Abstract
The aim of this study was to investigate the association between the polymorphism of transporters associated with antigen processing (TAP1/TAP2) genes and rheumatoid arthritis in Chinese patients. A total of 100 RA patients and 99 healthy control subjects were enrolled. Analyses with polymerase chain reaction (PCR) based restrictions were used to identify the polymorphisms of the TAP1 and TAP2 genes, which were mapped on chromosome 6. There was a significant difference in the distribution of the TAP2 gene codon 565 polymorphism frequency between the RA patients and healthy control subjects (p<0.001). The odds ratio for the risk of the ‘A’ allele in RA patients was 1.60 (95% CI: 0.82–2.92). No statistical associations in the distribution of the TAP1 gene polymorphism frequency were found between RA patients and controls. There were some physical links found between TAP1/TAP2 gene polymorphism loci. However, there was no linkage observed from TAP1/TAP2 gene polymorphisms and HLA-DRB1*04 between RA patients and healthy controls. We concluded that the TAP2 gene codon 565 ‘A’ allele was associated with RA in Chinese patients in Taiwan. Individuals possessing the ‘A’ allele had a higher incidence of RA. A lack of association of TAP1 gene polymorphisms between RA patients and healthy individuals was noted. The results of this study provide genetic evidence that TAP2 gene codon 565 polymorphism may play a role in RA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rheumatoid arthritis (RA) is a chronic inflammatory disease affecting the synovial membranes of articulating joints [1]. There is evidence for immunopathogenesis in a genetic susceptible host [2, 3], but the genetic basis of RA is largely unknown. The major histocompatibility (MHC) class II region is an important susceptibility factor and the human leukocyte antigen (HLA)-DR4 has been associated with serious disease courses [4, 5]. The disease-associated HLA-DRB1*04 alleles (Dw4, Dw14) share a common sequence (amino acid position 70–74 of HVR3) or epitope [6]. Transporters associated with protein processing (TAP) genes are located within the class II region of the human HLA complex, between the DQ and DP loci [7]. TAP1 and TAP 2 polymorphisms have been identified in humans [8, 9, 10, 11]. If TAP1 and TAP2 genes occur within the HLA class II region and are polymorphic, TAP gene products may be important for RA immunopathogenesis from a functional point of view.
We used single nucleotide polymorphisms (SNP) as a tool to search for the genetic markers of RA [12, 13]. We hypothesized that the problems of whether TAP1 and TAP2 genes were associated with RA could be resolved using SNP. The AG polymorphisms at codon 333 and 637 of the TAP1 gene and codons 379, 665 and 565 of the TAP2 gene were previously reported by Kuwata et al. [14] Thus, the aim of this study was to investigate whether these polymorphisms were associated with RA in Chinese patients using polymerase chain reaction (PCR)-based restriction analysis. We compared genotype distributions and allelic frequencies in 100 patients with RA and 99 healthy individuals.
Materials and methods
We studied 100 Chinese patients with definite RA according to the 1987 revised American College of Rheumatology criteria [15]. The mean age of the patients was 52.2±13.4 years and the mean age at disease onset was 45.2±14.3 years. The mean duration of the disease was 7.0±5.9 years. Sixty-one patients were seropositive RA; 48% of the RA patients were HLA-DRB1*04 positive. In addition, 99 unrelated healthy individuals living in central Taiwan served as controls. Informed consent was obtained from each individual who participated in the study (Table 1).
Genotyping and PCR for TAP genes
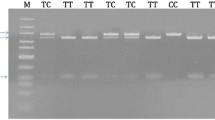
The genomic DNA was prepared from peripheral blood using a Genomaker DNA Extractor kit (Bloosm, Taiwan). Two sets of primers for the TAP1 gene and three sets of primers for the TAP2 gene were used. Nucleotide sequences of the primers are shown in Table 2. TAP1 and TAP2 genotyping was performed by the PCR-RFLP method using the specific primers shown in Table 2. Two dimorphic sites of TAP1–codons 333 and 637–were digested with DpnII and AccI, respectively. Three dimorphic sites of TAP2 –codons 379, 665, 565 –were digested using AccII, MspI and RsaI, respectively (Table 3). PCR was carried out to a total volume of 50 μl, containing genomic DNA, 2–6 pmol of each primer, 1X Taq polymerase buffer (1.5 mM MgCl2), and 0.25 units of AmpliTaq DNA polymerase (Perkin Elmer, Foster City, CA, USA). The PCR cycles consisted of an initial denaturation for 2 min at 94°C and 35 cycles of denaturation for 15 s at 94°C, annealing for 20 s at 60°C, and extension for 20 s at 72°C, which was followed by an extension of 10 min at 72°C. This cycling was performed in a programmable DNA Thermal Cycler (Perkin Elmer Cetus, Norwalk, Conn., USA). The PCR products were studied after restriction enzyme digestion (New England Biolabs, Beverly, Mass, USA). Then, 10 μl of the product was loaded into a 3% agarose gel containing ethidium bromide for electrophoresis.
HLA typing for DRB1*04
HLA-DRB1*04 typing was performed by PCR amplification with sequence-specific primers (RCR-SSP) described previously by Olerup [25].
Statistics
Allelic frequency was expressed as a percentage of the total number of alleles. Results from the control subjects and RA patients were compared using the χ2 test (2×2 contingency tables) for statistical significance. When the assumption of the χ2 test was violated, one cell had an expected count of <1 or >20% of the cells had an expected count of <5, Fisher’s exact test was used. The distributions of the TAP1 and TAP2 gene polymorphisms in each group were evaluated. A p value less than 0.05 was considered statistically significant. The odds ratios (OR) were calculated from allelic frequency with 95% confidence interval (95% CI) for the polymorphisms of the TAP genes. Linkage disequilibrium between alleles was calculated with the standardized disequilibrium coefficient.
Results
The basic data between RA patients and healthy control subjects, including mean age and female/male ratio, were compared. The results are shown in Table 1. There were no significant differences between the RA patients and healthy controls in either age or gender.
The frequencies of the genotypes in the RA patients and control subjects are shown in Table 4. There were no significance genotype frequencies of the TAP1 codons 333/637 and TAP2 codons 379/665 between RA patients and normal controls. The genotype distributions of AG polymorphisms at TAP2 codon 565 in the healthy subjects showed that 80 patients (80.8%) had the genotype GG and 19 patients (19.2%) had AG. Among the 100 RA patients, the genotype GG was found in 81 (81 %), AG in nine (9 %), and 10 patients (10%) had AA. There were no AA homozygotes in the healthy control group. There were significant statistical differences between the RA patients and the healthy subjects (χ2 test, p<0.001). The data were further subdivided into A and G groups according to the allelic frequencies in each group (Table 4). The allelic distribution of AG polymorphisms at the TAP2 codon 565 in healthy subjects who had the ‘A’ allele was 0.096, and in those with the ‘G’ allele was 0.904. In the RA patients who had the ‘A’ allele the distribution was 0.145, and in those with the ‘G’ allele was 0.855. There were no significant statistical differences in allelic frequencies between patients and controls. The odds ratio for the risk of the ‘A’ allele in RA patients was 1.60, with a 95% CI ranging from 0.82 to 2.92.
The Hardy–Weinberg (HW) equilibrium test was performed and results showed that distributions of all genotypes were in HW equilibrium, except for the TAP2–3 in RA patients (p<0.001). The allelic and genotype frequencies of all SNP are shown in Tables 4 and 5. Linkage disequilibrium between alleles was calculated with the standardized disequilibrium coefficient. The results showed that there were linkages between TAP1–1(A)/TAP1–2(G) (p<0.01), TAP1–1(G)/TAP1–2(G) (p<0.01), TAP 2–1(A)/TAP2–2(A) (p<0.05) in control subjects and TAP2–1(A)/TAP2–2(A) (p<0.01), TAP2–1(A)/TAP2–2(G) (p<0.05), TAP 2–2(A)/TAP2–3(A) (p<0.01), TAP2–2(A)/TAP2–3(G) (p<0.01) in patients (data not shown).
The associations of TAP1 and TAP2 alleles with HLA-DRB1*04 were estimated in RA patients and normal controls. The results are shown in Table 6. There were 48% of RA patients who carried HLA-DRB1*04. Only 27% of normal controls carried HLA-DRB1*04. No significance was observed in TAP1 and TAP2 gene polymorphisms between patients and controls. There was no linkage between HLA-DRB1*04 and TAP1/TAP2 gene polymorphisms.
Discussion
TAP1 and TAP2 genes located adjacent to the MHC class II region can control antigen presentation by class I molecules [16] and, as such, are candidate susceptibility genes for autoimmune diseases. Class I antigens may be important in the development of class II-associated disease, as for example in multiple sclerosis (MS). MS patients may have particular TAP alleles favoring the presentation of some viral or myelin autoantigen-driven peptides by HLA-class I molecules, which then initiates a strong T-cell mediated immune response leading to demyelination [17]. Defects in this process, mediated by transporter or MHC class I molecules, can have an influence on the T-cell repertoire, the response to diseases, and tolerance to self-antigens [18].
Polymorphisms in rat and murine TAP genes have been shown to alter the spectrum of peptides bound to MHC class I molecules [19]. It is possible that differences in human TAP genes could also cause alterations in translocation of the peptides. In human antigen-processing pathways the TAP molecule may play an exclusive role in selecting the size of peptides [20].
There has been little genetic evidence to support the hypothesis that TAP1 and TAP2 genes polymorphisms are associated in patients with RA. We investigated whether these polymorphisms were associated with Chinese patients with RA in Taiwan. The results demonstrated that only the prevalence of a variant of the TAP2 gene codon 565 polymorphism was significantly higher in RA patients than in controls. However, there were no associations of TAP1 gene codons 333 and 637, and TAP2 gene codons 379 and 665 between RA patients and control subjects.
Rheumatoid arthritis is a progressive, destructive disease characterized by inflammation, abnormal immune responses and synovial hyperplasia. There is strong epidemiological evidence that genes contribute to the risk of developing many common diseases [17, 18]. Genes susceptible to rheumatic diseases are being proved using serial association studies by screening DNA polymorphisms for some genes such as IL-1β, IL-1 receptor antagonist [21] and vitamin D receptor genes [12, 13]. Evidence shows that many genes contribute to disease susceptibility and each may contribute a small increase in risk [22]. The TAP2 gene codon 565 polymorphism was highly correlated with RA patients in our study. However, there are studies suggesting that the TAP 2 gene polymorphism in RA patients was linked with HLA-DRB1*01 [23, 24]. We did find some linkage disequilibrium between TAP1 and TAP2 variants, but our results showed no significance in TAP1 and TAP2 gene polymorphisms between DRB1*04-positive RA patients and control subjects. So, despite the physical linkage displayed by these TAP1/2 gene loci, they are not in linkage disequilibrium with HLA-DRB1*01. This evidence indicates that the TAP2 gene codon 565 polymorphism may be a genetic marker for RA. The association of genes with RA could provide further risk identification, improved preventive medicine, and a choice of unique treatment strategies for some patients with subtypes of the disease. Therefore, using single nucleotide polymorphism (SNP) genotyping is likely to become a part of the routine management of patients with RA in the future.
In conclusion, we determined the existence of TAP1 and TAP2 gene alleles in Chinese patients with RA in Taiwan. No association was observed with allele amino acid residue frequencies except TAP2 codon 565. There was no linkage with HLA-DRB1*01 in either RA patients or control subjects. Further functional studies of the antigen-processing pathway are needed to clarify the precise antigen-presentation mechanisms involved in the development of RA.
Abbreviations
- MHC:
-
Major histocompatibility
- MS:
-
Multiple sclerosis
- PCR:
-
Polymerase chain reaction
- RA:
-
Rheumatoid arthritis
- SNP:
-
Single nucleotide polymorphism
References
Krane SM, Simon LS (1986) Rheumatoid arthritis: clinical features and pathogenetic mechanisms. Med Clin North Am 70:263–284
Panayi GTS, Lanchbury JS, Kingsley GH (1992) The importance of the T cell in initiating and maintaining the chronic synovitis of rheumatoid arthritis. Arthritis Rheum 35:729–735
Moreland LW, Heck LW, Sullivan W, Pratt PW, Koopman WJ (1993) New approaches to the therapy of autoimmune diseases: Rheumatoid arthritis as a paradigm. Am J Med Sci 305:40–51
Wagner U, Kaltenhauser S, Sauer H et al. (1997) HLA markers and prediction of clinical course and outcome in rheumatoid arthritis. Arthritis Rheum 40:341–351
Van Zeben D, Hazes JMW, Zwinderman AH et al. (1991) Association of HLA-DR4 with a more progressive disease course in patients with rheumatoid arthritis: results of a followup study. Arthritis Rheum 34:822–830
Gregerson P, Silver J, Winchester R (1987) The shared epitope hypothesis. An approach to understanding the molecular genetics of susceptibility to rheumatoid arthritis. Arthritis Rheum 30:1205–1213
Ziegler A, Field LL, Sakaguchi AY (1991) Report of the committee on the genetic constitution of chromosome 6. Cytogenet Cell Genet 295–336
Kelly A, Powis SH, Glynne R, Radley E, Beck S, Trowsdale J (1990) A proteasome-related gene between the ABC transporter loci in the class II region of the human MHC. Nature 353:357–360
Powis SH, Mockridge I, Kelly A et al. (1992) Polymorphism in a second ABC transporter gene located within the class II region of the human major histocompatibility complex. Proc Natl Acad Sci USA 89:1463–1467
Colonna M, Bresnahan M, Bahram S, Strominger JL, Spies T (1992) Allelic variants of the human putative peptide transporter involved in antigen processing. Proc Natl Acad Sci USA 89:3932–3936
Aoki Y, Isselbacher KJ, Pillai S (1993) Polymorphisms involving the transmembrane domains of human TAP 2. Immunogenetics 38:382
Huang CM, Wu MC, Wu JY, Tsai FJ (2002) Association of vitamin-D receptor gene Bsm I polymorphisms in Chinese patients with systemic lupus erythematosus. Lupus 11:31–34
Huang CM, Wu MC, Wu JY, Tsai FJ (2002) No association of vitamin-D receptor gene start condon Fok I polymorphisms in Chinese patients with systemic lupus erythematosus. J Rheumatol 29:1121–1123
Kuwata S, Yanagisawa M, Saeki H et al. (1995) Lack of primary association between transporter associated with antigen processing genes and atopic dermatitis. J Allergy Clin Immunol 96:1051–1060
Arnett FC, Edworthy SM, Bloch DA et al. (1988) The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum 3:315–324
Monaco JJ (1992) A molecular model of MHC class I restricted antigen processing. Immunol Today 13:173–179
Hayashi T, Morimoto C, Burks JS, Kerr C, Hauser SL (1988) Dual-label immunocytochemistry of the active multiple sclerosis lesion: major histocompatibility complex and activation antigens. Ann Neurol 24:523–531
Faustmann DL (1993) Mechanisms of autoimmunity in type I diabetes. J Clin Immunol 47:3–10
Powis SJ, Deverson EV, Coadwell WJ (1992) Effect of polymorphism of an MHC-linked transporter on the peptides assembles in a class I molecule. Nature 357:211–215
Momburg F, Roelse J, Hammerling GJ (1994) Peptide size selection by the major histocompatibility complex-encoded peptide transporter. J Exp Med 179:1613–1623
Huang CM, Wu MC, Wu JY, Tsai FJ (2002) Lack of association of interleukin-1β gene polymorphisms in Chinese patients with systemic lupus erythematosus. Rheumatol Int 21:173–175
Mathew C (2001) Postgenomic technologies: hunting the genes for common disorders. Br Med J 322:1031–1034
Wordsworth BP, Pile KD, Gibson K, Burney RO, Mockridge I, Powis SH (1993) Analysis of the MHC-encoded transporters TAP1 and TAP2 in rheumatoid arthritis: linkage with DR4 accounts for the association with a minor TAP2 allele. Tissue Antigens 42:153–155
Vandevyver C, Geusens P, cassiman J-J, Raus J (1995) Peptide transporter genes (TAP) polymorphisms and genetic susceptibility to rheumatoid arthritis. Br J Rheumatol 34:207–214
Olerup O. Zetterquist H (1992) HLA-DR typing by PCR amplification with sequenc-specific primers (PCR-SSP) in 2 hours: An alternative to serological DR typing in clinical practice including donor-recipient matching in cadaveric transplantation. Tissue Antigens 39: 225–235
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yu, MC., Huang, CM., Wu, MC. et al. Association of TAP2 gene polymorphisms in Chinese patients with rheumatoid arthritis. Clin Rheumatol 23, 35–39 (2004). https://doi.org/10.1007/s10067-003-0769-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-003-0769-3