Abstract
Our objective was to delineate the relevance of the personality construct alexithymia and anger-in in patients with fibromyalgia syndrome. Fifty subjects with fibromyalgia syndrome were compared to 20 subjects with rheumatoid arthritis and 42 healthy controls on the measures of anxiety, depression, anger, alexithymia, pain intensity and disability. There was a significant difference on the measures of anxiety and anger between FMS and RA groups, and also between FMS patients and healthy controls. There was a significant difference between FMS patients and healthy controls on the measures of depression, difficulty in identifying feelings subscale of TAS (TAS-dif), and total alexithymia scores. When the severity of pain was controlled for, there was a significant difference on the measures of anger and alexithymia between the FMS and the RA groups. Fibromyalgia patients were more alexithymic than rheumatoid arthritis patients even when the level of depression was controlled for. Anger towards oneself, which is anger-in, was higher in patients with fibromyalgia patients than in the rheumatoid arthritis sample. A stepwise regression model showed that the anger-out scores and the anxiety scores predicted the level of pain severity, and this explained 32% of the variance in the fibromyalgia syndrome group. Although anger-in is consistently higher in fibromyalgia patients, it is the behavioral expression of anger, together with anxiety, that predicts the severity of the pain. The difficulty of identifying feelings, rather than other dimensions of alexithymia, seems to be associated with fibromyalgia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fibromyalgia (FMS) is a syndrome of chronic musculoskeletal pain with typical symptoms of chronic musculoskeletal pain and stiffness, tenderness over specific trigger points, fatigue and sleep disturbances [1]. Elevated rates of lifetime and current psychiatric disorders, and elevations on psychological self-report measures assessing depression, anxiety and hypochondriasis, have been reported in FMS patients as well as studies refuting these results [2]. Alexithymia is a personality construct characterized by difficulty in identifying and communicating feelings, and externally oriented thinking [3]. Alexithymic individuals may tend to misinterpret their emotional arousal as symptoms of physical illness [4]. Unable to identify affects as signals of inner psychic events, alexithymic individuals are thought to focus on, and to amplify, the somatic sensations of emotional arousal, which are then experienced as overwhelming somatic distress and/or misinterpreted as signs of disease [5]. Some authors have claimed that alexithymia is common in fibromyalgia patients [6, 7]. This was not confirmed in the study by Malt et al., where no difference was seen in the alexithymia scores of fibromyalgia patients and healthy controls [8]. One must bear in mind that there are substantial individual differences in pain severity and disability among those with persistent pain. The differences in alexithymia may account for variations in the experience of pain and disability [9]. In most cases, pain in fibromyalgia is rated as more severe than that felt by other chronic pain sufferers [10]. Therefore, it is essential to compare fibromyalgia patients with other chronic pain groups after controlling for the pain severity.
The available research indicates that chronic pain patients experience anger, but that this may be underestimated because of denial [11]. Two styles of anger management have received particular attention: anger-in, i.e. the tendency to suppress anger when it is experienced, and anger-out, the tendency to express anger through verbal or physical means [12]. Chronic pain patients have been reported to score higher than controls on measures of anger suppression or hostility, or both, which in turn have been found to be associated with increased pain and disability [13]. Kerns et al. [14] found that the internalization of angry feelings accounted for a significant proportion of the variance in measures of pain intensity, perceived interference and reported frequency of pain behaviors. Gaskin et al. [15] showed that state anger as assessed by the State-Trait Anger Expression Inventory was an important predictor of the affective pain rating index on the McGill Pain Questionnaire. In a study by Okufiji et al. [16] 70% of the chronic pain patient sample reported to have angry feelings. Anger toward oneself was significantly associated with pain and depression, whereas only overall anger was significantly related to overall disability [16]. Although there are studies on the association of chronic pain with anger, empirical studies investigating the role of anger in fibromyalgia patients are few.
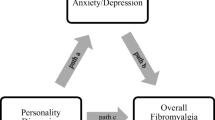
We wanted to see whether the personality constructs alexithymia and anger may be associated with fibromyalgia independent of pain.
Psychological abnormalities found in FMS patients can be related to the degree of pain, and hence the severity of pain should be controlled for to delineate any specific factor. To our knowledge, this is one of the few studies in the literature comparing FMS patients with rheumatoid arthritis (RA) controls on the grounds of anger and alexithymia as measured by TAS-20.
Material and methods
The study was conducted between May 2002 and February 2003 at the outpatient clinics of Karadeniz Technical University Medical School, a university hospital based in the city of Trabzon in northeastern Turkey. All consecutive patients diagnosed as having fibromyalgia according to American College of Rheumatology (ACR) criteria in the outpatient clinics of the physical therapy and rehabilitation department were interviewed [17]. Patients with current suicidal thoughts, psychosis, severe heart disease (congestive heart failure or coronary heart disease) or a debilitating neurological condition were excluded from the study, as well as patients who had used psychotropic agents (antidepressants, anxiolytics and antipsychotics) within the last month. Thirteen subjects were excluded from the study and 50 were found to be eligible. All patients gave informed consent and none refused to participate. All the eligible patients were women. As a medical comparison group consecutive women patients attending the same outpatient clinic with a diagnosis of rheumatoid arthritis as defined by American College of Rheumatology were approached for the study [18]. Of 25 patients approached 20 consented and completed the assessments (an 80% response rate). Subjects who consented to be recruited in the study were representative of women with rheumatoid arthritis attending the outpatient clinic, with no difference in terms of age or duration of illness. As a healthy control group women with no current or past medical history were assessed. This group comprised relatives of outpatients in the physical therapy and rehabilitation outpatient clinics of KTU medical school. The healthy control group did not report current pain. The procedures followed were in accordance with the ethical standards of KTU medical school and with the Helsinki declaration of 1975, as revised in 1983.
All patients were diagnosed as fibromyalgia and RA according to the operational criteria proposed by ACR [17, 18]. The subjects were given the following scales apart from the sociodemographic data form: the Beck Depression Inventory, the Beck Anxiety Inventory, the Toronto Alexithymia Scale, the State-Trait Anger Inventory, and the Fibromyalgia Impact Questionnaire. The severity of the pain was recorded with a visual analog scale (VAS) of 100 mm length by patients. All patients were able to complete the questionnaires independently, alone in a hospital room reserved for them.
Statistics
The Kolmogorov–Smirnov test was used to test the normal distribution of the data. As they were normally distributed, the FMS, RA and control groups were compared with ANOVA (post hoc Bonferroni test). The scores of psychometric assessments between FMS and RA group were compared using Student’s t-test. The VAS pain score was regarded as covariate, and after means had been corrected the difference between the FMS and the RA groups was evaluated using analysis of covariance (ANCOVA). A separate analysis of covariance was made to control for the confounding effects of depression on the alexithymia measure, where depression scores were taken as covariate. Person’s correlation analysis was used to search for univariate relationships between age, pain, disability, anger, alexithymia, anxiety and depression measures in the FMS and RA groups. A stepwise regression model was set up where pain scores were taken as a dependent variable, and age, trait anger, anger-in, anger-out, anger control, depression, anxiety and alexithymia scores were entered into the equation. Next, a stepwise regression model was set up where disability scores were taken as a dependent variable. Quantitative data are presented as mean ± standard deviation and the level of significance was set at 0.05.
Measures
A VAS was used by the patients to rate the intensity of their pain . A 100 mm scale was used, with anchors of ‘no pain’ and of ‘pain as bad as it could be’. Most studies that compare VAS with numerical and verbal ratings conclude that the VAS or the numerical ratings are statistically preferable to the verbal rating scales [19].
The Fibromyalgia Impact Questionnaire
The FIQ is a self-report instrument composed of 19 items [20]. The first 10 items comprise a physical functioning scale; each item is rated on a 4-point Likert-type scale. On items 11 and 12, subjects indicated the number of days that they felt well or missed work because of fibromyalgia symptoms. Items 13–19 are 10 cm visual analog scales along which subjects rated the difficulty in performing their job responsibilities, pain, fatigue, morning tiredness, stiffness, anxiety and depression. All subscores, with the exception of the two work-related scores, were summed to yield the total score of fibromyalgia impact, which ranges from 0 (no impact) to 80 (maximum impact). FIQ is widely used in fibromyalgia patients to evaluate both the clinical severity of the disease and the efficacy of different interventions. It has been found to be valid and reliable in Turkish fibromyalgia patients [21].
The Beck Depression Inventory
The BDI is a 21-item self-report questionnaire that assesses the severity of depression [22]. Individuals are asked to rate themselves on a spectrum of 0–3 (0=least, 3=most) with a score range of 0–63. The total score is a sum of all items. It was shown to be valid and reliable in Turkish patients [23].
The Beck Anxiety Inventory
The BAI is a 21-item self-report questionnaire [24]. Each item is rated on a 4-point Likert scale ranging from 0=not at all to 3=severely, I could barely stand it. The total score ranges from 0 to 63. It was shown to be valid and reliable in Turkish patients [25].
Toronto Alexithymia Scale (TAS)
This is a 20-item self-report scale which has good psychometric properties [26, 27]. Subjects are asked to respond on a 5-point Likert scale the extent to which they agree or disagree with each statement. The results are expressed as TAS-20 global scores, as well as three subscales measuring difficulty in identifying feelings and distinguishing them from bodily sensations of emotion (Factor 1), difficulty expressing feelings (Factor 2), and externally oriented thinking (Factor 3). The Turkish translation of the TAS-20 has good reliability (α=0.76) [28]. Items are rated on a 1–5 scale and summed; higher scores indicate greater levels of alexithymia.
State-Trait Anger Expression Inventory (STAXI)
The STAXI consists of 44 items on which subjects rate themselves on 4-point scales that assess either the intensity of their angry feelings or the frequency with which anger is experienced, expressed, suppressed or controlled. STAXI assesses the intensity of the feelings of anger (state anger) by 7 items, the disposition to experience anger (trait anger) by 6 items, behaviorally expressed anger (anger-out) by 6 items, suppressed anger (anger-in) by 6 items, and self-control of anger behavior (anger control) by 6 items [29]. This scale has been validated in Turkish population studies with Cronbach’s α of subscales ranging between 0.69 and 0.90. The State-anger subscale had not been validated in this study and therefore we did not administer it [30].
Results
Fifty women with FMS, 20 with RA and 42 healthy controls were included in the study. The mean age of the women with FMS was 40.5±8.8, with RA 45.6±14.9 and healthy controls 38.8±10.4, and the difference was not significant (F=2750, df=109, p=0.068). The mean duration of illness was 8.4 (SD=7.8) for FMS patients and 8.9 (SD=7.4) for RA patients. This difference was insignificant. The FIQ mean scores for FMS patients were 48.1 (SD=18.1) and for RA patients 44.0 (SD=12.8). The difference was not significant. (t=0.93, df=68, p=0.355). The mean VAS pain score in the FMS group was 66.8 (SD=23.7) and in the RA group 43.4 (SD=24.3), the difference being significant (t=3.72, df=68, p=0.0005). The FMS group reported significantly higher levels of perceived pain than did the RA group. The sociodemographic data of the subjects are presented in Table 1.
There was a significant difference on the measures of anxiety and anger-in between FMS and RA groups, and also between FMS patients and healthy controls. There was a significant difference between FMS patients and healthy controls on the measures of depression, difficulty in identifying feelings subscale of TAS (TAS-dif), and the total alexithymia scores (Table 2).
Student’s t-test revealed a significant difference in terms of anxiety, anger-in and total alexithymia scores between FMS and RA groups, but when the severity of pain was controlled for there was a significant difference on the measures of anxiety, depression, anger-out, anger-in, trait-anger, TAS-dif and global alexithymia score between FMS and RA groups (Table 3).
When depression was taken as covariate FM patients had significantly higher levels of anger-out, anger-in, trait anger, difficulty identifying feelings and difficulty communicating feelings subscales of TAS-20, as well as the higher global alexithymia score (Table 4).
Univariate correlations revealed that there was a significant association between the trait anger, anger-out, depression, anxiety, alexithymia, disability scores and the perceived pain scores in FMS patients. Disability scores were significantly associated with the levels of perceived pain, depression and anxiety in FMS patients. In the RA group none of the psychological measures were associated with either VAS pain or the FIQ scores. There was only a significant association between pain intensity and disability.
A stepwise regression model was set up to see which factors predicted the level of pain severity in FMS patients. Age, trait anger, anger-in, anger-out, anger control, depression, anxiety and alexithymia scores were entered into the equation, and VAS pain scores were taken as dependent variables. The anger-out scores and the BAI scores predicted the level of pain severity, and this explained 32% of the variance (Table 5, Table 6).
We then set up another stepwise regression model where disability scores were taken as dependent variables. The only independent variable that was able to predict disability scores was the level of the intensity of pain, and this explained 30% of the variance (R2=0.30, β=0.544, t=4.489, p=0.0001).
Discussion
The differences between the educational levels of FMS and RA patients were not statistically significant, but it is remarkable that in the RA group 45% were literate with no formal training, as opposed to 22% in the FMS group. This is in accordance with findings by others that RA patients are often less educated than FMS patients. To our knowledge, there are only two studies addressing the relevance of alexithymia in fibromyalgia patients using TAS. In the study by Brosschot and Aarsse [6] FMS subjects scored higher on the TAS-20 than did healthy controls. An analysis of variance of the alexithymia scores of FMS and healthy subjects with negative affectivity as a covariate showed that the groups still differed significantly. The FMS patients in our study had more difficulty in understanding and identifying emotions than the RA patients or the healthy controls. This contrasts with the findings of Malt et al. [8], where no differences were seen in the alexithymia scores of female FMS patients and age-matched random sample female population controls. In this study a high correlation was found between alexithymia scores and scores for anxiety, depression and neuroticism, which may indicate that alexithymia scores may be associated with psychological distress [8]. In our study, when the severity of pain was controlled for FMS patients still scored significantly higher than the RA controls on the difficulty in identifying subscale of the Toronto Alexithymia Scale. FMS patients also had significantly higher total alexithymia scores than the RA patients. This finding is important in the sense that alexithymia does not emerge as a product of pain, but rather is intrinsic to this illness. Alexithymia has been linked to depression in some studies [31]. For our study, one might argue that depression mediates the relationship between alexithymia and pain. FMS patients did not appear to be more depressed than RA patients in our study; indeed, when the severity of the pain was controlled for, RA patients were even more depressed than FM patients. When depression measure was taken as covariate, FMS patients were significantly more alexithymic than RA controls. In this analysis the difficulty in communicating feelings subscale of TAS also revealed a significant difference between the two pain groups. This shows that alexithymia in FMS patients was not confounded by the levels of depression or pain intensity in our sample. Alexithymia has been reported to be associated with enhanced sensitivity not only to internal (somatic) unpleasant sensations, but also to externally induced pain [32]. Alexithymic individuals may tend to misinterpret their emotional arousal as symptoms of physical illness [4]. Self-reports by fibromyalgia patients of physical symptoms and comorbid conditions, as well as their perceived importance, is in excess of that seen in other rheumatic disease patients, pointing toward somatization as a feature of the illness [33]. FMS patients might rate their symptoms as more severe because of their alexithymic nature. We think that this finding should be further corroborated by future studies employing FMS patients from the community.
FMS patients showed higher scores of anger-in compared to RA and healthy controls in our study. Anger-in refers to the suppression of the angry feelings, whereas anger-out is the engagement in aggressive behavior when motivated by angry feelings [12]. Findings suggest that these anger dimensions are associated with sensitivity to both acute and chronic pain [34]. Individuals less inclined to control anger display lower pain thresholds and tolerance of the ischemic task [13]. Elevated anger has been associated with greater chronic pain intensity among patients with FMS. Positive relationships between chronic pain intensity and trait anger, anger-in, and anger-out have been found [35]. When the severity of pain has been controlled for trait-anger and anger-out were higher in the RA group, whereas anger-in was still higher in the FMS group in our study. It seems that RA patients are more prone to anger (trait anger) and they more readily express it, but anger is rather internalized and suppressed by FMS patients. Our findings differ from Amir et al.’s study [35], where there was no difference in the measure of anger between FMS, RA and chronic low back pain (CLBP) groups.
In the univariate correlation analysis psychological measures were associated with pain and disability scores in the FMS group but not in the RA group. This finding might be attributed to the ‘somatizing’ nature of FMS patients. Payne et al. [36] compared the FMS patients with arthritis groups and proposed that the ‘conversion V profile’ on MMPI might be specific for FMS patients. Another study has revealed the same ‘conversion V pattern’ in FMS and CLBP patients, but not in RA patients [37]. This does not mean that psychological factors are not operating in RA patients, but rather, they are more intrinsic to the illness process in FMS patients than in RA patients. In the regression model, pain severity in FMS patients was determined by the anxiety and anger-out levels. Celiker et al. [38] found pain severity to be correlated with trait anxiety scores in FMS patients. Anxious subjects whose anxiety levels and psychological states fluctuate concomitantly in response to everyday stressors may perceive body sensations as more intense than do non-anxious subjects, who, because of a steadier emotional tone, have less autonomic fluctuation [39]. Wade et al. [40] assessed depression, anxiety, anger, frustration and fear on visual analog scales (VAS) and regressed these on to VAS measures of pain-related unpleasantness and depression as indexed by the Beck Depression Inventory and the MMPI. They found that when pain unpleasantness was at its minimum it was significantly predicted by anger and anxiety, and when the pain unpleasantness was at its maximum it was best predicted by anxiety. In our study, it is interesting to see that anger-out rather than anger-in predicts pain severity in the FMS patients. In a study by Okufiji et al. [16] predictive analyses revealed that CLBP patients reporting higher overall levels of anger experienced higher levels of pain, depression and disability. Chronically angry emotional reactions are often maladaptive because they lead to pervasive interpersonal disruption and chronic sympathetic activation [41]. We suggest that the behavioral expression of anger may lead to enhanced pain sensitivity by causing sympathetic activation.
Finally we should mention several caveats of our study. Correlational analyses do not give a definitive idea about the line of causation. It might be argued that the anger-out scores and the BAI scores are predicted by the pain rather than the reverse. But the idea of the reverse fits very well in with the philosophy of pain as described by Morris [42]. Our assessors were not blind to whether patients had FMS or RA, to circumvent possible assessor biases, but as all our measures are self-report instruments this bias must be regarded as minimal. We recruited clinical samples into our study rather than a representative cross-section of the population with FMS. This might have led to a selection bias where more anxious and depressive persons with FMS were recruited. We tried to control for this by recruiting another chronic pain control group. Subjective pain ratings were used instead of an objective instrument, and this might have led more distressed subjects to rate their pain as more severe. Against all these methodological pitfalls, we believe that our study sheds further light on the psychological determinants of fibromyalgia syndrome. Alexithymia and anger are two constructs that should be addressed in the psychopathology of fibromyalgia. In conclusion, we found that subjects with FMS scored higher on the measure of alexithymia and anger-in than did RA patients and healthy controls. Pain severity was determined by the levels of anxiety and anger-out in our FMS sample. Alexithymia was still significantly higher when pain severity and depression were controlled for separately in the FMS group. Neither alexithymia nor the suppressed anger (anger-in) seems to be confounded by pain severity, but play pathogenetic roles in FMS independently. Though anger-in is consistently higher in FMS patients, it is the behavioral expression of anger, together with anxiety, that predicts the severity of the pain. The difficulty of identifying feelings, rather than other dimensions of alexithymia, seems to be associated with FMS.
Abbreviations
- CLBP:
-
Chronic low back pain
- FMS:
-
Fibromyalgia syndrome
- RA:
-
Rheumatoid arthritis
- VAS:
-
Visual analog scale
References
Wolfe F, Smythe HA, Yunus MB et al. (1990) The American College of Rheumatology 1990 criteria for the classification of fibromyalgia. Report of the Multicenter Criteria Committee. Arthritis Rheum 33:160–172
Epstein SA, Clauw D, Klein D, Kuck J, Masur D, Waid R (1999) Psychiatric disorders in patients with fibromyalgia. Psychosomatics 40:57–63
Taylor G (1984) Alexithymia: Concept, measurement, and implications for treatment. Am J Psychiatry 141:725–732
Lumley MA, Stettner L, Wehmer F (1996) How are alexithymia and physical illness linked? A review and critique of pathways. J Psychosom Res 41:505–518
Taylor GJ, Parker JDA, Bagby MA, Acklin MW (1992) Alexithymia and somatic complaints in psychiatric outpatients. J Psychosom Res 36:417–424
Brosschot JF, Aarsse HR (2001) Restricted emotional processing and somatic attribution in fibromyalgia. Int J Psychiatry Med 31:127–146
Leichner-Hennig R, Vetter GW (1986) [Relation between pain experience and psychological markers in patients with fibrositis syndrome and patients with rheumatoid arthritis]. Z Rheumatol 45:139–145
Malt EA, Olafsson S, Lund A, Ursin H (2002) Factors explaining variance in perceived pain in women with fibromyalgia. BMC Musculoskel Dis 3:12–21
Lumley MA, Smith JA, Longo DJ (2002) The relationship of alexithymia to pain severity and impairment among patients with chronic myofascial pain. Comparisons with self-efficacy, catastrophizing, and depression. J Psychosom Res 53:823–830
Walter B, Vaitl D, Frank R (1998) Affective distress in fibromyalgia syndrome is associated with pain severity. Z Rheumatol 57:101–104
Fernandez E, Turk DC (1995) The scope and significance of anger in the experience of chronic pain. Pain 61:165–175
Spielberger CD, Jacobs G, Russel S, Crane RS (1983) Assessment of anger: the state-trait anger scale. In: JN Butcher,Spielberger CD (eds) Advances in personality assessment, vol 2. Hillsdale, Lawrence Erlbaum, pp 159–186
Janssen SA, Spinhoven P, Brosschot JF (2001) Experimentally induced anger, cardiovascular reactivity, and pain sensitivity. J Psychosom Res 51:479–485
Kerns RD, Rosenberg R, Jacob MC (1994) Anger expression and chronic pain. J Behav Med 17:57–67
Gaskin GE, Greene AF, Robinson ME, Geisser ME (1992) Negative affect and the experience of chronic pain. J Psychosom Res 36:707–713
Okifuji A, Turk DC, Curran SL (1999) Anger in chronic pain: Investigations of anger targets and intensity. J Psychosom Res 47:1–12
Wolfe F, Smythe HA, Yunus MB et al. (1990) The American College of Rheumatology 1990 criteria for the classification of fibromyalgia. Report of the Multicenter Criteria Committee. Arthritis Rheum 33:160–172
Arnett FC, Edworthy SM, Bloch DA et al. (1988) The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum 31:315–24
Huckisson HC (2000) Visual analog scales. Handbook of psychiatric measures. Washington, DC, American Psychiatric Press, pp 601–603
Burckhardt CS, Clark SR, Bennett RM (1991) The Fibromyalgia Impact Questionnaire: development and validation. J Rheumatol 18:728–733
Sarmer S, Ergin S, Yavuzer G (2000) The validity and reliability of the Turkish version of the Fibromyalgia Impact Questionnaire. Rheumatol Int 20:9–12
Beck AT, Waed CH, Mendelson M (1961) An inventory for measuring depression. Arch Gen Psychiatry 4:561–571
Hisli N (1988) Beck Depresyon Olcegi’nin bir Turk ornekleminde gecerlilik ve guvenilirligi [The reliability and validity study of the Beck Depression Inventory in a Turkish sample]. Psikoloji Dergisi 6:118–122 (in Turkish)
Beck AT, Epstein N, Brown G, Steer RA (1988) An inventory for measuring clinical anxiety: Psychometric properties. J Consult Clin Psychol 56:893–897
Ulusoy M, Sahin NH, Erkmen H (1998) Turkish version of the Beck Anxiety Inventory: Psychometric properties. J Cognitive Psychother 12:163–172
Bagby RM, Parker JDA, Taylor GJ (1994) The 20-Item Toronto-Alexithymia-Scale-1. Item Selection and Cross-Validation of the Factor Structure. J Psychosom Res 38:23–32
Bagby RM, Taylor GJ, Parker JDA (1994) The 20-Item Toronto-Alexithymia-Scale-2. Convergent, Discriminant, and Concurrent Validity. J Psychosom Res 38:33–40
Sayar K, Gulec H, Ak I (2001) Yirmi soruluk Toronto Aleksitimi Olcegi’nin guvenirligi ve gecerligi (The reliability and validity of the Twenty-Item Toronto Alexithymia scale). 37. Ulusal Psikiyatri Kongresi Bilimsel Calismalar Ozet Kitabi (37th National Congress of Psychiatry, Scientific Studies Abstract Book). Istanbul
Spielberger CD, Gorsuch RL, Lusahene RE (1970) Manual for Stait-Trait Anxiety Inventory. California, Consulting Psychologists Press
Ozer AK (1994) Surekli Ofke ve Ofke Ifade Tarzi Olcekleri On Calismasi. Turk Psikoloji Dergisi 9:31:26–35
Hintikka J, Honkalampi K, Lehtonen J, Viinamaki H (2001) Are alexithymia and depression distinct or overlapping constructs? A study in a general population. Compr Psychiatry 42:229–234
Nyklicek I, Vingerhoets A (2000) Alexithymia is associated with low tolerance to experimental painful stimuli. Pain 65:471–475
Wolfe F, Hawley DJ (1998) Psychosocial factors and the fibromyalgia syndrome. Z Rheumatol 57:88–91
Bruehl S, Burns JW, Chung OY, Ward P, Johnson B (2002) Anger and pain sensitivity in chronic low back pain patients and pain-free controls: the role of endogenous opioids. Pain 99:223–233
Amir M, Neumann L, Bor O, Shir Y, Rubinow A, Buskila D (2000) Coping styles, anger, social support, and suicide risk of women with fibromyalgia syndrome. J Musculoskel Pain 8:7–20
Payne TC, Leavitt F, Garron DC et al. (1982) Fibrositis and psychologic disturbance. Arthritis Rheum 25:213–217
Ardic F, Toraman F (2002) Psychological dimensions of pain in patients with rheumatoid arthritis, fibromyalgia syndrome, and chronic low back pain. J Musculoskel Pain 10:19–29
Celiker R, Borman P, Oktem F, Gokce-Kutsal Y, Basgoze O (1997) Psychological disturbance in fibromyalgia : relation to pain severity. Clin Rheumatol 16:179–184
Hoehn-Saric R, McLeod DR, Zimmerli WD (1989) Symptoms and treatment of generalized anxiety disorder patients with high versus low levels of cardiovascular complaints. Am J Psychiatry 146:854–859
Wade JB, Price DD, Hamer RM, Scwartz SM, Hart RM (1990) An emotional component analysis of pain. Pain 40:303–310
Greenwood KA, Thurston R, Rumble M, Waters SJ, Keefe FJ (2003) Anger and persistent pain : current status and future directions. Pain 103:1–5
Morris CW (1970) Foundations of the theory of signs. Chicago, Chicago University Press, 1938/1970
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sayar, K., Gulec, H. & Topbas, M. Alexithymia and anger in patients with fibromyalgia. Clin Rheumatol 23, 441–448 (2004). https://doi.org/10.1007/s10067-004-0918-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-004-0918-3