Abstract
Subluxation of the cervical spine is one of a number of devastating complications of rheumatoid arthritis. In spite of this, the features of cervical spine subluxation in Thai patients with rheumatoid arthritis have never previously been studied. We enrolled 134 patients with rheumatoid arthritis who were being followed at the rheumatology clinic, Ramathibodi Hospital, during 1978–2001. Radiological examinations were made in lateral neck flexion, extension and open-mouth views. Symptoms of neck pain and the results of relevant neurological examinations were recorded at the time of imaging. Other data on clinical features and treatments since diagnosis were reviewed retrospectively. The overall prevalence of cervical spine subluxation was 68.7%, which can be categorised into anterior (26.9%), posterior (14.9%), lateral (17.2%), vertical (16.4%) atlantoaxial and subaxial subluxation (28.4%). The percentages of cervical subluxation in patients who had suffered from the disease for 1, 5, 10 or more than 10 years were 77.8%, 64.9%, 70% and 64.7%, respectively. None of the patients had neurological deficits. No correlation between neck pain and cervical spine subluxation was established. The number of patients treated with corticosteroids was significantly higher in the subluxation group than in the non-subluxation group (p=0.04). However, no difference in duration of treatment and cumulative dosages of steroids was displayed between the two groups. It was concluded that the prevalence of cervical spine subluxation in Thai patients with rheumatoid arthritis is much higher than the average, even in the early phase of the disease. Hence, radiological examination of the cervical spine should be included in the initial evaluation of Thai RA patients. Corticosteroid use was associated with cervical subluxation, regardless of dose and duration of treatment. The possible explanations are that steroids may directly cause ligament laxity, osteoporosis and decreasing muscle mass, which leads to accelerated subluxation, or that steroid treatments are used in more severe cases which have a higher tendency towards cervical subluxation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rheumatoid arthritis (RA) is a chronic systemic inflammatory disorder of unknown aetiology that can affect people all over the world. The cervical spine alteration is commonly associated with rheumatoid arthritis, which may result in spinal cord and brainstem compression, causing severe neurological symptoms or death. Cervical spine involvement can be classified into three patterns: 1) involvement of the atlantoaxial complex with anteroposterior subluxation and the odontoid process; 2) involvement of the lateral facet joints of C1/C2 and the atlantooccipital joints with lateral, rotatory and vertical subluxation; and 3) involvement of the subaxial spine, presenting as subluxation with or without discitis [1].
In earlier studies the prevalence of cervical spine changes varied in diverse populations [2, 3, 4, 5, 6]. The most frequent involvement of the cervical spine was the atlantoaxial complex with anteroposterior subluxation and odontoid process [1]. Fifty percent of patients with cervical involvement had neck pain, but the remainders were asymptomatic [7]. Although there may be no neurological signs in patients with large subluxations [8], once signs of cervical cord compression do appear, myelopathy will progress rapidly and 50% of these patients will die within a year [9].
The prevalence of rheumatoid arthritis in the Thai population is 0.12% [10]. However, cervical lesions in Thai patients with RA have never been reported. Therefore, the objective of this study was to investigate the prevalence of cervical subluxations and their clinical correlation in Thai patients with RA.
Methods
From 1978 to 2001, 134 RA patients who were being followed up at the rheumatology clinic, Ramathibodi Hospital, were randomly selected and enrolled in this study. The patients had to fulfill the following inclusion criteria: 1) meet the American College of Rheumatology classification criteria for RA [11]; 2) age >16 years; and 3) duration of symptoms >6 months. The exclusion criteria were pregnancy, previous cervical spine surgery, and patients who refused to join the study. The symptom of neck pain was recorded and a neurological examination was performed in all patients at the time of imaging. The medical reports during the period from diagnosis to radiological examination were reviewed.
The study was performed according to the principles of the Declaration of Helsinki and approved by an ethical clearance committee on human rights related to research involving human subjects. All patients involved in this study gave their written consent to participation. This study was supported by a research grant from the Faculty of Medicine, Ramathibodi Hospital, Mahidol University.
Radiological examinations
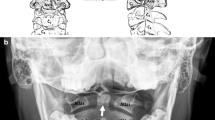
Radiographs of the cervical spine were taken in lateral (during flexion and extension) and open-mouth views using a 150-cm tube-to-plane distance. A diagnosis of anterior atlantoaxial subluxation (AAAS) was made if the distance between the posterior aspect in the middle level of anterior arch of the atlas and the anterior aspect of the dens was >3 mm during flexion. Posterior atlantoaxial subluxation (PAAS) was diagnosed if the posterior aspect of the anterior arch of the atlas was situated posteriorly in relation to the anterior aspect of the dens in the lateral view radiographs taken during extension. Vertical subluxation or atlantoaxial impaction (AAI) was described if the distance that the tip of the odontoid extended above a line (McGregor’s line) drawn between the hard palate and the most caudal inferior point of the occipital curve was >4.5 mm. Lateral atlantoaxial subluxation (LAAS) was considered present if the lateral masses of C1 were displaced >2 mm laterally with respect to C2 and the patient’s head was kept from rotating. Subaxial subluxation (SAS) was considered significant if a vertebra had moved >1 mm in relation to the next vertebra when measured from the posterior line of the vertebral bodies. Disc space narrowing at C2/3, C3/4 and C4/5 was recorded only if there was a relative lack of osteophytes. Disc space narrowing at lower levels in the cervical spine was not documented, as degenerative changes are frequently superimposed. Vertebral plate erosions and sclerosis, including apophyseal joint erosions and sclerosis, were also looked for.
All cervical spine radiographs were evaluated separately by two investigators (P.P. and C.P.). The results were compared and re-evaluated in consensus, if there were incompatible findings.
Statistical analysis
The descriptive values of variables were expressed as the mean ± SD or median. Comparisons between groups were performed by unpaired t-test or the Mann–Whitney test. Measurement of discrete distribution was expressed as counts and percentages, and the association between groups was analysed by χ2 or Fisher’s exact tests.
Results
The demographic data of the patients are shown in Table 1. Most of the RA patients were female (92.5%) which is general the case in the Thai RA population [12]. Erythrocyte sedimentation rate (ESR) at the time of diagnosis and of X-ray was quite high (67.7 ± 35.6 mm/h and 45.1 ± 29.8 mm/h, respectively). Eighty-four of 134 patients (62.7%) were being treated with steroids and 39 (29.1%) had been using steroids acquired from the local pharmacy without prescription prior to diagnosis. As several preparations containing steroid were obtainable, the dosage of steroid from the dispensary cannot be assessed. The prescribed steroid was low-dose (prednisolone 5–10 mg/day). Disease-modifying antirheumatic drugs (DMARD) were used in almost all of the patients (97.1%). Up to 88 of 134 patients (65.7%) received combination DMARD.
Abnormal X-ray findings demonstrated cervical subluxation as follows: AAAS 26.9%, PAAS 14.9%, AAI 16.4%, LAAS 17.2% and SAS 28.4% (Table 2). The overall number of subluxations was 92 out of 134 patients (68.7%). There was no difference in the number of total subluxations between 82 of 124 females (66.1%) and 7 of 10 males (70%). Other findings were erosion of the dens (18.7%), vertebral plate erosion (10.4%), disc space narrowing (33.5%), apophyseal joint narrowing (80.6%), erosion (5.2%) and sclerosis (1.5%).
The prevalence of subluxation was not distinguished between patients with various disease durations. The incidence of subluxation was high even among patients with early disease, i.e. duration less than 1 year (77.8%), which is similar to that in patients with disease duration 5 years or less (64.9%), 10 years (70%), and more than 10 years (64.7%). The association between neck pain and cervical subluxation was shown (Table 3). Forty of 92 patients (43.5%) with cervical subluxation had symptomatic neck pain, whereas 52 patients (56.5%) did not. Forty of 56 patients (71.4%) who complained of neck pain exhibited cervical subluxation. There was no association between cervical subluxation and neck pain (p>0.05). Furthermore, analysis of the subgroup of patients with anterior AAS discovered no relationship between neck pain and amount of subluxation (p=0.07). None of the patients had neurological deficits.
The clinical parameters in patients with and without cervical subluxation were analysed (Table 4). There were no statistically significant differences between the groups in duration of symptoms to diagnosis and duration of disease before X-ray examination. The two groups were also parallel in ESR, rheumatoid factor, number of patients using steroids without prescription prior to diagnosis, initial X-ray changes, and number and type of DMARDtreatments (p>0.05).
Sixty-three of 92 subluxation patients (68.5%) received corticosteroid treatment, in contrast to 21 of 42 non-subluxation patients (50%). These figures reached a statistically significant difference (p=0.04). However, cumulative dosage and duration of steroid treatment were comparable between the groups.
Discussion
Narrowing of the apophyseal joints is the most frequent abnormal radiographic finding from plain X-ray studies and gives a prevalence of cervical involvement at 80.6% in our RA patients. This is approximately the same as previously reported in the 1970s [3] but higher than the prevalence reported in 2000 [7] (80.7% vs 57%). There are two probable explanations for this inconsistency in the same period. First, our hospital is a referral centre taking care of more severe RA patients. Second, although DMARD treatments that are believed to retard atlantoaxial subluxation [13] were given to most of our patients, they are still under treated evidence such as high ESR levels at the time of radiological examination. Also, the start of therapy may have been too delayed to impede the subluxation (median duration of symptoms to diagnosis 12 months).
Atlantoaxial subluxation that can bring about spinal cord compression was recognised in 68.7% of our patients and was more common than the 42%–50% prevalence reported by previous prospective studies [2, 3, 6, 14, 15]. This inconsistency might be explained by diverse criteria for radiological change. However, vertical subluxation (AAI), which carries the worst prognosis of all types of AAS, occurred less often than in previous studies [15] (16.4% vs 26%).
The earliest and most common symptom of cervical subluxation is pain radiating up into the occiput [16]. Only a half of our cervical subluxation patients had neck pain, which is in agreement with other reports [7]. Even if subtle signs of myelopathy are also present, neurological symptoms bear only a slight relationship to the degree of subluxation and may relate to individual variations in the diameter of the spinal canal. None of the patients had this abnormality on neurological examination. Nevertheless, physicians should be aware that patients are susceptible to small falls, whiplash injuries and general anaesthesia with intubation. Subluxations can also cause twisting and compression of the vertebral arteries, leading to vertebrocerebellar insufficiency.
Prognostic factors in determining radiographic damage in early RA included erosion score >1, IgM RF positivity, and ESR >33 mm/h [17]. We found no statistically significant differences in these parameters between patients with and without abnormalities on cervical X-ray examination. There were also no differences in the duration of symptoms to diagnosis and X-ray examination, or in the number of patients using steroids without prescription prior to diagnosis and DMARD treatment. Interestingly, even patients with a disease duration of less than 1 year had an up to 77.8% prevalence of cervical subluxation. Other studies have also reported AAS in patients with a mean disease duration as little as 7 months [18]. In the FIN-RACo trial [13], patients with early active RA, if randomised to triple therapy which also included low-dose (5–10 mg) prednisolone, had no AAAS compared to those treated with monotherapy but allowed to use steroids if they had active disease [13]. In contrast, the only parameter associated with cervical subluxation in our study was the steroid treatment. Other studies are also in agreement with ours [4, 14]. Unfortunately, the amount of steroid that the patients received from the local pharmacy cannot be evaluated. Hence we cannot identify the purely steroid effect on cervical subluxation. The only conclusion is that the cumulative dosage and duration of steroid treatment in the subluxation group were similar to those in the non-subluxation group. The possible explanations of this outcome are that: 1) steroid directly causes ligament laxity, osteoporosis and a decrease in muscle mass; 2) steroid reduces the symptom leading to delay in DMARD adjustment together with overuse of the neck which can accelerate cervical subluxation; and 3) steroids are likely to be used in more severe cases with a higher tendency to cervical subluxation. Other than this, we can reveal no difference in prognostic factors between subluxation and non-subluxation in this study.
In conclusion, we found a higher prevalence of cervical spine subluxation in our RA patients. As there is no correlation between the duration of the disease, signs and symptoms and parameters of active disease, radiological examination of the cervical spine should be included in the initial evaluation of RA patients in order to prevent the danger of spinal cord compression. This study demonstrated the correlation between cervical subluxation and steroid treatment. However, it is an uncontrolled study and the patients treated with steroids may have a more severe disease, which could be at least one reason for the cervical changes. For ethical reasons we cannot carry out a prospective trial to determine the consequences of steroid treatment without DMARD therapy for cervical subluxation. Therefore, rheumatologists should treat rheumatoid arthritis so actively that all the inflammation is suppressed, in order to hinder the serious complication of cervical subluxation. As most RA patients are postmenopausal women,the risk of osteoporosis due to steroid use should also be borne in mind. Also of concern is the correlation between cervical subluxation and steroid treatment. Corticosteroid use in rheumatoid arthritis should be avoided if at all possible.
Abbreviations
- RA:
-
Rheumatoid arthritis
- AAAS:
-
Anterior atlantoaxial subluxation
- PAAAS:
-
Posterior atlantoaxial subluxation
- AAI:
-
Atlantoaxial impaction
- LAAS:
-
Lateral atlantoaxial subluxation
- SAS:
-
Subaxial subluxation
- DMARD:
-
Disease-modifying antirheumatic drugs
References
Halla JT, Hardin JG, Vitek J, Alarcon GS (1989) Involvement of the cervical spine in rheumatoid arthritis. Arthritis Rheum 32: 652–659
Mathews JA (1974) Atlantoaxial subluxation in rheumatoid arthritis. A 5-year follow-up study. Ann Rheum Dis 33:526–531
Isdale IC, Conlon PW (1971) Atlantoaxial subluxation. A 6-year follow-up report. Ann Rheum Dis 30:387–389
Smith PH, Benn RT, Sharp J (1972) Natural history of rheumatoid cervical luxations. Ann Rheum Dis 31:431–439
Halla JT, Hardin JG Jr (1990) The spectrum of atlantoaxial facet joint involvement in rheumatoid arthritis. Arthritis Rheum 33: 325–329
Winfield J, Cooke D, Brook AS, Corbett M (1981) A prospective study of the radiological changes in the cervical spine in early rheumatoid disease. Ann Rheum Dis 40:109–114
Fujiwara K, Owaki H, Fujimoto M, Yonenobu K, Ochi T (2000) A long-term follow-up study of cervical lesions in rheumatoid arthritis. J Spinal Disord 13: 519–526
Pellicci PM, Ranawat CS, Tsairis P, Bryan WJ (1981) A prospective study of the progression of rheumatoid arthritis of the cervical spine. J Bone Joint Surg Am 63: 342–350
Meijers KA, Cats A, Kremer HP, Luyendijk W, Onvlee GJ, Thomeer RT (1984) Cervical myelopathy in rheumatoid arthritis. Clin Exp Rheumatol 2: 239–245
Chaiamnuay P, Darmawan J, Muirden KD, Assawatanabodee P (1998) Epidemiology of rheumatic disease in rural Thailand: a WHO-ILAR COPCORD study. J Rheumatol 25: 1382–1387
Arnett FC, Edworthy SM, Bloch DA et al. (1988) The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum 31:315–324
Osiri M, Akkasilpa S, Deesomchok U (2000) Initial disease modifying antirheumatic drugs and prednisolone prescriptions for patients with rheumatoid arthritis: a 15-year study. J Med Assoc Thai 83:217–224
Neva MH, Kauppi MJ, Kautiainen H et al. (2000) Combination drug therapy retards the development of rheumatoid atlantoaxial subluxations. Arthritis Rheum 43: 2397–2401
Rasker JJ, Cosh JA (1978) Radiological study of cervical spine and hand in the patients with rheumatoid arthritis of 15 years’ duration: an assessment of the effects of corticosteroid treatment. Ann Rheum Dis 37:529–535
Neva MH, Kaarela K, Kauppi M (2000) Prevalence of radiological changes in the cervical spine –a cross sectional study after 20 years from presentation of rheumatoid arthritis. J Rheumatol 27: 90–93
Monsey RD (1997) Rheumatoid arthritis of the cervical spine. J Am Acad Orthop Surgery 5: 240–248
Combe B, Dougados M, Goupille P et al. (2001) Prognostic factors for radiographic damage in early rheumatoid arthritis: a multiparameter prospective study. Arthritis Rheum 44: 1736–1743
Paimela L, Laasonen L, Kankaanpää E, Leirisalo-Repo M (1997) Progression of cervical spine changes in patients with early rheumatoid arthritis. J Rheumatol 24: 1280–1284
Acknowledgements
We thank Umaporn Udomsubpayakul and Trairak Pisitkun for kindly helping with the statistical analysis, and Vassana Sawatdee for providing patients’ files.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pisitkun, P., Pattarowas, C., Siriwongpairat, P. et al. Reappraisal of cervical spine subluxation in Thai patients with rheumatoid arthritis. Clin Rheumatol 23, 14–18 (2004). https://doi.org/10.1007/s10067-003-0782-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-003-0782-6