similarity to endogenous healthy synovial fluid and demonstrated clinical superiority over placebo in clinical studies with a dosing regimen of three injections of 2 ml [3, 4].
Few data exist on the use of viscosupplementation in hip OA. The present study demonstrates the safety and efficacy of hylan G-F 20, injected under ultrasound control [14], for the treatment of hip OA. The data from this pilot study are similar to those from previous studies in which one or two injections of 2 ml injected intra-articularly under fluoroscopy were used [10, 11], giving additional evidence that hylan G-F 20 may be useful in treating symptomatic hip OA.
The use of ultrasound guidance may help to avoid the possibility of side effects because the hip joint is adjacent to anatomic structures that could be seriously damaged by a blind injection. Fluoroscopy allows introduction of the needle into the joint space but does not allow identification and avoidance of vascular and nervous structures; on the contrary, continuous sonographic monitoring is able to reveal the presence of vessels and nerves in addition to needle placement. Direct evidence of hylan G-F 20 fluid inside the joint can be also revealed during the injection on the screen. Ultrasound guidance contrary to fluoroscopic techniques does not require use of contrast, allowing use in patients intolerant to iodised contrasts. It can be repeated without problems of radiation load to either the operator or the patient. Moreover, it is more economic and faster in comparison to fluoroscopic guidance. Considering the above, we believe that, even if fluoroscopy or computed tomography (CT) guidance can, on occasion, be employed, nevertheless for general use physicians should use ultrasound.
The limited number of patients enrolled in this study precludes any definitive conclusion about safety and efficacy. However, the 12 patients treated with hylan G-F 20 showed a clinically significant reduction of Lequesne and VAS pain scores. Such improvement lasted for at least 3 months in 75% of the patients after the administration of only one injection of 2 ml of hylan G-F 20. The small number of patients enrolled in this pilot study made it impossible to identify any difference in response between patients of differing radiological grades of OA, or between patients with baseline high and low Lequesne score. Therefore questions remain about the predictability of the response to hylan G-F 20. However, comorbidity seems to reduce the efficacy of the therapy, as seen in two patients in this study (one malignant haemopathy and one depressive syndrome). Nevertheless our data, even though inadequately powered, seem to have detected two subgroups: responders and nonresponders.
Furthermore, there was a significant reduction in NSAID consumption, which should encourage broader consideration of the cost/benefit of a combination of such therapies. The reduction in NSAID consumption is not only an important clinical achievement, but also a significant health economic consideration [2]. Not only direct costs (NSAID purchasing) are saved, but also the indirect costs associated with the management of NSAID-associated side effects (gastrointestinal bleeding, arterial hypertension, renal and cardiac failure, hospitalisation etc.).
The safety data confirm good local tolerability and the absence of any serious or systemic effects. This was partly due to the safe and effective technique used for the IA injection. This study highlights that hip viscosupplementation may be particularly useful in patients with localised illness and/or in whom NSAIDs are contraindicated, as is often the case in elderly patients. Moreover, using an ultrasound-controlled IA injection technique can certainly make the provision of treatment safer, simpler and relatively inexpensive. Taking into consideration the limited number of subjects and the scarcity of published scientific literature, our data require corroboration from larger, prospective, placebo-controlled, double-blind trials. Further studies are also warranted to address the ideal dosing regimen of hylan G-F 20, the definition of a responder population and to establish the average duration of clinical benefit.
References
Altman RD, Hochberg MC, Moskowitz RW, Schnitzer TJ (2000) Recommendations for the medical management of osteoarthritis of the hip and knee. Arthritis Rheum 43:1905–1915
Sturkenboom MC, Romano F, Simon G, Correa-Leite ML, Villa M, Nicolosi Á, Borgnolo G, White-Porro G, Mannino S (2002) The iatrogenic costs of NSAID therapy: a population study. Arthritis Rheum 47:132–140
Wobig M, Dickhut A, Maier R, Vetter G (1998) Viscosupplementation with hylan G-F 20: a six-month controlled trial of efficacy and safety in the osteoarthritic knee. Int J Drug Ther 20:410–423
Dickson DJ, Hosie G, English JR et al (2001) A double-blind, placebo-controlled comparison of hylan G-F 20 against diclofenac in knee osteoarthritis. J Clin Res 4:41–52
Lussier A, Cividino AA, McFarlane CA, Olszynski WP, Potashner WJ, de Medicis R (1996) Viscosupplementation with hylan for the treatment of osteoarthritis: findings from clinical practice in Canada. J Rheumatol 23:1579–1585
Marshall KW (1997) The current status of hylan therapy for the treatment of osteoarthritis. Today’s Ther Trends 15:99–108
Raynauld JP, Torrance GW, Band PA, Goldsmith CH, Tugwell P, Walker V, Schultz M, Bellamy N (2002) A prospective, randomized, pragmatic health outcomes trial evaluating the incorporation of hylan G-F 20 into the treatment paradigm for patients with knee osteoarthritis (Part 1 of 2): clinical results. Osteoarthritis Cartilage 10:506–517
Bragantini Á, Molinaroli F (1994) A pilot clinical evaluation of the treatment of hip osteoarthritis with hyaluronic acid. Curr Ther Res Clin Exp 55:319–330
Qvistgaard E, Kristoffersen H, Terslev L, Danneskiold-Samsoe B, Torp-Pedersen S, Bliddal H (2001) Guidance by ultrasound of intra-articular injections in the knee and hip joints. Osteoarthritis Cartilage 9:512–517
Brocq O, Tran G, Breuil V, Grisot C, Flory P, Euller-Ziegler L (2002) Hip osteoarthritis: short-term efficacy and safety of viscosupplementation by hylan G-F 20. An open-label study in 22 patients. Joint Bone Spine 69:388–391
Conrozier T, Bertin P, Mathieu P, Charlot J, Bailleul F, Trèves R et al (2003) Intra-articular injections of hylan GF-20 in patients with symptomatic hip osteoarthritis: an open-label, multi-centre pilot study. Clin Exp Rheumatol 21:605–610
Jones A, Regan M, Ledingham J, Pattrick M, Manhire A, Doherty M (1993) Importance of placement of intra-articular steroid injections. BMJ 307:1329–1330
Jackson DW, Evans NA, Thomas BM (2002) Accuracy of needle placement into the intra-articular space of the knee. J Bone Joint Surg Am 84A: 1522–1527
Migliore A, Martin Martin LS, Alimonti A et al (2003) Efficacy and safety of viscosupplementation by ultrasound-guided intra-articular injection in osteoarthritis of the hip. Osteoarthritis Cartilage 11:305–306
Altman R, Alarcon G, Appelrouth D, Bloch D, Borenstein D, Brandt K et al (1991) The American College of Rheumatology criteria for the classification and reporting of osteoarthritis of the hip. Arthritis Rheum 34:505-514
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteoarthrosis. Ann Rheum Dis 16:494-502
Lequesne MG (1997) The algofunctional indices for hip and knee osteoarthritis. J Rheumatol 24:779–781
Scott-Huskisson EC (1976) Graphic representation of pain. Pain 2:175–184
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Migliore, A., Tormenta, S., Martin, L.S.M. et al. Open pilot study of ultrasound-guided intra-articular injection of hylan G-F 20 (Synvisc) in the treatment of symptomatic hip osteoarthritis. Clin Rheumatol 24, 285–289 (2005). https://doi.org/10.1007/s10067-004-1009-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-004-1009-1