Abstract
We report on a carrier of human T-lymphotropic virus type 1 (HTLV-1) who developed mixed connective tissue disease (MCTD). This patient suddenly manifested clinical symptoms and interstitial pneumonia ascribable to MCTD following long-term infection with HTLV-1. After initiation of oral prednisolone all manifestations quickly improved in parallel with a decrease in inflammatory reactions. In this patient HTLV-1 infection might have played an important role in the pathogenesis of MCTD. Since HTLV-1 can cause adult T-cell leukemia and HTLV-1-associated myelopathy, and also collagen diseases including MCTD, careful observation is necessary even in a carrier, particularly when autoantibodies are detectable in serum.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Human T-lymphotropic virus type 1 (HTLV-1) is well known as a retrovirus that causes adult T-cell leukemia (ATL) and HTLV-1-associated myelopathy (HAM) [1, 2]. According to several recent reports, however, infection with this virus is often accompanied also by other inflammatory disorders, including arthropathy, bronchopneumonopathy, Sjögren’s syndrome, and systemic lupus erythematosus (SLE) [3, 4, 5, 6]. These disorders can coexist and develop irrespective of associated leukemia [7]. Here, we report on an HTLV-1 carrier who showed mixed connective tissue disease (MCTD) with interstitial pneumonia. In this patient the HTLV-1 infection might have been related to the pathogenesis of MCTD, and we review the literature and focus on the immunomodulatory mechanisms of this virus.
Case report
A 34-year-old Japanese woman was diagnosed as an HTLV-1 carrier during pregnancy. On the basis of familial history the HTLV-1 infection was considered to have occurred by transplacental transmission. She was in good general condition during the pregnancy, but Raynaud’s phenomenon developed in the bilateral fingers soon after delivery. Five months later she sometimes experienced polyarthritis and erythema on her face and both upper extremities, particularly on exposure to sunlight. These symptoms gradually worsened, and she was referred to our hospital. Physical examination showed erythema with itching on both forearms and the anterior side of the bilateral knees, multiple lymphadenopathy in the neck, and sclerotic change to the skin of both hands. The skin biopsy from the hand demonstrated an increase in collagen fibers with mild infiltration of lymphocytes in the dermis (Fig. 1), but no specific findings for ATL. After initiation of vasodilators such as calcium antagonists and prostaglandin, Raynaud’s phenomenon improved but sometimes reappeared, particularly in winter.
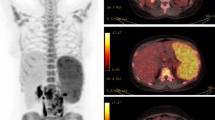
At age 37 she was admitted to a neighboring hospital because of continuous high fever (above 39°C) with reappearance of Raynaud’s phenomenon. The high fever persisted despite the administration of antibiotics, and 5 days later she was again referred to our hospital. Physical examination at admission showed no remarkable findings other than fine crackles over the lower chest bilaterally and sclerotic change in both hands. She complained of systemic arthralgia, but no swelling was seen in any joints. Routine laboratory data demonstrated an increase in inflammatory reactions, including erythrocyte sedimentation rate (ESR, 59 mm/h, normal value: <15 mm/h) and C-reactive protein (CRP, 8.88 mg/dl, normal value: <0.1 mg/dl), and elevated liver enzymes, including alkaline phosphatase (746 U/l, normal: 124~367 U/l), lactate dehydrogenase (529 U/l, normal: 114~220 U/l), aspartate aminotransferase (198 U/l, normal: 12~37 U/l), and alanine aminotransferase (189 U/l, normal: 7~45 U/l). Serum creatine kinase and arterial blood gas under room air were within normal limits, and immature lymphocytes could not be detected in smear specimens of peripheral blood. Antinuclear and anti-U1-ribonucleoprotein (RNP) antibody titers were ×1280 and ×64, respectively, and other autoantibodies, including anti-double-stranded DNA antibody, other anti-extractable nuclear antigen antibodies, antimitochondrial antibody, myeloperoxidase-specific antineutrophil cytoplasmic antibody (ANCA), and proteinase 3-specific ANCA were all negative. The cytomegalovirus antigen could not be detected in peripheral blood, and β-D-glucan was negative in the serum. In Western blot analysis HTLV-1 core protein bands were detected in the serum of the patient (Fig. 2). Chest computed tomography (CT) demonstrated reticular shadows in the lower dorsal portion of both lungs (Fig. 3A).
Soon after cessation of antibiotics liver enzymes in serum returned to normal values. Oral prednisolone was started at a dose of 60 mg/day, and the high fever and Raynaud’s phenomenon immediately improved in parallel with a decrease in inflammatory reactions in serum. One week after starting oral prednisolone the abnormal shadows also disappeared on the chest CT (Fig. 3B). Oral prednisolone was gradually tapered, and she was discharged around 2 months after admission to our hospital. In the follow-up at the outpatient clinic she has since been in good general condition with oral prednisolone at a dose of 5–10 mg/day, although Raynaud’s phenomenon sometimes reappears, particularly in cold weather.
Discussion
At admission to our hospital this patient showed sclerotic change in both hands and positive anti-U1-RNP antibodies with a history of Raynaud’s phenomenon, polyarthritis, lymphadenopathy, and facial erythema, leading to the diagnosis of MCTD following the criteria proposed by the Ministry of Health and Welfare of Japan [8]. Elevated liver enzymes at admission were probably ascribable to the antibiotics administered at the previous hospital. She was considered to have developed MCTD without any other associated disorders specific to long-term persistent infection with HTLV-1, including ATL and HAM. Although the cause-and-effect relationship between HTLV-1 infection and rheumatic diseases remains unconfirmed in retrospective studies [9, 10], there are four reported cases of MCTD developing in HTLV-1 carriers in the literature, and the clinical findings in these cases are summarized in Table 1 [10, 11, 12]. All cases were women and were well controlled with nonsteroidal anti-inflammatory drugs and/or corticosteroid as in this patient, except for one case. Autoimmune disorders other than MCTD also coexisted in three cases, but no patient showed interstitial pneumonia.
There are three possible causes of the associated interstitial pneumonia, which was a notable clinical point in this patient: HTLV-1, other infectious agents, and MCTD itself. Among these, the absence of antibodies and antigens in serum excluded the possibility of other infectious agents such as cytomegalovirus and fungi. Interstitial pneumonia ascribed to HTLV-1 infection, which is designated as HTLV-1-associated bronchopneumonopathy, is characterized clinically by a chronic and slowly progressive course and pathologically by massive infiltration of mature lymphocytes in alveolar septa [4, 13]. This pathology is compatible with lymphocytic interstitial pneumonia (LIP), and radiological examinations frequently demonstrate characteristic findings, including ground-glass attenuation with focal consolidation and sometimes small nodules and cystic formation, in accordance with the progression of the disease [4, 14]. In this patient, however, interstitial pneumonia showed a relatively acute clinical course and reticular shadows alone without radiological findings specific to LIP on chest CT. Although histological examinations could not be performed because of poor general status, these clinical findings suggest that the HTLV-1 infection might have played a role in the formation of interstitial pneumonia, but was not a main and direct cause of it. The most likely cause of the interstitial pneumonia in this patient is MCTD itself. Interstitial pneumonia is frequently associated with MCTD irrespective of apparent pulmonary symptoms and often shows an acute clinical course with a good response to corticosteroid therapy as in this patient [15, 16]. In this disease radiological examinations usually demonstrate irregular and linear hyperattenuating lesions with a reticular pattern mainly in the basal part of both lungs in the early phase of illness, and these findings were seen also in this patient [16, 17]. Considering that the abnormal shadows on CT disappeared soon after initiation of oral prednisolone in parallel with improvement of clinical symptoms due to MCTD, the interstitial pneumonia in this patient belonged to the pathologically early phase of illness and was probably pathogenetically related to the MCTD.
The precise pathogenetic mechanism of MCTD associated with HTLV-1 infection remains unclear. According to a report by Query and Keene [18], U1-RNP cloned from human brainstem partly showed an amino acid sequence homologous to a p30 gag protein found in several retroviruses. Because immunization with p30 gag protein could induce anti-U1-RNP antibodies in experimental animals, this homology in amino acid sequence was considered to probably have cross-reactivity and pathognomonic activity. Also in this patient, associated MCTD might be explainable by molecular mimicry between U1-RNP and HTLV-1. To further clarify the pathogenetic mechanism of MCTD in HTLV-1 carriers, investigation at the molecular level and a larger set of patient data are necessary.
References
Shimoyama M (1991) Diagnostic criteria and classification of clinical subtypes of adult T-cell leukaemia-lymphoma. A report from the Lymphoma Study Group (1984–87). Br J Haematol 79:428–437
Izumo S, Umehara F, Osame M (2000) HTLV-1-associated myelopathy. Neuropathology 20:S65–S68
Hasunuma T (1997) Pathomechanism of HTLV-I associated arthropathy and the role of tax gene (in Japanese). Nippon Rinsho 55:1482–1485
Tateishi U, Nishihara H, Miyasaka K (2001) HTLV-1-associated bronchopneumonopathy (HAB): CT-pathological correlation. Clin Radiol 56:664–666
Nakamura H, Eguchi K, Nakamura T, et al. (1997) High prevalence of Sjögren’s syndrome in patients with HTLV-I associated myelopathy. Ann Rheum Dis 56:167–172
Miura T, Tanaka H, Makino Y, et al. (1999) Human T cell leukemia virus type I-associated myelopathy in a patient with systemic lupus erythematosus. Intern Med 38:512–515
Sugimoto M, Nakashima H, Watanabe S, et al. (1987) T-lymphocyte alveolitis in HTLV-1-associated myelopathy. Lancet 2:1220
Kasukawa R, Tojo T, Miyawaki S, et al. (1987) Preliminary diagnostic criteria for classification of mixed connective tissue disease. In: Kasukawa R, Sharp GC (eds) Mixed connective tissue disease and antinuclear antibodies. Excerpta Medica, Amsterdam, pp 41–47
Sebastian D, Nayiager S, York DY, Mody GM (2003) Lack of association of human T-cell lymphotropic virus type 1 (HTLV-1) infection and rheumatoid arthritis in an endemic area. Clin Rheumatol 22:30–32
Bowness P, Davies KA, Tosswill J, et al. (1991) Autoimmune disease and HTLV-1 infection. Br J Rheumatol 30:141–143
Mizuki M, Tagawa S, Shibano M, et al. (1993) A HTLV-I carrier who showed various symptoms and antibodies of autoimmune diseases. Intern Med 32:449–454
Matsumoto Y, Muramatsu MO, Sato K (1993) Mixed connective tissue disease and Sjögren’s syndrome, accompanied by HTLV-I infection. Intern Med 32:261–264
Ishikawa N, Awaya Y, Maeda H, et al. (2002) KL-6 as an indicator for lymphocytic interstitial pneumonia (LIP) in a human T-lymphotrophic virus type 1 (HTLV-1) carrier. Ann Hematol 81:474–477
Ichikawa Y, Kinoshita M, Koga T, Oizumi K, Fujimoto K, Hayabuchi N (1994) Lung cyst formation in lymphocytic interstitial pneumonia: CT features. J Comput Assist Tomogr 18:745–748
Sullivan WD, Hurst DJ, Harmon CE, et al. (1984) A prospective evaluation emphasizing pulmonary involvement in patients with mixed connective tissue disease. Medicine (Baltimore) 63:92–107
Saito Y, Terada M, Takada T, et al. (2002) Pulmonary involvement in mixed connective tissue disease: comparison with other collagen vascular diseases using high resolution CT. J Comput Assist Tomogr 26:349–357
Kim EA, Lee KS, Johkoh T, et al. (2002) Interstitial lung diseases associated with collagen vascular diseases: radiologic and histopathologic findings. Radiographics 22:S151–S165
Query CC, Keene JD (1987) A human autoimmune protein associated with U1 RNA contains a region of homology that is cross-reactive with retroviral p30gag antigen. Cell 51:211–220
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shimojima, Y., Ishii, W., Hineno, A. et al. Mixed connective tissue disease with interstitial pneumonia in HTLV-1 carrier: case report and review of the literature. Clin Rheumatol 23, 548–551 (2004). https://doi.org/10.1007/s10067-004-0955-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-004-0955-y