Abstract
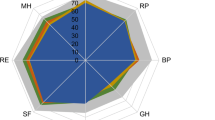
The aim of this study was to evaluate health-related quality of life (HR-QOL) in patients with systemic sclerosis (SSc), to compare it with that of patients with rheumatoid arthritis (RA), and to correlate it with other parameters. HR-QOL was evaluated by the Short Form 36 (SF-36), SSc disease activity and severity by preliminary indexes recently proposed, disability by the Health Assessment Questionnaire (HAQ), and depressive symptoms by the Beck Depression Inventory. HR-QOL perception was not statistically different in patients with SSc and RA, except that patients with diffuse cutaneous involvement had worse scores in the general health and mental health dimensions than patients with RA (p=0.03). Compared with RA, patients with SSc tended to perceive less bodily pain (p=0.06) and have less disability (p=0.04) but to report higher depressive symptom scores (p=0.05). SSc patients’ HR-QOL was associated with some disease severity scales (general, kidney and, less significantly, heart), but it was poorly correlated with the other evaluated disease activity and severity indexes. A strong correlation with disability and with depressive symptoms was observed. In conclusion, patients with SSc perceived a reduced HR-QOL similar to that of patients with RA. SF-36 may provide useful information in their evaluation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The importance of psychological factors in modifying the influence of chronic rheumatic diseases such as systemic sclerosis (SSc) on the affected individuals is increasingly recognized [1]. In particular, everybody who is involved in the care of these patients is aware of the dramatic impact that the presence of this disease has on their health-related quality of life (HR-QOL).
Since patients’ perception of their health status is poorly assessed by physicians [2], there is consensus that in monitoring chronic diseases, most importance should be given to subjective accounts of health. Instruments such as the Short Form 36 (SF-36), a general health status questionnaire describing the impact of the disease in terms of patient-centered outcomes [3], have been proven to allow reliable assessment of HR-QOL in the general population [4] and across diverse patient groups [5, 6], including several rheumatic disorders [6, 7, 8, 9, 10, 11, 12, 13, 14, 15]. However, not much information is available on the HR-QOL of patients with SSc [16, 17, 18].
Using the SF-36 questionnaire, we have evaluated the HR-QOL in a series of 76 consecutive patients with SSc and its association with demographic and disease characteristics (e.g., duration, subset). These patients were compared with patients suffering from another autoimmune rheumatic disease, rheumatoid arthritis (RA). This disease was chosen because it shares many similarities with SSc, including chronicity and difficulty in diagnosis and cure. Moreover, RA was used for comparison in other studies evaluating HR-QOL in diseases such as Sjögren’s syndrome, fibromyalgia, and psoriatic arthritis [13, 14]. Finally, correlations of SSc patients’ HR-QOL with disease activity and severity indexes, as well as with loss of functional status (i.e., disability), and depressive symptoms were sought.
Methods
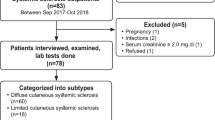
Patients
SSc and RA were defined by American College of Rheumatology (ACR) criteria [19, 20]. Patients with SSc were classified as limited or diffuse SSc (lSSc, and dSSc, respectively) according to the criteria of LeRoy [21]. During a 3-month period, all consecutive patients with SSc or RA attending our outpatient clinic for periodic controls, or daycare facility for infusion therapies (with iloprost or infliximab, respectively), were asked to answer self-administered questionnaires. Only one patient with SSc refused to participate in the study. Two patients with RA were unable to answer the questionnaires. Four incomplete questionnaires were discarded. The final response rate was 97%.
Quality of life
Quality of life was evaluated by an Italian version of the SF-36 [22]. This questionnaire contains 36 items, measuring health on eight dimensions: general health perception, physical and social functioning, role limitations by physical or emotional problems, mental health, vitality, and bodily pain. For each dimension items are coded, summed, and transformed on to a scale from 0 (worst health) to 100 (best health).
Functional status
Functional status was evaluated by the Health Assessment Questionnaire (HAQ). This questionnaire contains 20 items, each assessed on a 0 (lack of disability) to 3 (complete disability) scale. These are divided into eight domains; the highest scores in each of the eight domains are summed and divided by 8 to calculate the general disability index [23].
Depressive symptoms
Depressive symptoms were assessed by the Beck Depression Inventory (BDI). This questionnaire contains 21 items, each assessed on a 0 (lack of depressive symptoms) to 3 (severe depressive symptoms) scale [24]. Thirteen items concern “cognitive-affective” symptoms such as changes in mood and self-worth, hopelessness, and suicidal feelings, whereas eight items concern “somatic” symptoms such as appetite loss, sleep disturbance, etc. The items are summed to obtain total depression score on a 0 to 63 scale. A separate analysis of “cognitive-affective” and “somatic” items was also performed.
SSc disease severity
SSc disease severity was evaluated by the preliminary Mesdger scales [25]. These are nine individual organ system scales graded from 0 (no documented involvement) to 4 (endstage disease). To complete the evaluation of the disease severity scales, history, physical examination, and laboratory analysis at the time of the visit were considered. Chest radiography, lung function test and carbon monoxide diffusion capacity (DLCO), electrocardiogram, and echocardiogram were performed at least annually in all patients and the last available results were considered. Esophageal motility was evaluated in 66 patients by manometry at the start of the follow-up and periodically afterwards only in patients with residual motility. A small bowel hypomotility study was performed only when clinically indicated. The gastrointestinal (GI) tract severity scale in the present study therefore reliably only concerns esophageal involvement. Moreover, many data of the scales concerning joint/tendon and muscle disease severity were not collected in our patients. Therefore, these scales were not considered in our study.
SSc disease activity
SSc disease activity was measured by the preliminary indexes recently proposed by a European multicenter study [26]. These include three indexes, one for the whole series of patients with SSc and one each for dSSc and lSSc patients, respectively, graded on a 0 (no activity) to 10 (maximal activity) scale.
RA disease activity
RA disease activity was measured by the Disease Activity Score (DAS), which, as originally proposed in 1990 by van der Heijde et al. [27], evaluates 44 joints and is now therefore also called DAS44.
Statistical analysis
Data are expressed as the median (25th-75th percentile). The Mann-Whitney nonparametric test was used for comparisons between groups. The chi-squared test was used for comparisons of proportions. Spearman’s rank correlation coefficients were calculated to determine the strength of the relationship between variables.
Results
Patients
The main demographic, clinical, and laboratory characteristics of patients with SSc and RA participating in the study are presented in Table 1. The only differences between disease groups were a higher prevalence of females and a higher use of benzodiazepines among the patients with SSc. Of note, separate analysis by gender did not disclose any difference in HR-QOL or depressive symptoms either in patients with SSc or RA (data not shown). SSc-specific disease activity and severity indexes are shown in Table 2. RA disease activity was measured by the DAS44: median score was 2.37 (1.92–3.23). These data reflect the fact that around 50% of the patients with RA evaluated in this study had low disease activity and most of the others had moderate disease activity. These results were obtained with aggressive treatments: as shown in Table 1, 32 patients (27%) were treated with tumor necrosis factor blocking agents and 35 (30%) with combinations of disease-modifying antirheumatic drugs (DMARDs).
HR-QOL
As shown in Table 3, the subscales of the SF-36 did not differ significantly in the groups of patients with dSSc and lSSc. A separate analysis was also performed comparing patients attending the daycare facility to receive periodic treatment with iloprost (34 for ischemic ulcers and 2 for pulmonary hypertension) and 40 outpatients: the only difference found was a significant reduction of the score concerning the “social functioning” items in daycare patients vs outpatients [62.5 (46.9–90.6) vs 93.75 (75–100), p=0.003]. This observation probably reflects the interference of periodical admission in daycare for prolonged, and sometimes not well tolerated, infusion therapy on patients’ social life [28].
Patients with SSc were therefore pooled together for comparisons with patients with RA. No significant difference was observed between the two groups (Table 3): there was a trend for patients with SSc to have less bodily pain than those with RA and, on the contrary, to have a lower perception of their general health and mental health. The latter observations concern particularly the subset of patients with dSSc. In fact, this group of patients had significantly lower scores in these subscales than patients with RA (general health: p=0.03, mental health: p=0.03).
Functional status
Figure 1 shows that patients with dSSc had more disability, evaluated by the HAQ index, than patients with lSSc [1.38 (0.88–2.03) vs 0.50 (0–1.12), p=0.001]. Analogously, patients with SSc admitted in daycare had a higher disability index than outpatients [1.06 (0.59–1.68) vs 0.25 (0–1.12), p=0.001].
As shown in Fig. 1, functional status, in the total group of SSc, was slightly less compromised than in RA [0.88 (0.12–1.38) vs 1.00 (0.50–1.75), p=0.04]. In patients with SSc, questions on scales influenced by hand function, such as “reaching” and “gripping,” had the highest scores, but were nevertheless (not significantly) lower than in RA. On the contrary, patients with RA had more disability in the scales of “hygiene” (p=0.001), “dressing” (p=0.04), and “activity” (p=0.02).
Depressive symptoms
The BDI questionnaire, used to evaluate the presence of depressive symptoms, contains 21 items, 13 concerning “cognitive-affective” symptoms, and 8 concerning “somatic” complaints. A high correlation between the two sets of items was found in patients with SSc (r s=0.77, p<0.0001), reflecting the interrelationship between patients’ emotional status and the physical symptoms evaluated by the questionnaire.
The BDI score in patients with SSc was not strictly related to the subset of disease [dSSc: 17 (8.75–22.5) vs lSSc: 11 (5.75–20), p=0.08], but a significant difference was found comparing patients receiving iloprost therapy in daycare with the outpatients with SSc [17 (10.75–24.75) vs 8 (4.75–18.25), p=0.003].
As shown in Fig. 2, patients with SSc had more depressive symptoms than patients with RA [13 (7–20.25) vs 9 (6–15.5), p=0.05]: the scores were moderately higher in the items assessing cognitive-affective symptoms of depression [6 (2–12) vs 4.5 (2–8), p=0.07] as well in those assessing somatic symptoms [6.5 (3–9.25) vs 5 (3–8), p=0.08].
Correlation of SF-36 items with other variables
HR-QOL perceived by patients with SSc was not significantly correlated with age and disease duration (not shown). A significant correlation was observed between all the dimensions of SF-36 and some disease severity scales (general and kidney, Table 4). Some dimensions of SF-36 were significantly correlated also with the heart disease severity scale, whereas no correlation was found with other disease severity scales (peripheral vascular, skin, GI tract, lung, data not shown). Severity indexes on joint/tendon and muscle disease were not evaluated in our study.
Also the disease activity indexes were poorly associated with HR-QOL perception: only the correlation with the vitality and social functioning dimensions had statistical significance (Table 4; similar data were found using the indexes specific for dSSc and lSSc, not shown).
Perception of HR-QOL was significantly correlated both with disability (HAQ score) and with depressive symptoms (BDI score) (Table 4). Single subscales of the SF-36 investigate specifically areas similar to those assessed by these questionnaires: in particular, the Mental Health subscale overlaps with the BDI, and the Physical Function subscale overlaps with the HAQ. As predicted, these correlations were found to have the highest coefficients, thus demonstrating the reliability of the SF-36 as measures of these health status dimensions in patients with SSc. However, the physical function dimensions (and the other subscales exploring the physical component of HR-QOL perceived by patients with SSc) were highly correlated not only with disability, but also with the depressive symptoms, even with the score exploring only symptoms concerning the cognitive-affective area (not shown). This correlation could not be explained by overlaps between the two questionnaires and showed that our patients who reported more symptoms, considered “pure” expression of depression, tended to have also a poorer perception of their “physical” HR-QOL. Vice versa, the dimensions of the SF-36 exploring the mental component of HR-QOL were highly correlated not only with the BDI, but also with the HAQ, confirming the interrelationship between disability, depressive symptoms, and HR-QOL in SSc.
Discussion
The SF-36 is an instrument whose validity and reliability have been demonstrated across different medical conditions, but information on its use to measure HR-QOL in patients with SSc is limited [16, 17, 18]. A formal validation of the SF-36 in SSc was beyond of the aim of the present study. However, its validity was suggested by the fact that the predicted strict relationships among single subscales of SF-36 and specific measures providing similar information, observed in other diseases, were confirmed also in patients with SSc.
It was fortunate that the two groups of patients evaluated in our study were well matched for demographic and socioeconomic characteristics, as well as for disease duration. Disease characteristics of the patients reflect the selection criteria: they were consecutive individuals evaluated at the outpatient clinic (with a daycare facility for infusion therapies) of a university hospital. Given the relatively short time of recruitment (3 months) and considering our policy of controlling patients with less severe disease with longer time intervals, there might have been a slight bias toward more severe cases. This may be reflected by the relatively high proportion of SSc patients receiving iloprost or RA patients receiving anti TNF.
Our data showed that the HR-QOL perceived by patients with SSc is similar to that of patients with RA, evaluated in the same period and in the same clinic. In our experience, the only small differences observed between RA patients and SSc patients suggested that individuals with SSc and diffuse cutaneous involvement may perceive some dimension of their HR-QOL as even worse than RA patients do. Since several papers demonstrated, either in community- or hospital-based studies, that RA patients experience a decreased HR-QOL as compared with healthy individuals [10, 12, 13, 14, 15], our findings confirmed a previous observation describing the HR-QOL of patients with SSc as significantly lower than that of a healthy control population [18].
We looked for variables significantly associated with HR-QOL in SSc patients. The observed correlation should not be interpreted as causal relationships, but the obtained results might help to identify the patients with worst perception of their HR-QOL. Considering that the roles of general demographic parameters (gender, age) and disease characteristics (subset, duration) were not significant, associations with disease activity and severity, disability and depressive symptoms were studied in more detail.
A correlation was observed between some disease severity indexes (general, kidney and, albeit less significantly, heart) and the dimensions of the SF-36 (Table 4). These data suggested that the subsets of patients with these severe manifestations of SSc experience a particular reduction of their HR-QOL. However, it should be noted that these indexes were raised only in a minority of our patients (Table 2), and therefore this subset of patients was small in our study. Moreover, the disease activity scales were not significantly correlated with most SF-36 dimensions. We can therefore conclude that, in our experience, the indexes assessing disease severity and activity were poorly associated with patients’ perception of HR-QOL.
A reduced HR-QOL in our patients with SSc was significantly associated with indexes evaluating disability and depressive symptoms. These two scales were highly intercorrelated (not shown). However, they were differentially associated with specific dimensions of HR-QOL, suggesting that they did not measure the same thing. The interrelationship among depressive symptoms and disability is likely to be potentially bidirectional, and perhaps sometimes a sort of vicious circle can contribute to reduce patients’ perception of HR-QOL.
The strict correlation between the disability measured by the HAQ and the SF-36 in patients with SSc was already described [18]. Moderate-to-severe disability is frequent in SSc and it correlates with diffuse skin involvement and with other clinical manifestations of the disease such as digital ulcers, heart and kidney involvement, hand contractures, and muscle weakness [23, 29, 30]. Our study confirmed the association of high disability with the dSSc subset, with digital ulcers, and (not shown) with heart and kidney involvement. The utility of the HAQ in the assessment of patients with SSc was demonstrated by studies reporting that it can predict outcome and survival in these patients [31]. However, the HAQ questionnaire does not cover psychological and social areas, i.e., dimensions that have a profound influence on the perception of QOL.
Surprisingly, not much information is available on the psychological impact of SSc, a disease that may be perceived as somehow mysterious, disfiguring, difficult to diagnose and cure [1]. Our study confirms previous reports that, using the BDI questionnaire, showed that depressive symptoms are rather common in patients with SSc [32, 33]. The rates of patients with SSc experiencing depressive symptoms have not been compared with groups with other illnesses in other studies. However, pain and disability are considered the most important factors contributing to symptoms of depression [1, 33], and these are common also in other chronic rheumatic diseases [34]. It is therefore of interest that our experience suggested that the depressive symptom score in sclerodermic patients is higher than in patients who have RA (Fig. 2), even if they tend to experience less bodily pain (Table 3) and have a lower disability index than in RA (Fig. 1). Factors other than pain and disability are therefore likely to play particularly important roles influencing the symptoms of depression in sclerodermic patients. The relevance of social and familial adjustment to the disease has been demonstrated in previous studies [32, 35]. Moreover, body image dissatisfaction is particularly great in these patients [36] and may be the cause of further depression [1]. Whatever the causes, the problem of depressive symptoms in SSc may be underestimated by clinicians, as suggested by the low number of our patients receiving antidepressant drugs or psychotherapy.
In conclusion, our experience suggests that the SF-36 may be a valid instrument to measure HR-QOL also in patients with SSc and that it is likely that disability and depression are better predictors of subjective HR-QOL than disease-specific parameters. Further longitudinal studies to determine the ability of this instrument to measure change in time are warranted, in order to introduce it into epidemiological research and clinical practice.
Abbreviations
- HAQ:
-
Health Assessment Questionnaire
- BDI:
-
Beck Depression Inventory
References
Haythornthwaite JA, Heinberg LJ, McGuire L (2003) Psychological factors in scleroderma. Rheum Dis Clin North Am 29:427–439
Calkins DR, Rubenstein LV, Cleary PD, et al. (1991) Failure of physicians to recognize functional disability in ambulatory patients. Ann Intern Med 114:451–454
Ware JE, Sherbourne CD (1992) The MOS 36-item short-form health survey (SF-36) I. Conceptual framework and item selection. Med Care 30:473–483
Brazier JE, Harper R, Jones MB, et al. (1992) Validating the SF-36 health survey questionnaire: new outcome measure for primary care. BMJ 305:160–164
Mc Horney CA, Ware JE, Lu JFR (1994) The MOS 36-item short-form health survey (SF-36). III. Tests of data quality, scaling assumptions and reliability across diverse patient groups. Med Care 32:40–66
Garratt AM, Ruta DA, Abdalla MI, Buckingham JK, Russel IT (1993) The SF-36 Health Survey questionnaire: an outcome measure suitable for routine use within the NHS? BMJ 306:1440–1444
Talamo J, Frater A, Gallivan S, Young A (1997) Use of the short-form (SF-36) for health status measurement in rheumatoid arthritis. Br J Rheumatol 36:463–469
Husted JA, Gladman DD, Farewell VT, Long JA, Cook RJ (1997) Validating the SF-36 health survey questionnaire in patients with psoriatic arthritis. J Rheumatol 24:511–517
DaCosta D, Dobkin PL, Fitzcharles MA, et al. (2000) Determinants of health status in fibromyalgia: a comparative study with systemic lupus erythematosus. J Rheumatol 27:365–372
Ruta DA, Hursat MP, Kind P, Hunter M, Shibbings A (1998) Measuring health status in British patients with rheumatoid arthritis: reliability, validity and responsiveness of the Short-Form 36-item health survey (SF-36). Br J Rheumatol 37:425–436
Kvien TK, Kaasa S, Smedstad LM (1998) Performance of the Norwegian SF-36 Health Survey in patients with rheumatoid arthritis. II. A comparison of the SF-36 with disease-specific measures. J Clin Epidemiol 51:1077–1086
Hill CL, Parsons J, Taylor A, Leach G (1999) Health related quality of life in a population sample with arthritis. J Rheumatol 26:2029–2035
Strombeck B, Ekdahl C, Manthorpe R, Wilkstrom I, Jacibsson L (2000) Health-related quality of life in primary Sjögren’s syndrome, rheumatoid arthritis and fibromyalgia compared to normal population data using SF-36. Scand J Rheumatol 29:20–28
Husted JA, Gladman DD, Farewell VT, Cook RJ (2001) Health-related quality of life of patients with psoriatic arthritis: a comparison with patients with rheumatoid arthritis. Arthritis Rheum 45:151–158
Wiles NJ, Scott DGI, Barrett EM, et al. (2001) Benchmarking: the five year outcome of rheumatoid arthritis assessed using a pain score, the Health Assessment Questionnaire: and the short-form (SF-36) in a community and a clinic based sample. Ann Rheum Dis 60:956–961
Suarez-Alzamor ME, Ahn C, Friedman AW, et al. (2000) Performance of outcome measures in systemic sclerosis (abstract). Arthritis Rheum 43:S319
Grove ML, Wilson A, Raza K, Carruthers DM, Bacon P (2000) Patients with damage from primary systemic vasculitides experience impaired physical health as measured by the SF-36 (abstract). Arthritis Rheum 43:S368
Cossutta R, Zeni S, Soldi A, Colombelli P, Belotti Masserini A, Fantini F (2002) Evaluation of quality of life in patients with systemic sclerosis by the SF-36 questionnaire (in Italian). Reumatismo 54:122–127
Subcommittee for Scleroderma Criteria of the American Rheumatism Association diagnostic and Therapeutic Criteria Committee (1980) Preliminary criteria for the classification of systemic sclerosis. Arthritis Rheum 23:581–590
Arnett FC, Edworthy SM, Block DA, et al. (1988) The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum 31:315–324
LeRoy EC, Black C, Fleischmayer R, et al. (1988) Scleroderma (systemic sclerosis): classification, subsets and pathogenesis. J Rheumatol 15:202–208
Apolone G, Mosconi P (1998) The Italian SF-36 Health Survey: translation, validation and norming. J Clin Epidemiol 51:1025–1036
Steen VD, Mesdger TA Jr (1997) The value of the Health Assessment Questionnaire and special patient-generated scale to demonstrate change in systemic sclerosis over time. Arthritis Rheum 40:1984–1991
Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J (1961) An inventory for measuring depression. Arch Gen Psychiatry 4:53–63
Mesdger TA Jr, Silman AJ, Steen VD, et al. (1999) A disease severity scale for systemic sclerosis: development and testing. J Rheumatol 26:2159–2167
Valentini G, Della Rossa A, Bombardieri S, et al. (2001) European multicentre study to define activity criteria for systemic sclerosis. II Identification of disease activity variables and development of preliminary activity indexes. Ann Rheum Dis 60:592–598
van der Heijde DM, van’t Hof MA, van Riel PL, Theunisse LA, Lubberts EW, van LeeuwenMA, et al. (1990) Judging disease activity in clinical practice in rheumatoid arthritis: first step in the development of a disease activity score. Ann Rheum Dis 49:916–920
Bettoni L, Geri P, Airò P, et al. (2002) Systemic sclerosis therapy with Iloprost. A prospective observational study of 30 patients treated for a median of 3 years. Clin Rheumatol 21:244–250
Merkel PA, Herlyn K, Martin RW, et al. (2002) Measuring disease activity and functional status in patients with scleroderma and Raynaud’s phenomenon. Arthritis Rheum 46:2410–2420
Clements PJ, Wong WK, Hurwitz EL, et al. (1999) Correlates of the Disability Index of the Health Assessment Questionnaire: a measure of functional impairment in systemic sclerosis. Arthritis Rheum 42:2372–2380
Clements PJ, Wong WK, Hurwitz EL, et al. (2001) The Disability Index of the Health Assessment Questionnaire is a predictor and correlate of outcome in the high-dose versus low-dose penicillamine in systemic sclerosis trial. Arthritis Rheum 44:653–661
Roca RP, Wigley FM, White B (1996) Depressive symptoms associated with scleroderma. Arthritis Rheum 39:1035–1040
Benrud-Larson LM, Haythornthwaite JA, Heinberg LJ, et al. (2002) The impact of pain and symptoms of depression in scleroderma. Pain 95:267–275
Newman S, Mulligan K (2000) The psychology of rheumatic diseases. Baillieres Clin Rheumatol 14:773–786
Moser DK, Clements PJ, Brecht ML, Weiner SR (1993) Predictors of psychosocial adjustment in systemic sclerosis. The influence of formal education level, functional ability, hardness, uncertainty, and social support. Arthritis Rheum 36:1398–1405
Benrud-Larson LM, Heinberg LJ, Haythornthwaite JA, et al. (2002) Body image dissatisfaction in scleroderma: extent and relationship to psychosocial function. Health Psychol 22:130–139
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Danieli, E., Airò, P., Bettoni, L. et al. Health-related quality of life measured by the Short Form 36 (SF-36) in systemic sclerosis: correlations with indexes of disease activity and severity, disability, and depressive symptoms. Clin Rheumatol 24, 48–54 (2005). https://doi.org/10.1007/s10067-004-0970-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-004-0970-z