Abstract
Subacromial corticosteroid injection is one of the most frequently used management tools in subacromial impingement syndrome (SIS) despite controversial reports on the efficacy. Our purpose, in this single blinded, randomised and controlled study was to clarify whether the corticosteroid injection provides additional benefit when used with other conservative treatment modalities in 48 patients with stage 2 SIS. The patients were randomly divided into three groups according to the two therapeutic injections applied with a 10-day interval: group 1: 10 cc of 1% lignocaine + 40 mg of methylprednisolone for the first and second injections, group 2: 10 cc of 1% lignocaine + 40 mg of methylprednisolone for the first injection and only 10 cc of 1% lignocaine for the second injection, group 3: only 10 cc of 1% lignocaine for the first and second injections. All the patients were prescribed 500 mg of naproxen sodium to use two times daily, instructed to rest and perform Codman’s pendulum exercises during the first 15 days. Shoulder pain during rest, activity, and causing disturbance of sleep was evaluated using a visual analogue scale and shoulder function was investigated by total Constant score and its subsectional parameters which are pain, daily living activities, active range of motion and strength before the therapy and 1 and 3 months after the therapy onset. Significant improvements from the baseline values in all pain and function parameters were observed at the first and second evaluation in all groups. Group 1 patients had more favourably improved values in pain causing sleep disturbance and daily living activity parameters than group 2 and 3 patients only in the 1st month after therapy onset. We found that subacromial corticosteroid injections in the acute or subacute phase of SIS provided additional short-term benefit without any complication when used together with nonsteroidal anti-inflammatory drugs (NSAIDs) and exercise.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tendon disorders are a source of major concern especially for the shoulder joint which is the site of multiple injuries and inflammatory conditions [1, 2]. Subacromial impingement of rotator cuff tendons, the long head of the biceps tendon and subacromial bursa between the humeral head and structures that make up the coracoacromial arch is among the most frequent problems leading to shoulder pain and consequent functional limitation [3, 4]. As the exact pathophysiology and healing mechanism of the tendon pathologies are only partly known, many treatment modalities based on empirical evidence including nonsteroidal anti-inflammatory drugs (NSAID), physical therapy, activity modification and corticosteroid injections have been advocated to be of benefit in subacromial impingement syndrome (SIS) [1, 2, 5]. However, there is little evidence to support the efficacy of therapeutic applications for shoulder pain [6]. Corticosteroid injection is one of the most frequently used management tools in SIS although its effect may not be so well maintained [1, 5]. In a recent meta-analysis, subacromial corticosteroid injection was reported to have a small benefit over placebo [1]. Many authors suggested good short-term results in patients who did not respond to conservative management [5]; however, some reported no efficacy over placebo on the other hand [7]. There seemed to exist a consensus among some authors that there has been a lack of good trials defining the scientific basis of subacromial corticosteroid injections, indications and the efficacy quantification despite the popularity of the intervention [1, 5].
Our purpose, in this single blinded, randomised and controlled study was to clarify whether the corticosteroid injection provides additional benefit when used with other conservative treatment modalities in a group of patients with stage 2 SIS.
Patients and methods
The procedures followed in this study were approved by a local ethics committee. The patients were informed about the study procedure and signed the informed consent prepared for this study.
Patient selection
Forty-eight patients with unilateral shoulder pain and diagnosed as having stage 2 SIS were included in this trial. Details were recorded about the patients’ ages, sexes, occupations, characteristics of pain and additional problems. Diagnosis was based on history, clinical examination, conventional radiography, subacromial injection test and magnetic resonance imaging (MRI). The patients with positive impingement tests (Neer, Hawkins Kennedy and painful arc tests) and positive subacromial injection test were diagnosed as having SIS if they had no calcified lesions in the plain radiograms [8]. The first therapeutic injection containing a local anaesthetic agent was the subacromial injection test at the same time and the patients with negative reactions to the injections were excluded from the study as we accepted this test as a reference test for SIS diagnosis and test-negative patients were thought to have another shoulder pathology, but not SIS, according to Neer’s concept [3]. The pathologic changes in rotator cuff tendons were classified according to Zlatkin MRI stages of SIS [9] by an experienced radiologist on MRI of the shoulder as follows: stage 0: tendon morphology and signal intensity normal, stage 1: increased signal intensity in the tendon without any thinning irregularity or discontinuity, stage 2: increased signal intensity with irregularity and thinning in the tendon, and stage 3: complete disruption of the supraspinatus tendon. Only the patients with stage 2 impingement were included in the study. The patients who had: (1) other concomitant shoulder pathologies such as adhesive capsulitis, calcific tendinitis, dislocations, etc., (2) cervical pain or other painful conditions such as fibromyalgia conflicting the clinical picture, (3) any local or systemic contraindication for corticosteroid use such as infection, diabetes, hypertension, etc., (4) history of gastritis or peptic ulcer that may cause complications with NSAID use, (5) prior applications of any treatment modality such as physiotherapy, corticosteroid injections and NSAID during the preceding 3 months were excluded from the study.
Study groups
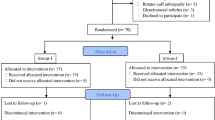
Patients were randomly divided into three equal groups of 16 patients in a simple systematic manner (×+1) according to the therapeutic injections applied. All patients had two subacromial injections with a 10-day interval. The injections were performed into the subacromial space under the acromion using an anterior approach by an experienced physician. The introduction of the needle was assisted by gentle longitudinal traction on the arm to widen the gap between the acromion and the humeral head. The needle was placed below the anterior edge of the acromion. Special attention was paid not to inject the material into the tendon or the glenohumeral joint. The injected medication in the three groups was differentiated as follows: group 1: 10 cc of 1% lignocaine + 40 mg of methylprednisolone for the first and second injections, group 2: 10 cc of 1% lignocaine + 40 mg of methylprednisolone for the first injection and only 10 cc of 1% lignocaine for the second injection, group 3: only 10 cc 1% lignocaine for the first and second injections. The patients knew the injected material consisted of a local anaesthetic agent, but only the physician knew if it consisted of corticosteroid additionally. Moreover, all the patients were prescribed 500 mg of naproxen sodium to use two times a day during the first 15 days. They were instructed to avoid exaggerated movements of the shoulder joint with a relative rest and to perform Codman’s pendulum exercises in this time period. Permission to start strengthening and stretching exercises was given after 1 month. A home exercise programme consisting of isometric and isotonic strengthening while the arm is in a neutral position and posterior capsule stretching was prescribed.
Outcome evaluation
The evaluation of the patients was performed three times by another physician blinded to the content of the subacromial injection: before the treatment, 1 month and 3 months after therapy onset. Shoulder pain during rest and activity periods, also pain causing sleep disturbance, was evaluated using a visual analogue scale (VAS). The patients were instructed to choose the grade of their pain intensity on a 10-point scale on which ‘0’ means no pain, ‘5’ moderate pain and ‘10’ intolerable pain. Functional status of the shoulder joint was evaluated by total Constant scale [10] and its subsectional parameters. This scale evaluates overall shoulder function in 100 points. Shoulder pain, as a subsection of this analysis, was evaluated in 15 points, daily living activities in 20 points, active range of motion in 40 points and strength in 25 points.
Analysis
The changes in pain and function parameters within and between the groups in the 1st and 3rd months after therapy onset were evaluated by nonparametric analysis of variance (ANOVA), Mann-Whitney U and Wilcoxon’s tests using SPSS Statistical program for Windows.
Results
No significant difference was found between the groups in terms of age, gender and symptom duration before the therapy. The mean ages ± SD in the three groups were 48.5±8.5, 50.5±7.6 and 47.5±9.5, respectively, beginning from the first group (p>0.05). Group 1 consisted of 12 female and 4 male patients, while there were 11 female and 5 male patients in group 2 and 10 female and 6 male patients in group 3 (p>0.05). The mean symptom duration was 19.0±12.2 months in group 1, 13.3±9.6 in group 2 and 11.8±7.8 in group 3 (p>0.05).
All the patients completed the study. Three patients from group 1, and two patients from each of groups 2 and 3, could not continue naproxen sodium after 10 days because of dyspeptic symptoms.
Baseline values of pain measured by VAS, total and subsectional functional parameters of the Constant scale were all comparable among the groups (p>0.05). When compared with the baseline values, significant improvements in terms of all pain parameters measured by VAS were observed at the first (1 month later) and second (3 months later) evaluation after therapy onset in all of the groups (p<0.05) (Table 1). The same significant improvements from the baseline values were observed in the total Constant score and all its subsectional parameters at the evaluations of the 1st and the 3rd months after therapy onset (p<0.05) (Table 2).
The group comparisons revealed more favourably improved values in pain causing sleep disturbance measured by VAS (p<0.001) and daily living activity (p<0.001) parameters in group 1 patients than the patients in groups 2 and 3 only in the 1st month after therapy onset (Table 1, Table 2). No significant difference of any parameter was observed among the groups at the second evaluation 3 months after therapy onset (p>0.05).
Discussion
Subacromial impingement syndrome and associated rotator cuff tendinitis are common shoulder problems with the symptoms of pain and loss of motion [4]. The classically accepted underlying pathologies causing these symptoms are oedema, haemorrhage, fibrosis, tendinitis and partial or complete ruptures of the rotator cuff tendons at different stages of the syndrome [3]. Many operative or nonoperative treatment modalities aim to treat these conditions by decreasing the inflammation and stimulating the healing in the tendons. However, the exact healing mechanisms remain partly unknown and this fact leads to use of many empirical conservative treatment methods such as ergonomics at work, NSAID, rest, superficial heat, ice, movement exercises, acupuncture, ultrasound therapy, strengthening exercise, stretching and transcutaneous electrical nerve stimulation [11]. One of these methods is subacromial corticosteroid injection and the current trend is to consider this method when other therapeutic conservative interventions fail to treat the condition [2, 11]. In this study we used NSAIDs, relative rest and Codman’s pendulum exercises in the acute and subacute periods followed by strengthening exercises 1 month later. Additionally we injected corticosteroid into the subacromial space in two groups of patients at admission. So we assessed whether corticosteroids have additional benefit when used once or repeatedly together with NSAID and conventional modalities. Stage 1 patients were not included as the pathologic process is reversible and could conflict the results. We limited the study population to the patients with stage 2 impingement in order to standardise the underlying pathology of tendinitis, tendon fibrosis and thinning where it sounds logical to use corticosteroids. However, subacromial injection of corticosteroids may have harmful effects on the tendon structure such as collagen necrosis, weakness and possible rupture. Akpınar et al. found abnormally soft and light coloured tendons with fragmentation and inflammatory cell infiltration after four times of repeated corticosteroid injections. Saline injections did not cause any kind of pathology in this study [12]. In another rat study, Tillander et al. reported focal inflammation, necrosis and fragmentation of collagen bundles after five corticosteroid injections to the subacromial space of rats, while no pathologic change was observed after three injections [13]. For these reasons we avoided more than two injections and excluded stage 3 patients with complete RC tears in order not to inflict any harm on the torn ligament although no reliable proof exists about this kind of deleterious effect on torn tendons [5].
In a meta-analysis by Buchbinder, subacromial injection with corticosteroids was demonstrated to have a small benefit over placebo in some trials [1]. In another systematic review about the interventions for subacromial pain, the trust of the general practitioners in subacromial corticosteroid injection was supported by definitive evidence for short-term efficacy [11]. It seems that corticosteroids do not alter the natural progression of the disease, but only cause a short-term symptomatic relief especially in pain, perhaps due to an anti-inflammatory effect. It can alter the release of noxious chemicals which are triggered by degenerated tendon and treat pain [5]. We also found short-term better improvement only in pain causing sleep disturbance and daily living activities when the corticosteroid injection was used together with rest, NSAID and exercise treatments. Some studies have found no efficacy difference between NSAID and local corticosteroid injections for shoulder pain in the short term. Our findings suggested that conservative treatment with NSAID and exercise is beneficial for SIS patients and concomitant use of corticosteroid injections provide additional benefit for some of the symptoms when used two times with a 10-day interval. It seems that better improvement especially in pain causing disturbance of sleep may be related with a more efficient anti-inflammatory effect of additional corticosteroid.
Some authors claim that corticosteroids can inhibit the production of collagen and the surrounding granulation tissue, thus prevent fibrosis, in addition to suppress inflammation [5]. Blair et al. observed an increase in shoulder range of motion with subacromial corticosteroid injection, which we could not observe in our study [14]. Green reported that subacromial corticosteroid injection was better than placebo in improving range of motion [6]. The improvement in the joint range of motion observed in these studies may be due to pain relief and effect of fibrosis prevention effect, which consequently facilitates daily living activities. The short-term better ROM improvement shows that this effect must more likely be due to pain relief. However, we could not find any favourable improvement in ROM values neither in the short- nor in the middle-term follow-up. We did not measure the range of motion exactly, but scored according to the Constant scale and that might have caused us to miss smaller improvements.
On the other hand, one study reported having found no beneficial effect of local methylprednisolone over lignocaine injection on symptoms of SIS during 12 weeks of follow-up [7]. This report is in contrast to the general tendency to accept the short-term success of corticosteroid injections. However, it is not surprising, because the various qualities of studies, different patient characteristics and injection techniques may effect the final outcome. Subacromial injection procedure is a relatively difficult procedure. A high incidence of injections was shown to miss the subacromial space. This can lead to a treatment failure with symptom persistence. In a study Esenyel et al. found that accuracy of corticosteroid injections which are evaluated by radiograms after contrast material injections correlated with subsequent shoulder pain and function in SIS [15]. Subacromial corticosteroid injections were performed by an experienced physician in this study. All the injected material consisted of 1% of lignocaine and that provided a check for the accuracy of the injection to the subacromial space. If symptoms relieved in a short time, we considered the place of the injection to be correct.
Recently Khan et al. reported that painful overuse tendon conditions have a non-inflammatorypathology, including rotator cuff diseases. They stated that light microscopy of patients operated on for tendonpain revealed collagen separation, thin, frayed and fragiletendon fibrils, separated from each other lengthwise and disruptedin cross section. There was an apparent increase in tenocytes with myofibroblastic differentiation and classicinflammatory cells were usually absent [16, 17]. They called this non-inflammatory situation tendinosis and they claimed that this term should replace the tendinitis myth. Although this claim gained popularity recently as a possible aetiology, no consensus exists yet on its clinical importance and its reflection to MRI findings in SIS. We also think tendinosis itself can cause asynchronous movement in the shoulder complex leading to impingement of the soft tissues between the humerus and acromion and can precipitate inflammation. The pain causing sleep disturbance and long symptom duration period can be a significant marker of this inflammation in our patients. Thus, our approach to the SIS diagnosis was based on the consequences of impinged tendons as shown by Zlatkin’s MRI classification and we constructed this study on Neer’s concept of SIS. However, on the other hand, the failure of anti-inflammatory medication (either oral or injectional) in the middle- and long-term follow-up seemed to support their way of thinking.
Good trials defining the indications and timing of corticosteroid injections, taking the new developments in the aetiopathogenesis into account, are still lacking. Also some other important issues such as accuracy of needle placement, injection frequency, amount and type of corticosteroids need to be clarified. Our initial aim was not to find answers to all these questions in this study. We found that subacromial corticosteroid injections in the acute or subacute phase of SIS provided additional beneficial effect when used together with NSAIDs and exercise in the short term without any complication. One of the limitations of this study was that it could not be a double blinded study as the physician performing the injections could not be blind to the injected material. The other limitation was the small numbers of patients in the groups to draw very strong conclusions. Also it would have been better if we could have assessed the final status of the patients with a global health quality measure such as SF-36. Further studies with large study populations and quality of life assessments are needed to clarify the unanswered questions.
References
Buchbinder R, Green S, Youd JM (2003) Corticosteroid injections for shoulder pain. Cochrane Database Syst Rev 1:CD004016
Tallia AF, Cardone DA (2003) Diagnostic and therapeutic injection of the shoulder region. Am Fam Physician 67:1271–1278
Neer CS (1983) Impingement lesions. Clin Orthop 173:70–77
Fongemie AE, Buss DD, Rolnick SJ (1998) Management of shoulder impingement syndrome and rotator cuff tears. Am Fam Physician 57:667–674, 680–682
Paavola M, Kannus P, Janvinen TA, Jarvinen TL, Jozsa L, Jarvinen M (2002) Treatment of tendon disorders. Is there a role for corticosteroid injection? Foot Ankle Clin 7:501–513
Green S, Buchbinder R, Glazier R, Forbes A (1998) Systematic review of randomised controlled trials of interventions for painful shoulder. BMJ 316:354–360
Vecchio PC, Hazleman BL, King RH (1993) A double-blind trial comparing subacromial methylprednisolone and lignocaine in acute rotator cuff tendinitis. Br J Rheumatol 32:743–745
Çalış M, Akgun K, Birtane M, Karacan İ, Çalış H, Tüzün F (2000) Diagnostic values of clinical diagnostic tests in subacromial impingement syndrome. Ann Rheum Dis 59:44–47
Zlatkin MB, Ianotti JP, Roberts MC, Esterhai JL, Dalinka ML, Kressel HY, Schwartz JS, Lenkinsky LE (1989) Rotator cuff tears: diagnostic performance of MRG imaging. Radiology 172:223–229
Constant CR, Murley AHG (1987) A clinical method of functional assessment of the shoulder. Clin Orthop 21:160–166
Johansson K, Oberg B, Adolfsson L, Foldevi M (2002) A combination of systematic review and clinicians’ beliefs in interventions for subacromial pain. Br J Gen Pract 52:145–152
Akpinar S, Hersekli MA, Demirors H, Tandogan RN, Kayaselcuk F (2002) Effects of methylprednisolone and betamethasone injections on the rotator cuff: an experimental study in rats. Adv Ther 19:194–201
Tillander B, Franzen LE, Karlsson MH, Norlin R (1999) Effect of steroid injections on the rotator cuff: an experimental study in rats. J Shoulder Elbow Surg 8:271–274
Blair B, Rokito AS, Cuomo F, Jarolem K, Zuckerman JD (1996) Efficacy of injections of corticosteroids for subacromial impingement syndrome. J Bone Joint Surg Am 78:1685–1689
Esenyel CZ, Esenyel M, Yeşiltepe R, Ayanoğlu S, Bulbul M, Sirvanci M, Kara AN (2003) The correlation between the accuracy of steroid injections and subsequent shoulder pain and function in subacromial impingement syndrome Acta Orthop Traumatol Turc 37:41–45
Khan KM, Cook JL, Bonar F, Harcourt P, Astrom M (1999) Histopathology of common tendinopathies. Update and implications for clinical management. Sports Med 27:393–408
Khan KM, Cook JL, Kannus P, Maffulli N, Bonar SF (2002) Time to abandon the “tendinitis” myth. BMJ 324:626–627
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Akgün, K., Birtane, M. & Akarırmak, Ü. Is local subacromial corticosteroid injection beneficial in subacromial impingement syndrome?. Clin Rheumatol 23, 496–500 (2004). https://doi.org/10.1007/s10067-004-0930-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-004-0930-7