Abstract
The purpose of this study was to determine the accuracy of acetabular cup insertion during total hip arthroplasty (THA) in a supine position using an accelerometer-based portable navigation system. A single-surgeon study was conducted in which 62 prospective patients with navigation and 42 retrospective patients without navigation as historical controls were compared. The patients underwent THA via an anterolateral supine approach. The absolute values of errors of radiographic inclination and anteversion were calculated. The navigation error was also calculated. The factors that affected the absolute values of errors of cup alignment were determined. The mean absolute error of the postoperative CT measurement from the target angle for radiographic inclination was 3.8° in the navigation group and 6.6° in the control group (P < 0.001). The mean absolute error for anteversion was 3.3° in the navigation group and 5.9° in the control group (P < 0.001). The mean absolute values of navigation error were 3.7° ± 2.8° in inclination and 3.0° ± 2.6° in anteversion. Changes in the pelvic tilt angle among preoperative, intraoperative, and postoperative were the significant risk factors for the absolute values of navigation error of anteversion relative to the anterior pelvic plane. Other factors affecting the absolute values of errors in the navigation group were not found for radiographic inclination and anteversion. The portable navigation system significantly improved the accuracy of cup inclination and anteversion. Changes in the pelvic tilt were the risk factors for the error of anteversion relative to the anterior pelvic plane.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Achieving accurate acetabular cup positioning during total hip arthroplasty (THA) is important to prevent dislocation [1, 2], impingement [3], and acetabular wear, as well as loosening [4]. To reduce the rate of dislocation, anterior and anterolateral approaches are reported to be useful [5]. Watson-Jones approach is modified as a mini-incision anterolateral approach. It separates the inter-muscular plane between the gluteus medius and tensor fasciae latae [6]. The modified Watson-Jones approach can be used in both the supine position (abbreviated ALS) and the lateral decubitus position. Although surgeons select either the supine position or the lateral decubitus position in the modified Watson-Jones approach, it is still unclear which position is superior to achieve more accurate cup insertion without navigation. The supine position allows for better pelvic stability and landmark availability during THA [7]. Using a mechanical alignment guide, a higher accuracy of acetabular cup inclination was reported in the supine position than in the lateral decubitus position in THA [8]. When the direct anterior approach (DAA) and mini-posterior approach were compared, DAA achieved accurate cup positioning [9]. In contrast, THA performed with the patient in the supine position had a higher rate of outliers of cup inclination compared with the lateral decubitus position using the modified Watson-Jones approach [10].
Placement with navigation is more precise with improved accuracy for cup inclination and anteversion than conventional placement [11, 12]. Computed tomography (CT)-based navigation and image-free navigation have been developed and used in clinical settings. High cost when starting to use these navigation systems might be the greatest problem [11, 12]. In CT-based navigation, there have been concerns regarding increased planning time and radiation to the patients. An accelerometer-based portable navigation system (KneeAlign, OrthAlign, Aliso Viejo, CA) was developed for total knee arthroplasty, comprising accelerometers, gyroscopes, and inertial detectors to communicate between a reference sensor and a display unit, with much less cost [13,14,15]. Results using KneeAlign were comparable to large-console navigation [13, 14]. Accelerometer-based portable navigation systems have also been developed for total hip arthroplasty (HipAlign, OrthAlign).
The hypothesis was that use of HipAlign in ALS is more accurate for acetabular cup placement in THA than the conventional technique. In addition, risk factors for navigation error were determined.
Materials and methods
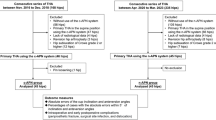
Between July 2017 and March 2019, 62 prospective consecutive patients underwent primary THA via an ALS approach using HipAlign. A G7 PPS Finned BoneMaster Acetabular Shell (Zimmer Biomet, Warsaw, IN) was used in all patients. As a control group, 42 retrospective consecutive patients who underwent THA via an ALS approach using the same acetabular cup between June 2015 and June 2017 were included. Patient demographic characteristics are shown in Table 1.
The navigation unit was calibrated on a flat table. Two fixation pins, 4.0 mm in diameter, were placed on the iliac crest to fix the navigation unit. The bilateral anterior superior iliac spines and pubic symphysis were registered as anatomical landmarks to define the anterior pelvic plane (APP). However, registration of the pubic symphysis has no effect on cup position in HipAlign. The functional pelvic plane (FPP) is defined as a reference plane where the APP is rotated about the inter-ASIS axis until its superior-inferior axis is parallel to the table plane at the time of registration in this navigation system. Cup angles are shown relative to the FPP.
All surgeries were performed with the patients in the supine position via an ALS approach under general anesthesia by a single surgeon (MH). After the neck cut and acetabular reaming, a navigation sensor was attached to a cup impactor. All cases were press fit fixation after 1-mm under-reaming without screw fixation. The target angle of cup inclination was 40° in all hips. The anteversion in the hips with navigation was targeted to 15° relative to the FPP. However, in the manual group, target anteversion was 20° relative to the operation table, because we can use a mechanical guide only for 20° anteversion. For all analyses, the radiographic angle values were used based on the definitions by Murray [16]. Radiographic inclination and anteversion angles of the cup, based on the FPP, were displayed on the monitor. We checked the inclination and anteversion angles before impaction of the cup, and adjusted to the aiming angles, and the final inclination and anteversion angles were re-checked after cup impaction [17]. When the angles were different between before and after cup impaction, the angle after cup impaction was adopted for intraoperative navigation record. These angles based on the APP were also presented on the monitor. Intraoperative pelvic tilt can be measured to see the monitor during surgery (Fig. 1). A TaperLoc Microplasty stem (Zimmer Biomet) was used, and ceramic on polyethylene articulation was selected for all hips. Computed tomography (CT) was performed from the pelvis to the knee joint 2 weeks postoperatively. Postoperative component positions were measured by uploading three-dimensional DICOM data to dedicated software (ZedHip, Lexi, Tokyo, Japan). Cup inclination and anteversion angles were measured with respect to the FPP and the APP by one observer (YN). The measurements were taken twice to evaluate intra-observer reliability of CT assessment in the first 20 cases. To evaluate the inter-observer reliability, the radiographic inclination and anteversion were measured in the first 20 cases by another observer (MH).
The absolute values of errors of radiographic inclination and radiographic anteversion were calculated by subtracting the intraoperative target angles from the target angles (postoperative CT measurement–preoperative target angle) with respect to the FPP. To analyze the accuracy of intraoperative navigation records for cup inclination and anteversion, the intraoperative cup angles using navigation records were compared with the postoperative angles using postoperative CT data relative to preoperative FPP and APP. The navigation error was calculated by subtracting the angles of the intraoperative navigation record from the angles of postoperative CT measurement (postoperative CT measurement–navigation record).
Pelvic tilt is defined as the angle between the APP and FPP. The preoperative FPP in the supine position was interpreted as a plane parallel to the CT table [18, 19]. The FPP was used as a reference plane for cup orientation. Changes in pelvic tilt were examined between the preoperative CT measurement and the intraoperative navigation record (navigation record–preoperative CT measurement), between the intraoperative navigation record and the postoperative CT measurement (postoperative CT measurement–navigation record), and between the preoperative CT measurement and the postoperative CT measurement (postoperative CT measurement–preoperative CT measurement). The absolute values of errors of measured postoperative angles from the target angles for radiographic inclination and anteversion were compared between the groups. The factors that affected the errors in the navigation group were determined. The percentage of the hips inside the Lewinnek safe zone (inclination between 30° and 50°, anteversion between 15° and 35°) was compared [1]. All patients were followed after THA, and complications and dislocation were examined. Our institutional review board approved this study.
Statistical analysis
From a previous portable navigation study [15], the differences (mean ± standard deviation) in the navigation and conventional groups of the cup inclination and anteversion were 2.8 ± 2.4 and 3.0 ± 2.3, respectively. Based on this finding, a sample size of 12 hips was needed in each group to detect a difference between the two groups (α = 0.05, power = 0.8). Intra-observer and inter-observer reliabilities were analyzed using the intraclass correlation coefficient (ICC). The ICC was classified as poor (less than 0.40), moderate (0.40–0.60), good (0.61–0.80), and very good (0.81–1.00) [20].
Patients’ demographic characteristics including age and body mass index (BMI) were compared between the two groups using the Mann–Whitney U test. The Chi-squared test and Fisher’s exact test were used to compare sex, diagnosis, and Crowe group. The Mann–Whitney U test was used to determine the differences (errors) between the intraoperative target angles or the intraoperative navigation records and postoperative CT measurements. The Chi-squared test and Fisher’s exact test were used to compare the hips that were within 5° and 10° of error in the navigation group, as well as the cups inside the “safe zone”, as detailed by Lewinnek et al. [1] (Lewinnek safe zone). Spearman’s rank correlation test was used to examine pelvic tilt preoperatively and postoperatively.
The factors that affected the absolute values of errors of cup alignment on both the FPP and the APP were determined. Correlation analyses were performed using Spearman’s rank correlation test. In these analyses, dependent variables included age, BMI, Crowe group, preoperative pelvic tilt, and changes in pelvic tilt among preoperative, intraoperative, and postoperative values. A value of P < 0.05 was considered significant. IBM SPSS Statistics Version 24 (IBM Corp., Armonk, NY) was used.
Results
There were no significant differences in patients’ demographic characteristics between the two groups. The intra-observer reliabilities were 0.915 and 0.963 in inclination and anteversion, respectively. The inter-observer reliabilities were 0.951 and 0.937 in inclination and anteversion, respectively. The mean postoperative radiographic inclination relative to the FPP was 37.5° ± 3.9° (range 30.2°–49.6°) in the navigation group and 34.6° ± 5.8° (range 20.9°–48.1°) in the control group. The mean postoperative radiographic anteversion relative to the FPP was 14.8° ± 4.2° (range 7.2°–25.7°) in the navigation group and 21.4° ± 7.0° (range 7.2°–39.5°) in control group. The mean absolute errors of the postoperative measured angles from the target angles for radiographic inclination and anteversion (postoperative CT measurement–target angle) are shown in Table 2. The navigation group showed better results both in inclination and anteversion. The mean absolute values of navigation error (postoperative CT–navigation record) were 3.7° ± 2.8° in inclination and 3.0° ± 2.6° in anteversion. The percentages of hips with error over 5° were 31% and 19% in radiographic inclination and anteversion, respectively. The percentage of hips with error over 10° was 2% in both radiographic inclination and anteversion. The mean postoperative radiographic inclination and anteversion relative to the APP in the navigation group were 38.0° ± 4.0° (range 30.6°–47.9°) and 16.3° ± 7.7° (range − 3.2° to 30.1°), respectively. The percentage of cups inside the Lewinnek safe zone was 98.4% in the navigation group and 66.7% in control group. Significantly more cups were inside the Lewinnek safe zone in the navigation group (P < 0.001). A strong correlation was found between preoperative and postoperative pelvic tilt (R = 0.919, P < 0.001). Change in the pelvic tilt angle between preoperative and intraoperative was the significant risk factor for the absolute values of navigation error of radiographic anteversion relative to the APP. Intraoperative anterior tilt was associated with small error, and intraoperative posterior tilt was associated with large error (R = − 0.630, P < 0.001, Fig. 2a). Change in the pelvic tilt angle between preoperative and postoperative was the significant risk factor for the absolute values of navigation error of radiographic anteversion relative to the APP. Postoperative anterior tilt was associated with small error, and postoperative posterior tilt was associated with large error (R = − 0.327, P = 0.009, Fig. 2b). In addition, change in the pelvic tilt angle between intraoperative and postoperative was the significant risk factor for the absolute values of navigation error of radiographic anteversion relative to the APP. Postoperative anterior tilt was associated with small error, and postoperative posterior tilt was associated with large error (R = − 0.606, P < 0.001, Fig. 2c). Other factors affecting the absolute values of errors in the navigation group were not found for radiographic inclination and anteversion.
Correlation between the absolute values of radiographic anteversion error relative to the APP and change in pelvic tilt. a intraoperative navigation measurement–preoperative CT measurement. b Postoperative CT measurement–preoperative CT measurement. c postoperative CT measurement–intraoperative navigation measurement. APP anterior pelvic plane, CT computed tomography
In the navigation group, there were no complications arising at the pin sites, and no dislocations occurred in any hips. In the control group, no dislocation occurred in any hips.
Discussion
The present study demonstrated that the portable navigation system significantly improved the accuracy of cup inclination and anteversion. There were significantly more cups inside the Lewinnek safe zone in the navigation group. In CT-based navigation, the absolute values of inclination errors were reported to range from 1.2° to 4.6°, and the anteversion errors ranged from 1.0° to 4.4° [21,22,23,24,25,26]. In image-free large-console navigation, the inclination errors were reported to range from 2.9° to 3.2°, and the anteversion errors ranged from 3.7° to 6.5° [4, 21, 27,28,29] (Table 3). Anteversion with CT-based navigation systems has been reported to have superior accuracy compared to the imageless large-console navigation systems. Anteversion of image-free navigation is based on the APP, which does not contain the pelvic tilt angle. If a patient has normal sagittal alignment (neutral pelvic tilt), the FPP is the same as the APP. In most patients, the FPP differs from the APP. The APP is hard to determine using a lateral radiograph of the pelvis. Furthermore, one should determine target tilt-adjusted anteversion before surgery using CT to convert the FPP. The thickness of the soft tissue overlying the pubic symphysis has an effect on the accuracy in anteversion. Accurate registration of the APP is required to achieve greater consistency in cup placement with image-free large-console navigation.
Compared with CT-based navigation and image-free large-console navigation, only a few minutes were required for HipAlign preparation before and during surgery. One of the most useful points of HipAlign with the patient in the supine position is that surgeons can know the cup angles relative to the FPP. In addition, there is no requirement to register the pubic symphysis for determining the APP, which could contribute to improved accuracy of anteversion using HipAlign. If surgeons ignore the relationship between the FPP and APP, HipAlign can be used in the same manner in all hips. In addition, HipAlign shows the radiographic angle during surgery, and the surgeon is not required to convert the anatomical or operative angle to the radiographic angle. The present study demonstrated that posterior tilt during or after THA was associated with navigation error of radiographic anteversion relative to the APP. If pelvic tilt calculated by HipAlign shows posterior tilt compared to preoperative CT during surgery, surgeons might be cautioned against navigation error of radiographic anteversion relative to the APP. Using only the FPP, surgeons could not find the risk factors for navigation error.
Absolute values of errors using HipAlign were reported to range from 2.6° to 3.7°, and the anteversion errors ranged from 2.7° to 3.8° in the supine position [17, 19, 30, 31]. All reports included hip dysplasia. In the lateral position, Tanino et al. [15] reported that the error in anteversion was 6.0° (Table 4). Patient positioning before skin incision could affect the error in anteversion in the lateral position. The supine position seems to be better for anteversion accuracy when working with accelerometers and gyroscopes. Our study had both navigation group and control group, and we showed the advantage of using HipAlign via ALS. The study by Hayashi et al. [30] also had both navigation group and control group. However, the studies by Kamenaga et al. [17] and Takada et al. [19] had no control groups. And these two studies failed to demonstrate the advantage of using HipAlign, and risk factors for navigation error were not determined. Patient volumes using navigation were 63, 75, and 30 in the studies by Hayashi et al. [30], Kamenaga et al. [17], and Takada et al. [19], respectively. All studies in Table 4 showed no consideration of changes of pelvic tilt before, intraoperative, and after surgery. Only our study evaluated pelvic tilt including cup position relative to the APP.
Most navigation systems including the HipAlign need no radiation exposure during surgery. Intraoperative feedback of preoperative CT scans increases surgical time. HipAlign can be used without radiation exposure preoperatively and intraoperatively. Some previous studies used a screw for cup fixation [15, 19]. In the present study, supplemental screw fixation was not used. If screws were inserted after checking cup position using navigation, the cup angles might be changed [32, 33]. In addition, error analysis was affected by changing the cup position after screw fixation. Press fit without a screw is the strong point in the present study to minimize the evaluation for navigation error.
The limitations of this study include the small number of patients and the lack of clinical results in cases without dislocation. In addition, absolute values of navigation error relative to the FPP was not determined. Further studies are needed to show the clinical advantages of the HipAlign. Cost-utility analyses are also required.
Conclusion
In THA via the ALS, HipAlign significantly improved the accuracy of cup inclination and anteversion, with the mean error of 3.7° in inclination and 3.0° in anteversion, including cases of hip dysplasia. Changes in the pelvic tilt angle between preoperative and intraoperative, preoperative and postoperative, as well as intraoperative and postoperative were the significant risk factors for the absolute values of navigation error of radiographic anteversion relative to the APP. Posterior tilt during or after THA was associated with navigation error of anteversion relative to the APP.
References
Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978;60-A:217–20.
Seagrave KG, Troelsen A, Malchau H, Husted H, Gromov K. Acetabular cup position and risk of dislocation in primary total hip arthroplasty. Acta Orthop. 2017;88:10–7.
McCarthy TF, Alipit V, Nevelos J, Elmallah RK, Mont MA. Acetabular cup anteversion and inclination in hip range of motion to impingement. J Arthroplasty. 2016;31:264–8.
Lass R, Kubista B, Olischar B, Frantal S, Windhager R, Giurea A. Total hip arthroplasty using imageless computer-assisted hip navigation: a prospective randomized study. J Arthroplasty. 2014;29:786–91.
Sheth D, Cafri G, Inacio MC, Paxton EW, Namba RS. Anterior and anterolateral approaches for THA are associated with lower dislocation risk without higher revision risk. Clin Orthop Relat Res. 2015;473:3401–8.
Bertin KC, Röttinger H. Anterolateral mini-incision hip replacement surgery: a modified Watson-Jones approach. Clin Orthop Relat Res. 2004;429:248–55.
Grammatopoulos G, Gofton W, Cochran M, Dobransky J, Carli A, Abdelbary H, et al. takadaPelvic positioning in the supine position leads to more consistent orientation of the acetabular component after total hip arthroplasty. Bone Joint J. 2018;100-B:1280–8.
Takada R, Jinno T, Miyatake K, Hirao M, Yagishita K, Yoshii T, et al. Supine versus lateral position for accurate positioning of acetabular cup in total hip arthroplasty using the modified Watson-Jones approach: a randomized single-blind controlled trial. Orthop Traumatol Surg Res. 2019;105:915–22.
Nakata K, Nishikawa M, Yamamoto K, Hirota S, Yoshikawa H. A clinical comparative study of the direct anterior with mini-posterior approach: two consecutive series. J Arthroplasty. 2009;24:698–704.
Kishimura Y, Minoda Y, Mizokawa S, Sugama R, Ohta Y, Nakamura H. Cup alignment in total hip arthroplasty using the muscle-sparing modified Watson-Jones approach-comparison between lateral and supine positions. Int Orthop. 2019;43:2477–83.
Beckmann J, Stengel D, Tingart M, Götz J, Grifka J, Lüring C. Navigated cup implantation in hip arthroplasty. Acta Orthop. 2009;80:538–44.
Snijders T, van Gaalen SM, de Gast A. Precision and accuracy of imageless navigation versus freehand implantation of total hip arthroplasty: a systematic review and meta-analysis. Int J Med Robot. 2017. https://doi.org/10.1002/rcs.1843.
Goh GS, Liow MHL, Tay DK, Lo NN, Yeo SJ, Tan MH. Accelerometer-based and computer-assisted navigation in total knee arthroplasty: a reduction in mechanical axis outliers does not lead to improvement in functional outcomes or quality of life when compared to conventional total knee arthroplasty. J Arthroplasty. 2018;33:379–85.
Shihab Z, Clayworth C, Nara N. Handheld, accelerometer-based navigation versus conventional instrumentation in total knee arthroplasty: a meta-analysis. ANZ J Surg. 2020. https://doi.org/10.1111/ans.15925.
Tanino H, Nishida Y, Mitsutake R, Ito H. Portable accelerometer-based navigation system for cup placement of total hip arthroplasty: a prospective, randomized, controlled study. J Arthroplasty. 2020;35:172–7.
Murray DW. The definition and measurement of acetabular orientation. J Bone Jt Surg Br. 1993;75:228–32.
Kamenaga T, Hayashi S, Hashimoto S, Matsumoto T, Takayama K, Fujishiro T, et al. Accuracy of cup orientation and learning curve of the accelerometer-based portable navigation system for total hip arthroplasty in the supine position. J Orthop Surg (Hong Kong). 2019;27:2309499019848871.
Sugano N. Computer-assisted orthopaedic surgery and robotic surgery in total hip arthroplasty. Clin Orthop Surg. 2013;5:1–9.
Takada R, Jinno T, Miyatake K, Hirao M, Yoshii T, Okawa A. Portable imageless navigation system and surgeon’s estimate for accurate evaluation of acetabular cup orientation during total hip arthroplasty in supine position. Eur J Orthop Surg Traumatol. 2020;30:707–12.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–74.
Kalteis T, Handel M, Bäthis H, Perlick L, Tingart M, Grifka J. Imageless navigation for insertion of the acetabular component in total hip arthroplasty: is it as accurate as CT-based navigation? J Bone Joint Surg Br. 2006;88:163–7.
Yamada K, Endo H, Tetsunaga T, Miyake T, Sanki T, Ozaki T. Accuracy of cup positioning with the computed tomography-based two-dimensional to three-dimensional matched navigation system: a prospective, randomized controlled study. J Arthroplasty. 2018;33:136–43.
Kajino Y, Kabata T, Maeda T, Iwai S, Kuroda K, Tsuchiya H. Does degree of the pelvic deformity affect the accuracy of computed tomography-based hip navigation? J Arthroplasty. 2012;27:1651–7.
Iwana D, Nakamura N, Miki H, Kitada M, Hananouchi T, Sugano N. Accuracy of angle and position of the cup using computed tomography-based navigation systems in total hip arthroplasty. Comput Aided Surg. 2013;18:187–94.
Tsutsui T, Goto T, Wada K, Takasago T, Hamada D, Sairyo K. Efficacy of a computed tomography-based navigation system for placement of the acetabular component in total hip arthroplasty for developmental dysplasia of the hip. J Orthop Surg (Hong Kong). 2017;25:1–7.
Nakahara, Kyo T, Kuroda Y, Miki H. Effect of improved navigation performance on the accuracy of implant placement in total hip arthroplasty with a CT-based navigation system. J Artif Organs. 2018;21:340–7.
Ybinger T, Kumpan W, Hoffart HE, Muschalik B, Bullmann W, Zweymüller K. Accuracy of navigation-assisted acetabular component positioning studied by computed tomography measurements: methods and results. J Arthroplasty. 2007;22:812–7.
Tsukada S, Wakui M. Decreased accuracy of acetabular cup placement for imageless navigation in obese patients. J Orthop Sci. 2010;15:758–63.
Fukunishi S, Nishio S, Fujihara Y, Okahisa S, Takeda Y, Fukui T, et al. Accuracy of combined anteversion in image-free navigated total hip arthroplasty: stem-first or cup-first technique? Int Orthop. 2016;40:9–13.
Hayashi S, Hashimoto S, Takayama K, Matsumoto T, Kamenaga T, Fujishiro T, et al. Evaluation of the accuracy of acetabular cup orientation using the accelerometer-based portable navigation system. J Orthop Sci. 2020;25:612–7.
Okamoto M, Kawasaki M, Okura T, Ochiai S, Yokoi H. Comparison of accuracy of cup position using portable navigation versus alignment guide in total hip arthroplasty in supine position. Hip Int. 2020. https://doi.org/10.1177/1120700020908788(Epub ahead of print).
Fujishiro T, Hayashi S, Kanzaki N, Hashimoto S, Shibanuma N, Kurosaka M. Effect of screw fixation on acetabular component alignment change in total hip arthroplasty. Int Orthop. 2014;38:1155–8. https://doi.org/10.1007/s00264-013-2271-0.
Tetsunaga T, Fujiwara K, Endo H, Tetsunaga T, Miyake T, Yamada K, et al. Changes in acetabular component alignment due to screw fixation in patients with hip dysplasia. Hip Int. 2019;29:535–42. https://doi.org/10.1177/1120700019828708.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no commercial associations that might pose a conflict of interest in connection with this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hasegawa, M., Naito, Y., Tone, S. et al. Accuracy of acetabular cup insertion in an anterolateral supine approach using an accelerometer-based portable navigation system. J Artif Organs 24, 82–89 (2021). https://doi.org/10.1007/s10047-020-01206-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10047-020-01206-8