Abstract
Basic fibroblast growth factor (bFGF) promotes epithelial cell proliferation and angiogenesis but its clinical applications are limited by its short half-life and low retention. Recently developed gelatin hydrogel sheets able to release physiologically active substances in a controlled manner have the potential to overcome these issues. In this study, the effects of gelatin hydrogel sheets impregnated with bFGF on flap survival and angiogenesis were examined in a murine skin flap model. A flap of 1 × 3 cm was generated on the backs of 60 C57BL/6 mice. The mice were divided into five groups (n = 12/group): Group I, untreated; Group II, treated with a gelatin hydrogel sheet impregnated with saline; Group III, treated with bFGF (50 µg) without sheets; Groups IV and V, treated with gelatin hydrogel sheets impregnated with 50 and 100 µg of bFGF, respectively. On the seventh day after surgery, the flap survival area and vascular network were examined and hematoxylin and eosin and von Willebrand factor staining were used for histological examinations. The flap survival areas were significantly larger in Groups IV and V than in other groups. The area of new vessels was significantly larger in Group IV than in the other groups. In the murine skin flap model, gelatin hydrogel sheets impregnated with bFGF promoted angiogenesis and improved flap survival. These findings support the use of bFGF-impregnated gelatin hydrogel sheets for improving ischemic flap survival in clinical settings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Surgical skin flaps are typically indicated for the reconstruction of skin and soft tissue defects, particularly after tumor resection or trauma. Safe and reliable engraftment of the flap is important for plastic and reconstructive surgery. However, these flaps offer limited coverage due to a lack of adequate blood flow, particularly at the distal ends. It is important to evaluate the surviving area of skin flap close to the necrosis area at the distal side because the motivation of this study is to overcome a lack of adequate blood flow in the skin at the distal ends. Various methods have been evaluated to prevent necrosis and ensure flap engraftment, including the injection of growth factors [1] and drug administration [2]; however, clinically effective engraftment methods have not been established.
Basic fibroblast growth factor (bFGF), also called fibroblast growth factor-2 (FGF-2), is a heparin-binding growth factor [3]. Over 20 FGF isoforms have been identified to date, with chemotactic, angiogenic [4], mitogenic [4], and adipogenic [5, 6] activity as well as important roles in early differentiation and developmental processes. In Japan, bFGF products have been approved for clinical applications, with well-known benefits for the treatment of bedsores and cutaneous ulcers. However, due to its short half-life and low retention rate at local sites, a single dose of bFGF does not provide a continuous effect that results in the maturation of new vessels and proliferation of fibroblasts.
To facilitate the sustained release of angiogenic factors, bioabsorbable gelatin hydrogels have recently been developed as drug delivery systems (DDS) for sustained release. In gelatin hydrogel sheets, immobilized acidic gelatin hydrogel molecules slowly dissolve, resulting in the controlled exudation of the integrated drug to the surrounding extracellular matrix with biodegradation of the hydrogel sheet [7]. From a tissue-engineering viewpoint, we evaluated the feasibility of improving the surgical skin flap engraftment rate by the sustained release of bFGF in vivo using a gelatin hydrogel sheet as a DDS. In particular, we explored whether or not the engraftment rate and flap viability of murine skin flaps were improved by using gelatin hydrogel sheets containing bFGF. We also assessed vascularization based on the flap survival area, histological examinations, and imaging analyses of new blood vessels in the flaps.
Materials and methods
Gelatin hydrogel sheets combined with bFGF
Gelatin hydrogel sheets with an isoelectric point of 5.0 were used, and rectangular sheets of 10 × 30 mm weighing 25 mg were prepared (n = 60 pieces) (Fig. 1a). The sheets were mixed in a glutaraldehyde (Wako Pure Chemical Industries, Osaka, Japan) solution with gelatin, and chemical cross-links were formed through the gelatin in polystyrene dishes, as described previously [8]. Human recombinant bFGF with an isoelectric point of 9.6 (Fiblast Spray 500; KAKEN Pharmaceutical Co., Tokyo, Japan) was obtained, and 50 or 100 μg of bFGF was dissolved with 250 μL of saline solution, dripped onto 12 gelatin hydrogel sheets each (12 sheets for 50 μg of bFGF and 12 sheets for 100 μg of bFGF), and incubated at 37 °C for 1 h. In addition, 250 μL of saline alone was used to prepare 12 gelatin hydrogel sheets.
a Gross appearance of gelatin hydrogel sheets. Preparation of rectangular gelatin hydrogel sheets (10 × 30 mm) impregnated ith bFGF (0, 50, and 100 μg) dissolved in 250 µL of saline. Scale bar: 10 mm. b Release of bFGF from gelatin hydrogel sheets. At different time intervals, the supernatant was removed, and the amount of bFGF released was determined. c Animals were divided into five groups (n = 12 animals/group). d Establishment of the murine dorsal skin flap model. (1) A murine dorsal skin flap (10 × 30 mm) with a cranial pedicle was designed. (2) The dorsal skin flaps were elevated beneath the panniculus carnosus. (3) A gelatin hydrogel sheet impregnated with bFGF (0, 50, and 100 μg) was inserted under the flap, or a bFGF solution was dripped under the flap. (4) Flaps were immediately sutured into the original position with 5-0 nylon. e Schematic illustration of the murine skin flap analysis method. Flap survival and necrotic areas were evaluated on day 7. Vascularization on the backside of a 7 × 7 mm area 3 mm from the skin flap base was investigated. In addition, a 2 × 2 mm section of flap tissue was collected from the distal site and used for histological assessments. f The time course of bFGF release from 100 μg of bFGF-impregnated gelatin hydrogel sheets (n = 5) in PBS with collagenase. The gelatin hydrogel sheet began to degrade in the collagenase solution, and bFGF was subsequently released. Data are presented as means ± standard error
bFGF release from bFGF-impregnated gelatin hydrogel sheets
To evaluate bFGF release from bFGF-impregnated gelatin hydrogel sheets, rectangular gelatin hydrogel sheets (10 × 12 mm) soaked in 100 μg of bFGF were incubated in phosphate-buffered saline (PBS) at 37 °C (n = 5). After 1 h, the PBS was replaced with PBS containing 10 µg/mL collagenase. At different time points, the supernatant was removed and replaced with the same volume of fresh PBS with 10 µg/mL collagenase, as described in a previous study [9] (Fig. 1b). The gelatin hydrogel sheets used in this study are widely used for the slow release of growth factors [7,8,9]. The amount of bFGF released was determined using a Quantikine Enzyme-linked Immunosorbent Assay (ELISA) Kit (R&D Systems, Minneapolis, MN, USA) in accordance with the manufacturer’s instructions.
Animal skin flap models
Sixty C57BL/6 male mice, 9 weeks of age (Shimizu Laboratory Supply Co., Ltd., Kyoto, Japan) with a mean weight of 33.8 g, were assigned to five experimental groups (n = 12 per group). Under general anesthesia by inhalation of 0.5 mg/kg body weight isoflurane (DS Pharma Animal Health Co., Ltd., Osaka, Japan), a dorsal skin flap of 10 × 30 mm was elevated beneath the panniculus carnosus. In the control group (Group I), the flap was elevated without inserting a hydrogel sheet. In Group II, a gelatin sheet impregnated with 250 µL of saline was inserted under the flap. In Group III, 100 µg (250 mL) of bFGF was sprayed under the flap without inserting a hydrogel sheet. Sheets impregnated with 50 and 100 μg of bFGF were inserted under the flap in Groups IV and V, respectively (Fig. 1c). Flaps were restored to their original positions (Fig. 1d) and sutured with nylon 5–0 (Bear Medic Co., Ltd., Tokyo Japan.) at 10 mm intervals at the flap margin. These procedures were performed under sterile conditions, and the animal study was conducted in accordance with the Guidelines for Animal Experimentation of Kansai Medical University and approved by the Animal Experimentation Committee of Kansai Medical University.
Evaluation of flap viability
Blood flow in a murine skin flap model is established on day 7 [10,11,12]. Accordingly, in this study, mice were euthanized by overdose inhalation of isoflurane gas 7 days after the surgery. The flaps were excised at the baseline and images of the surface and backside of the flaps were obtained using a digital camera (RICOH WG-5 GPS; RICOH IMAGING Co., Ltd., Tokyo, Japan) and imported to a computer (LaVie LZ750SSB; NEC Co., Ltd., Tokyo, Japan). The total flap survival areas were calculated by tracing the margins using Image J ver. 1.48 (National Institutes of Health, Bethesda, MD, USA). Angiogenesis on the backside of the flaps was assessed using KURABO Angiogenesis Image Analyzer ver. 2.0 (KURABO INDUSTRIES LTD., Osaka, Japan) by counting the converted pixels identified as blood vessels in each digital image. Angiogenesis was evaluated in 7 mm squares and 3 mm distal from the flap base, and joint angiogenesis and angiogenetic length were measured (Fig. 1e).
Histological assessments
A 2-mm square transverse segment was taken 10 mm distal from each flap base for fixation with 4% phosphate-buffered paraformaldehyde. Paraffin sections (5 μm thick) were then stained with hematoxylin and eosin (HE), and the flap thickness in the sections was analyzed using an NDP.view 2 Nanozoomer (Hamamatsu Photonics K.K., Hamamatsu, Japan). The thicknesses of the dermis, panniculus adiposus, and panniculus carnosus were measured and averaged at three randomly selected points in each HE-stained section. To identify changes in endothelial cell-lined vessels, the numbers and sizes of neovascular vessels were measured in all fields of anti-murine von Willebrand factor (vWF)-stained sections using a previously described method [9]. Slides were exposed to a rabbit polyclonal anti-murine vWF antibody (DakoCytomation, Carpinteria, CA, USA). All evaluations were carried out blindly by two of the authors (Kakudo and Lai).
Statistical analyses
Statistical analyses were performed using Excel (2013; Microsoft Corporation, Redmond, WA, USA). The results were analyzed by Student’s t tests. Values of p < 0.05 were considered significant.
Results
Amount of bFGF released per impregnated hydrogel sheet
The time course of the degradation of gelatin hydrogel sheets is shown in Fig. 1f. Gelatin hydrogel sheets began to degrade in the collagenase solution, subsequently releasing bFGF. A total of 13 h was required to release the total amount of bFGF impregnated in the gelatin hydrogel sheets. These findings indicate that the gelatin hydrogel sheets gradually released bFGF in a sustained manner according to the course of biodegradation.
Effect of gelatin hydrogel sheets impregnated with bFGF in on flap survival
Figure 2a shows the gross appearance of the flaps 7 days after the surgery. The flaps in Groups IV and V were markedly thickened and swollen. The average surviving area in Group IV (195.17 ± 41.74 mm2) was 1.35 times larger than that in group I (144.22 ± 31.07 mm2, p = 0.002896) and 1.33 times larger than that in Group II (147.17 ± 48.79 mm2, p = 0.001712). In addition, the average surviving area in Group V (177.88 ± 37.89 mm2) was also larger than those in Group I (144.22 ± 31.07 mm2, p = 0.02689) and Group II (147.17 ± 48.79 mm2, p = 0.09982). In a comparison of survival areas, flaps of the bFGF-impregnated gel groups (Group IV and Group V) were significantly larger than those of the groups with elevated flaps only (without a hydrogel sheet) (Group I), flaps treated with saline impregnated gel (Group II), and flaps sprayed with bFGF alone (without a hydrogel sheet) (Group III). The average flap survival rates for Groups I to V were 48.1%, 49.0%, 45.4%, 65.0%, and 59.2%, respectively (Fig. 2b).
a Gross appearance of the flaps in each group at 7 days after surgery. b Assessment of the flap survival area at 7 days after the surgery. The flap survival area was significantly larger in groups IV and V than in the other groups. c Gross appearance of angiogenesis on the backside of the flaps in each group at 7 days after the surgery. d The angiogenic length score was significantly higher in group IV than in group II. e The joint angiogenesis score was significantly higher in group IV than in groups II and III. Data are presented as the means ± standard error. *p < 0.05
Assessment of angiogenesis on the flap backside
On gross examination of the angiogenesis of the backside of flaps, Group IV showed significantly more vasodilatation and expansion of the vascular plexus than that in Groups I and II (Fig. 2c). In a quantitative analysis of the backside, Groups IV and II showed significant differences in angiogenic length (4098 ± 2313 pixels vs. 2214 ± 2105 pixels, p = 0.0488) (Fig. 2d) and joint angiogenesis (980.9 ± 582.8 pixels vs. 465.5 ± 491 pixels, p = 0.0291) (Fig. 2e). The average angiogenic length on the flap backside in Group IV was 1.85 times larger than that in Group II.
Histological assessment of the thickness of the dermis, panniculus adiposus, and panniculus carnosus
HE staining results for all groups are shown in Fig. 3a. The thickness of the dermis in all groups was roughly equal (423.5 ± 38.2 µm, 408.1 ± 52.8 µm, 427.8 ± 47.1 µm, 414.1 ± 53.8 µm, 398.7 ± 68.9 µm) (Fig. 3b), while the panniculus adiposus was significantly thicker in Group IV (195.7 ± 46.7 µm) than in Groups I (111.1 ± 14.5 µm, p = 0.0000457) and II (195.7 ± 46.7 µm vs. 118.8 ± 36.9 µm, p = 0.000208) and in Group V (197.4 ± 60.7 µm) than in Groups I (111.1 ± 14.5 µm, p = 0.000445) and II (118.8 ± 36.9 µm, p = 0.00122) (Fig. 3c). In addition, the panniculus carnosus was significantly thicker in Group IV (144.5 ± 27.6 µm) than in Groups I (93.5 ± 8.91 µm, p = 0.0000385) and II (109.5 ± 18.9 µm, p = 0.0018) and in Group V (112.1 ± 20.4 µm) than in Group I (93.5 ± 8.91 µm, p = 0.0111) (Fig. 3d).
a Light photomicrograph of the flap in each group 7 days after the surgery Hematoxylin–eosin (HE) staining. Scale bar: 200 μm. b Assessment of the thickness of the dermis. There was no significant difference among the groups. c Assessment of the thickness of the panniculus adiposus in each group. Thicknesses were significantly greater in groups IV and V than in Groups I and II. d Assessment of the thickness of the panniculus carnosus in each group. The thickness was significantly greater in group IV than in groups I and II. Data are presented as the means ± standard error. *p < 0.05
Histological assessment of newly formed capillaries
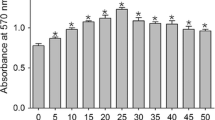
vWF staining results for all groups are shown in Fig. 4a. The number of vessels was significantly larger in Group IV (10.36 ± 3.06) than in Groups I (6.85 ± 1.61, p = 0.0026) and II (7.42 ± 3.61, p = 0.043) and in Group V (11.76 ± 3.47) than in Groups I (6.85 ± 1.61, p = 0.00041) and II (7.42 ± 3.61, p = 0.0066) (Fig. 4b). In addition, the areas of the vessels were significantly larger in Group IV (7765 ± 2987 µm2) than in Groups I (2916 ± 1299 µm2, p = 0.000117) and II (3650 ± 4540 µm2, p = 0.0251) and in Group V (4186 ± 1027 µm2) than in Group I (2916 ± 1299 µm2, p = 0.0148) (Fig. 4c).
a von Willebrand factor immunohistochemical staining of the flap in each group 7 days after the surgery. Scale bar: 250 μm. b Assessment of the number of vessels in each flap. The number of vessels in group IV was significantly larger than those in groups I and II, as was the number of vessels in group V. c Assessment of the area of vessels in each flap. The area of vessels in group IV was significantly larger than those in groups I and II as was the area of vessels in group V. Data are presented as means ± standard error. *p < 0.05
Discussion
Our results demonstrated that gelatin hydrogel sheets impregnated with bFGF improve the engraftment rate of murine skin flaps and increase the vascularization and thickness of the panniculus adiposus and panniculus carnosus. Covering a tissue defect with a local skin flap is a basic strategy in plastic and reconstructive surgery; however, necrosis of a distal portion of the skin flap often leads to clinical problems, re-operation, and elongation of the therapeutic period. To improve skin flap survival, various methods have been developed. For example, growth factor gene transfer [13, 14] and the administration of various drugs [15,16,17,18,19] experimentally improve skin flap survival. However, few procedures able to reliably exert such beneficial effects in clinical settings have been established.
bFGF is a heparin-binding growth factor that promotes the growth and migration of cultured vascular endothelial cells, protease formation, and lumen formation as well as vascularization [20, 21]. A human recombinant bFGF drug (Fiblast Spray 500; KAKEN Pharmaceutical Co.) for skin ulcers and bedsores is approved for clinical use in Japan, and its safety and efficacy are widely recognized. However, the half-life of bFGF in the body is < 1 h [22], and it is difficult to maintain an effective concentration at the target site. The sustained release of bFGF from biomaterials at the target site can resolve this issue.
Gelatin is chemically crosslinked in 5% (w/v) aqueous solution with various concentrations of glutaraldehyde at 4 °C to prepare hydrogels with different extents of crosslinking. Acidic gelatin with an isoelectric point of 5.0 is able to retain bioactive substances through electrostatic interactions [7]. To maintain a positive charge in acidic gelatin, it tends to stabilize with negatively charged proteins. Many growth factors are basic ionized proteins and can be easily impregnated in an acidic gelatin hydrogel. Since the degradation of the acidic gelatin hydrogel incorporating various growth factors results in the sustained release of bioactive substances, this material can behave as a DDS [7, 23]. Therefore, gelatin hydrogels are a versatile biodegradable material for medical uses, with demonstrated biosafety. Acidic gelatin hydrogels generally take the form of an injectable microsphere or a small disk sheet, and administration methods include local injection or intravascular infusion. Various growth factors have been incorporated into acidic gelatin hydrogels (e.g. bFGF and PRP) [8, 24]. However, the sustained release of bFGF from gelatin hydrogel sheets and consequent improvement of flap survival have not been reported.
It has been demonstrated that in vivo release profiles of bFGF from gelatin hydrogels were influenced by the degradability of the hydrogels and the resulting angiogenic activity of bFGF-incorporating gelatin hydrogels was modulated by the release profile [7]. Actually, an in vitro sustained-release experiment with gelatin hydrogels generally performed over time (12–48 h), was conducted as described by Matsui et al. [9]. Consistent with the previous results, incorporated bFGF was released along with the degradation of gelatin hydrogels. The in vivo results obtained with tissue specimens on day 7 showed absorption and degradation of the gelatin hydrogel sheet. The experiment of Matsui et al. also suggested that bFGF might be released along with the degradation of gelatin hydrogels both in vivo (7 days) and in vitro (12–35 h), promoting angiogenesis in vivo. The in vitro and in vivo results cannot be compared because of the different time courses. Currently, no suitable method is available to examine the in vivo absorption and bFGF release without inactivation, demanding the future development of novel experimental and evaluation methods. Thus, further investigation is needed on the appropriate profile of in vivo bFGF release.
It also has recently been reported that bFGF-impregnated hydrogel particles with a sustained controlled release promote angiogenesis in various tissues. For example, in ischemic limbs, a complex of gelatin microspheres and bFGF promotes angiogenesis and induces the development of functional collateral vessels via sustained release [25]. For bone augmentation, gelatin hydrogel microspheres enable the precise delivery of bFGF and induce bone augmentation around implants [26]. The combination of gelatin hydrogel, which is a feasible DDS for bFGF, with bFGF-2 leads to improved hard tissue healing and a reduced treatment time after surgery [27]. In humans, the sustained release of bFGF using a biodegradable gelatin hydrogel had therapeutic angiogenic effects and is safe for patients with critical limb ischemia [28]. In patients with severe Bell’s palsy, the efficacy of bFGF delivery has also been reported [29].
A previous study has shown that the controlled delivery of bFGF enhances the viability of ischemic skin flaps in rats [30]. In the skin flap model, however, almost all of the integral units of the gelatin hydrogel used as the DDS are handled as injectable microsphere particles administered via local injection or intravascular infusion. These conventional methods have various limitations, including complicated procedures, a high degree of invasiveness, and tissue damage, including potential negative effects on tissue viability and blood flow. Furthermore, the injection of microsphere particles might injure tissues and blood vessels, leading to low viability of flap tissue and low blood flow.
To overcome these deficits, a sheet-type gelatin hydrogel was developed. Platelet-derived growth factor BB-impregnated gelatin hydrogel sheets may promote tendon-to-bone healing after rotator cuff repair in rats [31]. Gelatin hydrogels are useful carrier sheets for the transplantation of cultivated corneal endothelial cells [32]. The controlled release of bFGF from a gelatin hydrogel sheet improves the structural and physiological properties of vein grafts in rats [33].
A cytokine-containing sheet-type gelatin hydrogel has not been applied to improve the viability of overlying skin flaps. In our murine skin flap model, angiogenesis was promoted by the sustained controlled release of bFGF, consequently increasing the skin flap thickness and flap survival area, as proven histologically. However, it is unclear why the results for Group V (100 µg of bFGF) were worse than those for Group IV (50 µg of bFGF). High concentrations of bFGF have been shown to inhibit angiogenesis [34]. An excessive concentration of bFGF is assumed to affect tissue invasion. The careful investigation of the treatment duration and dose, confirmation of the safety and efficacy in large animals, and confirmation of the efficacy in a randomized controlled study are necessary.
Conclusions
Our results indicated that a gelatin hydrogel sheet impregnated with bFGF can improve the engraftment rate of skin flaps, promote vascularization, and increase the thickness of the panniculus adiposus and panniculus carnosus. The clinical application of sustained-release bFGF from a gelatin hydrogel sheet might help improve flap engraftment rates.
References
Uhl E, Barker JH, Bondar I, Galla TJ, Lehr HA, et al. Improvement of skin flap perfusion by subdermal injection of recombinant human basic fibroblast growth factor. Ann Plast Surg. 1994;32:361–5.
Kusumoto K, Isshiki N, Suzuki S, Ohtsuka M, Nose K. Increase in length of experimental skin flaps that survive with dibutyryl-cyclic-amp. Scand J Plast Reconstr Surg Hand Surg. 1995;29:111–6.
Gospodarowicz D, Ferrara N, Schweigerer L, Neufeld G. Structural characterization and biological functions of fibroblast growth factor. Endocr Rev. 1987;8:95–114.
Powers CJ, McLeskey SW, Wellstein A. Fibroblast growth factors, their receptors and signaling. Endocr Relat Cancer. 2000;7:165–97.
Kakudo N, Shimotsuma A, Kusumoto K. Fibroblast growth factor-2 stimulates adipogenic differentiation of human adipose-derived stem cells. Biochem Biophys Res Commun. 2007;359:239–44.
Kakudo N, Morimoto N, Ogawa T, Taketani S, Kusumoto K. FGF-2 combined with bilayer artificial dermis composed of collagen matrix prompts generation of fat pad in subcutis of mice. Med Mol Morphol. 2018;52:73–81.
Tabata Y, Nagano A, Ikada Y. Biodegradation of hydrogel carrier incorporating fibroblast growth factor. Tissue Eng. 1999;5:127–38.
Notodihardjo PV, Morimoto N, Kakudo N, Matsui M, Sakamoto M, et al. Gelatin hydrogel impregnated with platelet-rich plasma releasate promotes angiogenesis and wound healing in murine model. J Artif Organs. 2015;18:64–71.
Matsui M, Tabata Y. Enhanced angiogenesis by multiple release of platelet-rich plasma contents and basic fibroblast growth factor from gelatin hydrogels. Acta Biomater. 2012;8:1792–801.
Lu F, Mizuno H, Uysal CA, Cai XB, Ogawa R, et al. Improved viability of random pattern skin flaps through the use of adipose-derived stem cells. Plast Reconstr Surg. 2008;121:50–8.
Akimoto M, Takeda A, Matsushita O, Inoue J, Sakamoto K, et al. Effects of CBVEGF-A injection in rat flap models for improved survival. Plast Reconstr Surg. 2013;131:717–25.
Sheng L, Yang M, Li H, Du Z, Yang Y, et al. Transplantation of adipose stromal cells promotes neovascularization of random skin flaps. Tohoku J Exp Med. 2011;224:229–34.
Fujihara Y, Koyama H, Nishiyama N, Eguchi T, Takato T. Gene transfer of bFGF to recipient bed improves survival of ischemic skin flap. Br J Plast Surg. 2005;58:511–7.
Zacchigna S, Papa G, Antonini A, Novati F, Moimas S, et al. Improved survival of ischemic cutaneous and musculocutaneous flaps after vascular endothelial growth factor gene transfer using adeno-associated virus vectors. Am J Pathol. 2005;167:981–91.
Toutain CE, Brouchet L, Raymond-Letron I, Vicendo P, Berges H, et al. Prevention of skin flap necrosis by estradiol involves reperfusion of a protected vascular network. Circ Res. 2009;104:245–54.
Shalom A, Friedman T, Westreich M. The effect of postoperative aspirin on random pattern flaps in rats. Am Surg. 2007;73:1126–8.
Emery FM, Kodey TR, Bomberger RA, McGregor DB. The effect of nifedipine on skin-flap survival. Plast Reconstr Surg. 1990;85:61–3.
Iinuma T, Sawada Y. Topical application of capsaicin and flap survival. Br J Plast Surg. 1996;49:319–20.
Huemer GM, Wechselberger G, Otto-Schoeller A, Gurunluoglu R, Piza-Katzer H, et al. Improved dorsal random-pattern skin flap survival in rats with a topically applied combination of nonivamide and nicoboxil. Plast Reconstr Surg. 2003;111:1207–11.
Folkman J, Klagsbrun M. Angiogenic factors. Science. 1987;235:442–7.
Sun XT, Ding YT, Yan XG, Wu LY, Li Q, et al. Angiogenic synergistic effect of basic fibroblast growth factor and vascular endothelial growth factor in an in vitro quantitative microcarrier-based three-dimensional fibrin angiogenesis system. World J Gastroenterol. 2004;10:2524–8.
Edelman ER, Nugent MA, Karnovsky MJ. Perivascular and intravenous administration of basic fibroblast growth factor: vascular and solid organ deposition. Proc Natl Acad Sci USA. 1993;90:1513–7.
Yamamoto M, Ikada Y, Tabata Y. Controlled release of growth factors based on biodegradation of gelatin hydrogel. J Biomater Sci Polym Ed. 2001;12:77–88.
Kurita J, Miyamoto M, Ishii Y, Aoyama J, Takagi G, et al. Enhanced vascularization by controlled release of platelet-rich plasma impregnated in biodegradable gelatin hydrogel. Ann Thorac Surg. 2011;92:837–44.
Hosaka A, Koyama H, Kushibiki T, Tabata Y, Nishiyama N, et al. Gelatin hydrogel microspheres enable pinpoint delivery of basic fibroblast growth factor for the development of functional collateral vessels. Circulation. 2004;110:3322–8.
Hayashi K, Kubo T, Doi K, Tabata Y, Akagawa Y. Development of new drug delivery system for implant bone augmentation using a basic fibroblast growth factor-gelatin hydrogel complex. Dent Mater J. 2007;26:170–7.
Kimura A, Kabasawa Y, Tabata Y, Aoki K, Ohya K, et al. Gelatin hydrogel as a carrier of recombinant human fibroblast growth factor-2 during rat mandibular distraction. J Oral Maxillofac Surg. 2014;72:2015–31.
Kumagai M, Marui A, Tabata Y, Takeda T, Yamamoto M, et al. Safety and efficacy of sustained release of basic fibroblast growth factor using gelatin hydrogel in patients with critical limb ischemia. Heart Vessels. 2016;31:713–21.
Hato N, Nota J, Komobuchi H, Teraoka M, Yamada H, et al. Facial nerve decompression surgery using bFGF-impregnated biodegradable gelatin hydrogel in patients with bell palsy. Otolaryngol Head Neck Surg. 2012;146:641–6.
Fujihara Y, Koyama H, Ohba M, Tabata Y, Fujihara H, et al. Controlled delivery of bFGF to recipient bed enhances the vascularization and viability of an ischemic skin flap. Wound Repair Regen. 2008;16:125–31.
Tokunaga T, Ide J, Arimura H, Nakamura T, Uehara Y, et al. Local application of gelatin hydrogel sheets impregnated with platelet-derived growth factor BB promotes tendon-to-bone healing after rotator cuff repair in rats. Arthroscopy. 2015;31:1482–91.
Watanabe R, Hayashi R, Kimura Y, Tanaka Y, Kageyama T, et al. A novel gelatin hydrogel carrier sheet for corneal endothelial transplantation. Tissue Eng Part A. 2011;17:2213–9.
Haraguchi T, Okada K, Tabata Y, Maniwa Y, Hayashi Y, et al. Controlled release of basic fibroblast growth factor from gelatin hydrogel sheet improves structural and physiological properties of vein graft in rat. Arterioscler Thromb Vasc Biol. 2007;27:548–55.
Okumura M, Okuda T, Nakamura T, Yajima M. Acceleration of wound healing in diabetic mice by basic fibroblast growth factor. Biol Pharm Bull. 1996;19:530–5.
Author information
Authors and Affiliations
Contributions
Conceived and designed the experiments: MH, NK, and KK. Performed the experiments: MH, NK, and FL. Analyzed data: NM and TH. Contributed reagents/materials/analysis tools: JJ, and YT. Wrote the paper: MH, NK and KK.
Corresponding author
Ethics declarations
Conflict of interest
The authors report no proprietary or commercial interest in any of the products mentioned or any of the concepts discussed in this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hihara, M., Kakudo, N., Morimoto, N. et al. Improved viability of murine skin flaps using a gelatin hydrogel sheet impregnated with bFGF. J Artif Organs 23, 348–357 (2020). https://doi.org/10.1007/s10047-020-01188-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10047-020-01188-7