Abstract
The congenital muscular dystrophies (CMD) constitute a clinically and genetically heterogeneous group of autosomal recessive myopathies. Patients show congenital hypotonia, muscle weakness, and dystrophic changes on muscle biopsy. Mutations in four genes (FKT1, POMGnT1, POMT1, FKRP) encoding putative glycosyltransferases have been identified in a subset of patients characterized by a deficient glycosylation of α-dystroglycan on muscle biopsy. FKRP mutations account for a broad spectrum of patients with muscular dystrophy, from a severe congenital form with or without mental retardation (MDC1C) to a much milder limb-girdle muscular dystrophy (LGMD2I). We identified two novel homozygous missense FKRP mutations, one, A455D, in six unrelated Tunisian patients and the other, V405L, in an Algerian boy. The patients, between the ages of 3 and 12 years, presented with a severe form of MDC1C with calf hypertrophy and high serum creatine kinase levels. None had ever walked. Two had cardiac dysfunction and one strabismus. They all had mental retardation, microcephaly, cerebellar cysts, and hypoplasia of the vermis. White matter abnormalities were found in five, mostly when cranial magnetic resonance imaging was performed at a young age. These abnormalities were shown to regress in one patient, as has been observed in patients with Fukuyama CMD. Identification of a new microsatellite close to the FKRP gene allowed us to confirm the founder origin of the Tunisian mutation. These results strongly suggest that particular FKRP mutations in the homozygous state induce structural and clinical neurological lesions in addition to muscular dystrophy. They also relate MDC1C to other CMD with abnormal protein glycosylation and disordered brain function.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Congenital muscular dystrophies (CMD) constitute a heterogeneous family of autosomal recessively inherited diseases, presenting at birth or within the first few weeks of life with hypotonia, delayed motor development, and dystrophic changes on skeletal muscle biopsy [1]. Clinical heterogeneity is evidenced by different patterns of motor involvement, variable serum creatine kinase (CK) levels, and the presence or not of mental retardation and structural defects of the central nervous system (CNS). At least one-third of patients in western countries have a primary deficiency in the laminin α2 chain (merosin) resulting from mutations in the LAMA2 gene [2, 3, 4]. This type of CMD, usually referred to as merosin-deficient CMD, has now been classified as MDC1A and is always associated with diffuse white matter abnormalities, and occasionally cerebellar hypoplasia or abnormal lesions of the cerebral gyri [5, 6, 7]. Epileptic seizures have been reported in a subset of these patients. A secondary deficiency of laminin α2 and of α-dystroglycan is found in some CMD forms, including muscle-eye-brain disease (MEB), Walker-Warburg syndrome (WWS), Fukuyama CMD (FCMD), and MDC1C, mapped to chromosomes 1p32, 9q34, 9q31, and 19q13, respectively [8, 9, 10, 11]. These CMD are caused by defects in genes encoding putative glycosyltransferases: the POMGnT1 gene coding for an O-mannose glycosyltransferase (MEB) [8], the POMT1 gene coding for O-mannosyltransferase 1 (WWS) [9], the FKT1 gene encoding a protein of unknown function called fukutin (FCMD) [10], and FKRP, a homologue of the FKT1 gene (MDC1C) [11]. Clinically, the first three types show severe symptoms and structural CNS involvement. MDC1C is characterized by marked elevation of serum CK, early onset hypotonia, delayed or arrested motor development, muscle hypertrophy, and variable cardiomyopathy. However, no major CNS abnormalities have been described in initial reports of even the most-severe forms [11, 12]. Very recently, two homozygous FKRP mutations associated with mental retardation and cerebellar cysts have been identified in two Turkish patients [13]. They were isolated cases and, therefore, it was not possible to conclude if particular FKRP gene mutations may constitute a subset of patients with a particular phenotype characterized by severe neurological involvement.
To address this issue, we report two new FKRP mutations associated with CMD and mental retardation, one in a series of six unrelated Tunisian families and another in an Algerian patient. All patients had mental retardation and neuroimaging showed a variable combination of CNS abnormalities, including cerebellar cysts or atrophy with or without white matter lesions. These results suggest strongly that certain FKRP mutations induce structural and clinical neurological abnormalities in a subset of patients with MDC1C. They may contribute to the better understanding of this entity and relate this type of CMD to others with abnormal protein glycosylation and structural CNS abnormalities. In addition, identification of a new microsatellite close to the FKRP gene was used to investigate the founder origin of the Tunisian mutation.
Patients and methods
Patients
Seven unrelated patients belonging to six consanguineous Tunisian CMD families from southern Tunisia (patients 1–6) and one consanguineous Algerian CMD family (patient 7) were studied. The diagnosis of CMD was made on the basis of hypotonia and weakness at birth or within the first months of life, and dystrophic changes on muscle biopsy. In addition, all patients had a marked increase in serum CK. Muscle biopsies were obtained from the deltoid muscle in five patients and from the tibialis anterior muscle in patients 6 and 7. Brain magnetic resonance imaging (MRI) was available for patients 1, 2, 3, 4, 6, and 7 and patient 5 had a cerebral computed tomographic (CT) scan. Blood samples were collected from the members of these families after informed consent.
Immunohistochemistry
Unfixed frozen 8-μm sections were incubated with monoclonal antibodies binding specifically to the human laminin α2 chain 80-kilodalton (kDa) fragment towards the C-terminal region (MAB 1922 Chemicon) and the human merosin 300-kDa fragment towards the amino-terminal region (NLC-merosin Novo-Castra) in all patients. In addition, muscle sections of patients 6 and 7 were immunolabelled with α-dystroglycan antibodies (V1A4-1, 05298, Euromedex). All primary antibodies were applied for 1 h and developed using an appropriate secondary antibody (fluorescein isothiocyanate-conjugated rabbit anti-mouse immunoglobulins, Dako).
Linkage and haplotype analysis
Genetic analysis was performed on genomic DNA extracted from blood leukocytes using a standard phenol-chloroform procedure [14]. Microsatellites spanning the FKRP locus (D19S606, D19S412, D19S219, and fkrp 52) were studied. PCR amplification was carried out in 50 μl with 60 ng of genomic DNA, 1 μM of each primer, 125 μM dNTPs, 1.5 mM MgCl2, 5 mM KCl, 10 mM TRIS-HCl, pH 8.8, and 1 U of Taq DNA polymerase. PCR products were analyzed on 6% denaturing polyacrylamide gels, transferred to a N+ Hybond membrane (Amersham Pharmacia Biotech), and hybridized with a poly AC probe labeled with α-32P. The following primers were designed to amplify the new microsatellite, fkrp 52 (ID=ss12568442 in the NCBI SNP database): 5′-TCTCCAAAAAACAACAACAAC-3′ and 5′-CTAGTGTTCTGGGACCTTT-3′. The sequence of the amplified fragment is available in the Third Party Annotation Section of the DDBJ/EMBL/Genbank databases under the accession number TPA: BK001438.
FKRP mutational analysis
A 1.8-kb fragment containing the FKRP coding sequence of exon 4 and its bordering intronic sequences was amplified using five primer sets (Table 1). The overlapping PCR products were purified (Qiagen) and used for direct sequencing on both strands. Sequencing reactions were carried out using an ABI Prism Big Dye Terminator Cycle Sequencing Kit (Applied Biosystems). The 1364C>A mutation induces the loss of a NaeI restriction site. The NaeI restriction pattern of the FKRP 4-5 fragment (421 bp) was used to confirm the presence of the mutation in patients’ relatives and to screen 100 unrelated healthy Tunisian individuals. Digestion of PCR products was performed according to the manufacturer’s instructions (New England Biolabs), followed by separation on 2% Nusieve gels. The 1213G>T mutation identified in the FKRP 4-5 fragment was investigated by direct sequencing in 50 Algerian and 100 French healthy control individuals.
Results
Clinical and complementary findings
The main clinical features of the Tunisian (patients 1–6) and Algerian patients are summarized in Table 2.
Patients 1, 2, and 3
These patients have previously been described [15]; they presented a severe form of CMD with mental retardation and cerebellar cysts. The condition of these patients worsened progressively. For patient 1, brain MRI performed at ages 3 and 6 years showed a significant reduction of the white matter abnormalities with age (Fig. 1). In contrast, the hypoplasia of the pons and cerebellar cysts remained unchanged.
Patient 4
This patient was a 5-year-old girl. She had a severe form of CMD with mental retardation. Electromyography (EMG) was myopathic and muscle biopsy showed severe dystrophic features. Cranial MRI at 5 years of age revealed only cerebellar cysts without any white matter or other cerebellar abnormality (Fig. 2). Echocardiography showed left ventricular hypertrophy.
A Transverse T2-weighted MRI of patient 4 showing cerebellar cysts. B Clinical features of patient 6: severe facial weakness and tongue enlargement, wrist and flexor finger contractures without elbow contractures, severe distal amyotrophy, and spinal deformity. C Transverse T2-weighted MRI of patient 6 showing hypoplasia of cerebellar vermis and cerebellar cysts
Patient 5
This patient was a 6-year-old girl. She presented at birth with a severe form of CMD with axial and facial weakness and had mental retardation. The ophthalmological examination was normal. Brain CT scan had been performed at the age of 3 years and showed white matter abnormalities (not shown).
Patient 6
Patient 6 was a 12-year-old mentally retarded girl who had an older brother with CMD associated with encephalopathy who had died at the age of 3 years due to a pneumopathy. She was the oldest child of this series and was the most severely affected patient. She never walked. She showed a severe facial weakness, progressive weakness, macroglossia, limited ocular excursion, and scoliosis that was treated surgically. She was mechanically ventilated by 10 years of age because of severe restrictive respiratory insufficiency. At 12 years she was only able to perform minimal movements of the fingers, which were contracted in flexion (Fig. 2) and a mild cardiac involvement was detected, with a reduced shortening fraction and a normal ejection fraction. She did not speak before 5 years of age. At 12 years, she was able to say only single simple words of two or three syllables (verbal IQ 50) and her brain MRI showed cerebral atrophy, large white matter abnormalities, and hypoplasia of cerebellar vermis and cerebellar cysts (Fig. 2). The abnormal white matter signal was very diffuse in early life and regressed progressively.
Patient 7
This patient was a 3-year-old mentally retarded boy. He presented at birth with a severe form of CMD. EMG showed myopathic features and the muscle biopsy of the tibialis muscle showed severe dystrophic features. Electrocardiography, electroencephalography, and ophthalmological examination were normal. Brain MRI revealed cerebellar cysts, megacisterna with hypoplasia of the vermis, and an abnormally high periventricular intensity on T2-weighed images. At the age of 3 years, he was microcephalic and could say only a few words.
Immunocytochemistry
All the patients showed histological changes characteristic of muscular dystrophy, and reduced immunohistochemical staining of laminin α2 chain using antibodies against the 80- and the 300-kDa fragments. α-Dystroglycan expression was markedly reduced in the only two samples available (data not shown).
Mutation screening of the FKRP gene
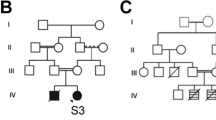
After exclusion of the CMD loci FCMD, MEB, MDC1A, and MDC1B in families 1–7 (data not shown), all patients were found to be homozygous for markers surrounding the FKRP locus (D19S219, D19S412, D19S606) on chromosome 19q13.3, suggesting homozygous mutations in FKRP. Sequencing of the FKRP coding region revealed the same homozygous transversion, 1364C>A, in the six Tunisian patients inducing the change of alanine 455 to a negatively charged aspartic acid (A455D) (Fig. 3). We took advantage of the loss of a NaeI restriction site induced by this mutation to exclude it as a non-pathogenic polymorphism. This variant was not found in 200 control chromosomes. Using NaeI digestion and direct sequencing, the mutation was found to segregate with the disease in an autosomal recessive fashion in the six consanguineous families (Figs. 4 and 5). A second homozygous transversion 1213G>T was identified in the Algerian patient changing valine 405 to leucine (V405L). This change was not found by direct sequencing in 50 Algerian and 100 French healthy control individuals.
Sequence chromatograms from normal individual (wild type, WT) and affected individuals (P) are shown together with the expected amino acid changes. Nucleotide variations are indicated by an arrow. A 1364C>A inducing the A455D mutation in patient 1 (P1), B 1213G>T inducing the V405L mutation in patient 7 (P7)
Restriction enzyme analysis showing the inheritance of the 1364C>A mutation in family 4. A 421-bp PCR fragment was digested with NaeI. Normal control DNA is cut into two fragments of 272 bp and 149 bp, whereas products containing the mutation remained uncut at 421 bp in patient 1. Only one of the two alleles was cut for parents and the two brothers who are heterozygous carriers of the A455D mutation
The pedigrees of the six Tunisian families showing the inheritance of the 1364C>A mutation. The haplotypes containing the mutation are boxed. We note the same founder haplotype for families 1, 2, 3, and 4. Families 5 and 6 had the same mutation but not the same haplotype. With the fkrp 52 all families shared the same founder allele (120 bp) transmitted with the Tunisian mutation
Since the six families originated from Tunisia, we searched for a founder origin of the mutation. The known markers flanking FKRP, D19S219, D19S412, and D19S606, were physically mapped according to the Human Genome Browser and Ensembl Genome Server maps (http://genome.cse.ucsc.edu/goldenPath/hgTracks.html and http://www.ensembl.org). They are located at 1,255 kb and 238 kb proximal and 722 kb distal to FKRP, respectively. Among the families tested, families 1–4 from the same region in the south of Tunisia shared the same alleles (Fig. 5), while the two others did not. We searched for new (CA)n microsatellite markers closer to FKRP. One was identified, fkrp 52, with alleles varying from 92 to 122 bp, 42 kb proximal to FKRP. A rare120-bp allele containing 26 CA repeats was shared by the six families, suggesting that the mutation has been transmitted by a common ancestor (Fig. 5).
Discussion
In this study, we report two new homozygous missense FKRP mutations in seven patients with MDC1C associated with mental retardation and CNS abnormalities. Six from Tunisia share the same mutation, which strongly suggests that this particular FKRP mutation in the homozygous state invariably lead to the CNS involvement.
Mutations in the FKRP gene previously reported account for a broad spectrum of patients with muscular dystrophy, from a severe congenital form (MDC1C) [11] to a much milder limb-girdle muscular dystrophy (LGMD2I) [16]. There are intermediate phenotypes that look like Duchenne muscular dystrophy. The intermediate and congenital forms may share an identical end-stage picture characterized by a paralytic atrophic-hypertrophic phenotype, including extreme diffuse weakness, tongue hypertrophy, and the need for continuous mechanical ventilation [11, 12]. Genotype-phenotype correlation has been shown by the identification of “mild” and “severe” mutations in cases with LGMD2I and MDC1C respectively, and which lead to an intermediate phenotype when combined [17, 18, 19]. In spite of differences in the degree of severity, a common phenotypic pattern, including some features such as high CK levels, muscle hypertrophy, a progressive course, and reduced expression of laminin α2 chain and α-dystroglycan in muscle, characterizes this entity.
The patients of our series presented with a typical MDC1C phenotype, but they also had severe psychomotor retardation and developed a microcephaly that was not observed at birth. They showed late and unsteady head control, inability to stand or walk, and marked mental retardation. Very high CK levels were common to all, and calf hypertrophy was noted in four patients. The oldest patient developed the typical paralytic atrophic-hypertrophic FKRP phenotype at the end of the first decade. This was not observed in the other six patients, probably because they were too young to manifest this progression, which is not usually observed in the first years of life [12]. All patients in our series showed white matter changes and/or cerebellar structural abnormalities on neuroimaging. We have previously reported minor signs of central involvement, such as speech delay, brain atrophy, and mild white matter lesions in some MDC1C patients. However, such findings were thought to be non-specific or secondary to hypoxic complications related to the respiratory insufficiency in advanced stages of the disease [12]. Therefore, MDC1C was initially classified as a CMD without neurological involvement, as distinct from the CMD syndromes with structural brain abnormalities, such as MEB, FCMD, and WWS. Brain abnormalities such as agyria, pachygyria or polymicrogyria, hypomyelination of the white matter, cerebellar cysts, or ponto-cerebellar hypoplasia are frequent findings in these three conditions [8, 9, 10]. In our series, brain MRI was available for six of the seven patients and revealed cerebellar cysts in all and hypoplasia of the vermis in five. MRI has not been performed in patient 5 and, therefore, we cannot exclude the presence of posterior fossa abnormalities in this patient. Our patients did not show any gyral malformation in contrast to what may be observed in MEB, FCMD, or WWS. White matter abnormalities were observed in five of our patients, with significant regression in one detected by serial MRI at 3 and 6 years of age. Such transient infra-myelination has also been described in MEB and FCMD [19, 20], while in primary laminin α2 chain-deficient CMD, brain white matter abnormalities do not regress with time. It is also noteworthy that one patient presented with strabismus and another with ophthalmoplegia in the 2nd decade of life.
Very recently, different FKRP homozygote mutations were identified in three Turkish patients, two with mental retardation, white matter changes, and cerebellar cysts [13], and another with a typical WWS (Beltran-Valero de Bernabé et al, personal communication). This finding raised the question of the role of specific homozygous FKRP mutations in the development of neurological disturbances. Our study revealing two new homozygous missense FKRP mutations, A455D and V405L, in seven additional patients of similar phenotype clearly supports this hypothesis. Fukutin-related protein has been localized in the Golgi apparatus [21]. It is involved in the glycosylation processing of α-dystroglycan, a heavily glycosylated membrane protein that forms a link between the actin-associated cytoskeleton and the extracellular matrix via the laminin α2 chain [22]. Hypoglycosylation of α-dystroglycan abolishes binding not only to laminin, but also to neurexin and agrin, and such abnormal interactions underlie the pathogenic mechanism of muscular dystrophy with brain abnormalities [23, 24]. The mutations identified in our patients, V405L and A455D, are localized in the C-terminal domain (catalytic domain) of the fukutin-related protein, where other severe MDC1C mutations (P448L, Y465S) without CNS involvement have also been identified. These different mutations may affect in various degrees the conformation or the catalytic activity of the protein and/or recognition sites for α-dystroglycan and other potential substrates [16]. In contrast, the two mutations reported by Topaloglu et al. [13], P315T and S221A, which cause a similar phenotype with CNS involvement are located outside the catalytic domain in the stem region. This region is believed to be involved in protein-protein interaction.
In summary, the report describes two new missense mutations in the FKRP gene in seven children with MDC1C, mental retardation, and CNS abnormalities. While brain white matter changes may regress with time, structural cerebellar abnormalities were present early in life and did not seem to progress. Our results support the existence of particular homozygous FKRP mutations associated with severe neurological involvement, and relate MDC1C to other CMD with abnormal protein glycosylation affecting brain function.
References
Dubowitz V, Fardeau M (1995) Proceedings of the 27th ENMC sponsored workshop on congenital muscular dystrophy, 22–24 April 1994, The Netherlands. Neuromuscul Disord 5:253–258
Tome FM, Evangelista T, Leclerc A, Sunada Y, Manole E, Estournet B, Barois A, Campbell KP, Fardeau M (1994) Congenital muscular dystrophy with merosin deficiency. CR Acad Sci [III] 317:351–357
Helbling-Leclerc A, Zhang X, Topaloglu H, Cruaud C, Tesson F, Weissenbach J, Tome FM, Schwartz K, Fardeau M, Tryggvason K, et al (1995) Mutations in the laminin alpha2-chain gene (LAMA2) cause merosin-deficient congenital muscular dystrophy. Nat Genet 11:216–218
Allamand V, Guicheney P (2002) Merosin-deficient congenital muscular dystrophy, autosomal recessive (MDC1A, MIM#156225, LAMA2 gene coding for alpha2 chain of laminin). Eur J Hum Genet 10:91–94
Philpot J, Cowan F, Pennock J, Sewry C, Dubowitz V, Bydder G, Muntoni F (1999) Merosin-deficient congenital muscular dystrophy: the spectrum of brain involvement on magnetic resonance imaging. Neuromuscul Disord 9:81–85
Pini A, Merlini L, Tome FM, Chevallay M, Gobbi G (1996) Merosin-negative congenital muscular dystrophy, occipital epilepsy with periodic spasms and focal cortical dysplasia. Report of three Italian cases in two families. Brain Dev 18:316–322
Sunada Y, Edgar TS, Lotz BP, Rust RS, Campbell KP (1995) Merosin-negative congenital muscular dystrophy associated with extensive brain abnormalities. Neurology 45:2084–2089
Yoshida A, Kobayashi K, Manya H, Taniguchi K, Kano H, Mizuno M, Inazu T, Mitsuhashi H, Takahashi S, Takeuchi M, Herrmann R, Straub V, Talim B, Voit T, Topaloglu H, Toda T, Endo T (2001) Muscular dystrophy and neuronal migration disorder caused by mutations in a glycosyltransferase, POMGnT1. Dev Cell 1:717–724
Beltran-Valero de Bernabe D, Currier S, Steinbrecher A, Celli J, Beusekom E van, Zwaag B van der, Kayserili H, Merlini L, Chitayat D, Dobyns WB, Cormand B, Lehesjoki AE, Cruces J, Voit T, Walsh CA, Bokhoven H van, Brunner HG (2002) Mutations in O-mannosyltransferase gene POMT1 give rise to the severe neuronal migration disorder Walker-Warburg syndrome. Am J Hum Genet 71:1033–1043
Kobayashi K, Nakahori Y, Miyake M, Matsumura K, Kondo-Iida E, Nomura Y, Segawa M, Yoshioka M, Saito K, Osawa M, Hamano K, Sakakihara Y, Nonaka I, Nakagome Y, Kanazawa I, Nakamura Y, Tokunaga K, Toda T (1998) An ancient retrotransposal insertion causes Fukuyama-type congenital muscular dystrophy. Nature 394:388–392
Brockington M, Blake DJ, Prandini P, Brown SC, Torelli S, Benson MA, Ponting CP, Estournet B, Romero NB, Mercuri E, Voit T, Sewry CA, Guicheney P, Muntoni F (2001) Mutations in the fukutin-related protein gene (FKRP) cause a form of congenital muscular dystrophy with secondary laminin alpha2 deficiency and abnormal glycosylation of alpha-dystroglycan. Am J Hum Genet 69:1198–1209
Quijano-Roy S, Galan L, Ferreiro A, Cheliout-Heraut F, Gray F, Fardeau M, Barois A, Guicheney P, Romero NB, Estournet B (2002) Severe progressive form of congenital muscular dystrophy with calf pseudohypertrophy, macroglossia and respiratory insufficiency. Neuromuscl Disord 12:466–475
Topaloglu H, Brockington M, Yuva Y, Talim B, Haliloglu G, Blake D, Torelli S, Brown SC, Muntoni F (2003) FKRP gene mutations cause congenital muscular dystrophy, mental retardation and cerebellar cysts. Neurology 60:988–992
Kawazaki ES (1990) Sample preparation from blood, cells, and other fluids. In: Innis M, Gelffand D, Snisky G, White T (eds) PCR protocols. A guide to methods and application. Academic Press, San Diego, pp 146–52
Triki C, Louhichi N, Meziou M, Choyakh F, Kechaou MS, Jlidi R, Mhiri C, Fakhfakh F, Ayadi H (2003) Merosin-deficient congenital muscular dystrophy with mental retardation and cerebellar cysts in three Tunisian patients unlinked to the LAMA2, FCMD, MEB and CMD1B. Neuromuscul Disord 13:4–12
Brockington M, Yuva Y, Prandini P, Brown SC, Torelli S, Benson MA, Herrmann R, Anderson LV, Bashir R, Burgunder JM, Fallet S, Romero N, Fardeau M, Straub V, Storey G, Pollitt C, Richard I, Sewry CA, Bushby K, Voit T, Blake DJ, Muntoni F (2001) Mutations in the ukutin related-protein gene (FKRP) identifies limb girdle muscular dystrophy 2I as a milder allelic variant of congenital muscular dystrophy MDC1C. Hum Mol Genet 10:2851–2859
Mercuri E, Brockington M, Straub V, Quijano-Roy S, Yuva Y, Herrmann R, Brown SC, Torelli S, Dubowitz V, Blake DJ, Romero NB, Estournet B, Sewry CA, Guicheney P, Voit T, Muntoni F (2003) Phenotypic spectrum associated with mutations in the fukutin-related protein gene. Ann Neurol 53:537–542
Quijano-RoyS, RomeroNB, LouhichiN, BrockingtonM, ManyH, YelizY, RichardP, EstournetB, MuntoniF, FardeauF, BaroisA, GuicheneyP (2002) FKRP (fukutin related protein) gene mutations associated with intermediate phenotype between CMD type 1C and LGMD2I (abstract). Neuromuscul Disord 12:743
Muntoni F, Valero de Bernabe B, Bittner R, Blake D, Bokhoven H van, Brockington M, Brown S, Bushby K Campbell KP, Fiszman M, Gruenewald S, Merlini L, Quijano-Roy S, Romero N, Sabatelli P, Sewry CA, Straub V, Talim H, Topaloglu H, Voit T, Yurchenco PD, Urtizberea JA, Wewer U, Guicheney P (2004) 114th ENMC International Workshop on Congenital Muscular Dystrophy (CMD), 17-19 January 2003, Naarden, The Netherlands (in press)
Osawa M, Sumida S, Suzuki N, Arai Y, Ikenaka H, Murasugi H, Shishikura K, Suzuki H, Saito K, Fukuyama Y (1997) Fukuyama type congenital progressive muscular dystrophy.In: Fukujama Y, Osawa M, Saito K (eds) Congenital muscular dystrophies. Elsevier Science, pp 31–68
Esapa CT, Benson MA, Schroder JE, Martin-Rendon E, Brockington M, Brown SC, Muntoni F, Kroger S, Blake DJ (2002) Functional requirements for fukutin-related protein in the Golgi apparatus. Hum Mol Genet 11:3319–3331
Ervasti JM, Campbell KP (1993) A role for the dystrophin-glycoprotein complex as a transmenbrane linker between laminin and actin. J Cell Biol 122:809–823
Michele DE, Barresi R, Kanagawa M, Saito F, Cohn RD, Satz JS, Dollar J, Nishino I, Kelley RI, Somer H, Straub V, Mathews KD, Moore SA, Campbell KP (2002) Post-translational disruption of dystroglycan-ligand interactions in congenital muscular dystrophies. Nature 418:417–422
Moore SA, Saito F, Chen J, Michele DE, Henry MD, Messing A, Cohn RD, Ross-Barta SE, Westra S, Williamson RA, Hoshi T, Campbell KP (2002) Deletion of brain dystroglycan recapitulates aspects of congenital muscular dystrophy. Nature 418:422–425
Acknowledgements
We thank the patients and their families for their participation. This work was supported by funds from the Secrétariat d’Etat à la Recherche Scientifique et à la Technologie (Tunisia), the Institut National de la Santé et de la Recherche Médicale (INSERM), Association Française contre les Myopathies (AFM), and the European Commission (contract no. QLG1-CT1999-00870).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Louhichi, N., Triki, C., Quijano-Roy, S. et al. New FKRP mutations causing congenital muscular dystrophy associated with mental retardation and central nervous system abnormalities. Identification of a founder mutation in Tunisian families. Neurogenetics 5, 27–34 (2004). https://doi.org/10.1007/s10048-003-0165-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10048-003-0165-9