Abstract
Cardiopulmonary bypass-associated acute kidney injury may appear postoperatively, but predictive factors are unclear. We investigated the potential of regional tissue oxygen saturation as a predictor of cardiopulmonary bypass-associated acute kidney injury. We analyzed the clinical data of 150 adult patients not on dialysis who underwent elective cardiac surgical procedures during January 2015–March 2017. Near-infrared spectroscopy was used to measure regional oxygen saturation. Sensors were placed on the patients’ forehead, abdomen, and thigh. The incidence of acute kidney injury was 2% at the end of surgery, 13% at 24 h, and 9% at 48 h, with the highest at 24 h after surgery. The multiple regression analysis revealed that the thigh regional oximetry during cardiopulmonary bypass, oxygen delivery index, and neutrophil count at the end of cardiopulmonary bypass and surgery were independent risk factors for acute kidney injury. The receiver-operating characteristic curve analysis suggested that a cutoff of regional oxygen saturation at the thigh of ≤ 67% was predictive of acute kidney injury within 24 h after surgery. In conclusion, the regional oxygen saturation at the thigh during cardiopulmonary bypass is a crucial marker to predict postoperative acute kidney injury in adults undergoing cardiac surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiopulmonary bypass-associated acute kidney injury (CPB-AKI) increases short- and long-term risks and is associated with prolonged hospital stay [1,2,3]. In recent years, perioperative renal protection during cardiopulmonary bypass (CPB) has assumed increasing importance [4, 5]. The pathophysiology of CPB-AKI is complicated and multifactorial, with risk factors known to include decreased renal perfusion, metabolic and neurohormonal activation, oxidative stress, activation of proinflammatory mediators leading to inflammation, and the presence of nephrotoxic substances [2, 6, 7]. CPB is always accompanied by a risk of ischemia–reperfusion injury, which is associated with blood dilution and low blood pressure, cardiac arrest, and reduced pulmonary blood flow, and is a major cause of CPB-AKI [6, 8, 9]. Monitoring tissue perfusion with near-infrared spectroscopy to assess regional oxygen saturation (rSO2) is reported to capture well the changes in oxygen supply and demand [10,11,12]. We investigated the potential of tissue rSO2, measured intraoperatively with near-infrared spectroscopy, as an early predictor of CPB-AKI.
Patients and methods
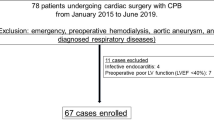
A retrospective study was performed on 150 consecutive cases of adult cardiac surgery from January 2015 to March 2017. Emergency operations, aortic procedures, and operations for patients on dialysis were excluded.
Regional oximetry using a near-infrared spectroscopy device, INVOS 5100 C (Medtronic, Minneapolis, MN, USA) was used to measure rSO2. Sensors were placed on the patients’ forehead, abdomen (at the level of the 12th thoracic vertebra), and the lateral side of the thigh during induction of anesthesia; rSO2 was measured from induction until the end of surgery, with data acquired every 30 s. The rSO2 data were calculated as an average of the values acquired at each detection point during CPB, with the average value during the first 5 min of induction of anesthesia used as the preoperative value. Furthermore, hematological examination was performed at the end of CPB and after entering ICU.
The oxygen delivery index (DO2i), as an indicator of the oxygen delivery amount, was evaluated per the following equation using cardiac output values.
AKI was determined according to the RIFLE classification by assessing the decline in estimated glomerular filtration rate (eGFR) [13].
The RIFLE classification is based on the serum creatinine and urine output determinants, and considers three severity classes of AKI (risk, injury, and failure), according to the variations in the serum creatinine and/or urine output, and two outcome classes (i.e., loss of kidney function and end-stage kidney disease) [14]. We investigated the association of various CPB factors, including rSO2, with the incidence and causes of postoperative AKI as indicated by changes in eGFR from preoperative values until 48 h after surgery. Univariate, logistic, and receiver-operating characteristic (ROC) curve analysis was used to assess the variables obtained at the time the postoperative AKI incidence was the highest to determine an association between CPB parameters, such as rSO2 and postoperative laboratory and clinical data.
Cardiopulmonary bypass procedure
For all cases, the CPB system comprised a centrifugal pump and a remote-controlled unit (HAS-2; Senko Medical, Tokyo, Japan), oxygenator, and reservoir (priming volume: 144 or 260 mL; Capiox-FX; Terumo, Tokyo, Japan). The extracorporeal circuit tubing was selected according to the patient’s body surface area, with a tubing priming volume of 650 mL for an area ≤ 1.66 m2 and 850 mL for an area > 1.66 m2. Blood gas management was performed with the alpha-stat strategy. During CPB, 300–400 U/kg heparin was used to prevent blood clotting, along with additional doses to attain and maintain an activated clotting time of > 480 s. The pump flow was adjusted to around 2.4 L/min/m2. The mean pressure during CPB was maintained at approximately 50–60 mmHg. The body temperature was maintained at 34 °C. Cardioplegic solution (10 mL/kg) was given every 30 min. After termination of CPB, heparin was neutralized by protamine sulfate until the activated coagulation time had normalized. Furthermore, the mixed venous oxygen saturation and forehead rSO2, which were routinely monitored using near-infrared spectroscopy during CPB, were maintained over 75% and 55%, respectively.
This study was approved by the Ethics Committee at the Kitasato Institute (Sagamihara, Kanagawa, Japan; August 22, 2019; B19-069).
Statistical analysis
In this study, statistical analysis was performed using JMP ver 11.0 (SAS Institute, Carey, NC). The continuous variables were presented as means ± standard deviations. We considered P < 0.05 as statistically significant.
Results
Table 1 presents perioperative data, including patients’ characteristics, and performed procedures, while Table 2 shows postoperative outcomes. In this study, the in-hospital mortality rate was 1.3%. The mean rSO2 values during CPB were 59.9% ± 7.8% at the forehead, 74.7% ± 8.6% at the abdomen, and 71.0% ± 6.5% at the thigh, respectively (Table 3), with the thigh rSO2 being significantly lower during CPB when compared with the preoperative value. An one-way ANOVA showed no difference in eGFR between the preoperative and 48-h postoperative values. The incidence of AKI by RIFLE classification was 2.7% (Risk 2%, Injury 0.7%) at the end of surgery, 12.7% (Risk 12.7%, Injury 0%) at 24 h after surgery, and 10.7% (risk 8.7%, injury 2%) at 48 h after surgery. AKI thus occurred most frequently at 24 h after surgery (Table 4). The difference in mean eGFR between the preoperative value and that 24 h after surgery was 1.3 mL/min. The univariate analysis revealed that patients’ age, duration of aortic cross-clamping, preoperative abdominal rSO2, thigh rSO2 during CPB, DO2i, neutrophil count at the end of CPB, lactate value at the end of CPB, and during the first 24 h after surgery significantly correlated with changes in eGFR from before to 24 h after surgery (Table 5). Multivariate regression analysis revealed that thigh rSO2 during CPB, DO2 index, and neutrophil count at the end of CPB were independent risk factors for a decrease in eGFR at 24 h after surgery (Table 6). ROC analysis indicated that a thigh rSO2 of 67% or lower was predictive of AKI developing within 24 h after surgery (Fig. 1).
Discussion
CPB is a necessary auxiliary procedure during cardiac surgery, but it can be a cause of postoperative multiple organ failure. Cardiac surgery with CPB correlates with multiple risk factors for AKI, such as low blood pressure, non-pulsatile flow, ischemia–reperfusion, and induction of inflammatory response mediators [6, 7]. A decrease in peripheral vascular resistance during CPB results in decreased effective renal plasma flow and thus decreased partial pressure of oxygen in the renal medulla [15, 16]. AKI is an important prognostic factor for postoperative recovery, such that early diagnosis and treatment of AKI is necessary for a good outcome. Elevated levels of postoperative serum creatinine and blood urea nitrogen are frequently used as a diagnostic marker depicting intraoperative glomerular injury. However, it only indicates injury that has already occurred [17]. Rather than waiting for that information after the fact, it is important to detect latent renal dysfunction to address it early in its course, which is why identifying early prognostic factors for AKI is important [18].
The use of near-infrared spectroscopy to measure cerebral oxygen saturation can easily and continuously detect hypoperfusion, ischemic changes, and oxygen supply and demand at the probe site. It is thus considered a useful noninvasive monitoring device to detect decreases in blood pressure, cannula malposition, malperfusion, or other conditions associated with CPB, allowing them to be addressed at an early stage [19,20,21]. Monitoring tissue rSO2 can detect changes in local oxygen supply and demand in various parts of the body. A decrease in local oxygen saturation, whether in the brain or elsewhere in the body, can thus be an early warning sign of ischemia, a risk factor for adverse events associated with CPB [22, 23]. Our study showed that, along with prolonged duration of CPB, DO2 index, and inflammatory response, peripheral tissue hypoperfusion detected by monitoring thigh rSO2 during cardiac surgery in adults was associated with postoperative renal dysfunction. This indicates that changes in oxygen supply and demand as reflected by changes in thigh rSO2 may be predictive of CPB-AKI. In this study, we performed abdominal and femoral monitoring because the oxygen supply-demand balance of abdominal organs with high blood flow, such as liver and kidney, can be measured at the abdomen (Th-12), whereas that in the peripheral tissues can be determined at the thigh. Choi et al. reported that the decline in abdominal rSO2 affixed just under the kidney with the echo guide correlated with AKI [24]. However, in this study, abdominal rSO2 did not correlate with AKI. The difference in the results could be because the sensor was not affixed just under the kidney without the echo guide, and the sensor at the right Th-12 could be slightly high for the assessment of the original renal blood flow. Hence, perhaps, the effective depth of field did not reach the organ because the effective depth of field of this model was ≤ 20 mm [25]. Conversely, the sensor at the thigh depicted the muscular layer perfusion status under the sensor without any effect of bones and the depth of field. The dysfunction of capillary microperfusion around the renal tubules, directly affects acute ischemic renal failure, and their epithelium cells slough off, and obstruct the lumen; thereby, inducing an increase in the hydrostatic pressure of the renal tubules and decline of glomerular filtration. On the other hand, the muscular layer of the lateral side of the thigh is capillary -rich; declined rSO2 of the thigh suggests capillary hypoperfusion and lack of O2 supply. Hence, when capillary hypoperfusion of the muscular layer of the thigh occurs, a similar phenomenon in the microperfusion of the capillary around the renal tubules located near the organ could occur. Thus, it is plausible that measuring the thigh rSO2 is convenience and sensitive. During CPB, when blood supply to peripheral tissues is poor, the microvasculature of surrounding organs is poorly perfused. In the kidney, a decrease in afferent arteriole blood flow can result in ischemia of downstream glomeruli.
Interestingly, our findings indeed suggest that thigh rSO2 values during CPB reflects not only poor peripheral tissue perfusion and hypoxia right underneath the probe but may also indicate microvascular ischemia in surrounding organs, notably the kidney. Renucci et al. reported a cutoff value of DO2 of 272 ml/min/m2 to be associated with CPB-AKI [26]; in this study, the average value exceeded this value, but there were also cases in which it did not exceed. When a reduction in peripheral rSO2 is indicated, an increase in DO2 by blood transfusion could be effective if the target blood pressure has been obtained. Alternatively, increasing peripheral rSO2 by decreasing the peripheral vascular resistance could be effective if the target DO2 has been reached. Furthermore, when the thigh rSO2 value decreased during rewarming, vasodilators were used to decrease the vascular resistance, and, subsequently, the pump flow and DO2 were increased. Thus, the thigh rSO2 value was recovered.
Although there are other studies assessing oxygen supply vis-a-vis AKI, none have previously assessed peripheral tissue oxygen demand in relation to the incidence of CPB-AKI. This knowledge gap should be addressed, which the current study has done. We have demonstrated an easy intraoperative method of assessing peripheral oxygen supply that appears to reflect concurrent renal perfusion. It is to be hoped that continuous monitoring of changes in tissue oxygen demand may allow prompt interventions to decrease the risk of CPB-AKI.
This study has the following limitations. One is that the data analysis was performed on a small sample from a single center. Therefore, our results may be specific to our study population. Similar studies in other institutions would be helpful in establishing more generalizable standards for such evaluations. To this end, further investigation is needed. Ours was a retrospective study. A prospective study investigating peripheral tissue rSO2 values could further confirm our findings and perhaps demonstrate useful interventions based on this monitoring method. Hemolysis can also cause renal dysfunction during CPB, but we did not assess this factor in our investigation. In a future study, we will consider the impact of hemolysis as an independent risk factor for CPB-AKI.
Conclusion
We found that the mean value of peripheral tissue rSO2 measured at the thigh during cardiac surgery in adults is an important marker to predict postoperative AKI. Further investigation is required to clarify the risk of AKI after CPB in cardiac surgery.
References
Josephs SA, Thakar CV. Perioperative risk assessment, prevention, and treatment of acute kidney injury. Int Anesthesiol Clin. 2009;47:89–105.
Rosner MH, Okusa MD. Acute kidney injury associated with cardiac surgery. Clin J Am Soc Nephrol. 2006;1:19–32.
Dasta JF, Kane-Gill SL, Durtschi AJ, Pathak DS, Kellum JA. Costs and outcomes of acute kidney injury (AKI) following cardiac surgery. Nephrol Dial Transp. 2008;23:1970–4.
Pickering JW, James MT, Palmer SC. Acute kidney injury and prognosis after cardiopulmonary bypass: a meta-analysis of cohort studies. Am J Kidney Dis. 2015;65:283–93.
Swaminathan M, Hudson CC, Phillips-Bute BG, Patel UD, Mathew JP, Newman MF, et al. Impact of early renal recovery on survival after cardiac surgery-associated acute kidney injury. Ann Thorac Surg. 2010;89:1098–104.
Hudson C, Hudson J, Swaminathan M, Shaw A, Stafford-Smith M, Patel UD. Emerging concepts in acute kidney injury following cardiac surgery. Semin Cardiothorac Vasc Anesth. 2008;12:320–30.
Haase M, Bellomo R, Haase-Fielitz A. Novel biomarkers, oxidative stress, and the role of labile iron toxicity in cardiopulmonary bypass-associated acute kidney injury. J Am Coll Cardiol. 2010;55(19):2024–33.
Karkouti K, Beattie WS, Wijeysundera DN, Rao V, Chan C, Dattilo KM, et al. Hemodilution during cardiopulmonary bypass is an independent risk factor for acute renal failure in adult cardiac surgery. J Thorac Cardiovasc Surg. 2005;129:391–400.
Slottosch I, Liakopoulos O, Kuhn E, Deppe A, Lopez-Pastorini A, Schwarz D, et al. Controlled lung reperfusion to reduce pulmonary ischaemia/reperfusion injury after cardiopulmonary bypass in a porcine model. Interact Cardiovasc Thorac Surg. 2014;19:962–70.
Murkin JM, Arango M. Near-infrared spectroscopy as an index of brain and tissue oxygenation. Br J Anaesth. 2009;103:i3–13.
Scheeren TW, Schober P, Schwarte LA. Monitoring tissue oxygenation by near infrared spectroscopy (NIRS): background and current applications. J Clin Monit Comput. 2012;26:279–87.
Steppan J, Hogue CW Jr. Cerebral and tissue oximetry. Best Pract Res Clin Anaesthesiol. 2014;28(4):429–39.
Uchino S, Bellomo R, Goldsmith D, Bates S, Ronco C. An assessment of the RIFLE criteria for acute renal failure in hospitalized patients. Crit Care Med. 2006;34:1913–7.
Lopes JA, Jorge S. The RIFLE and AKIN classifications for acute kidney injury: a critical and comprehensive review. Clin. Kidney J. 2013;6:8–14.
Lannemyr L, Bragadottir G, Krumbholz V, Redfors B, Sellgren J, Ricksten SE. effects of cardiopulmonary bypass on renal perfusion, filtration, and oxygenation in patients undergoing cardiac surgery. Anesthesiology. 2017;12:205–13.
Sgouralis I, Evans RG, Layton AT. renal medullary and urinary oxygen tension during cardiopulmonary bypass in the rat. Math Med Biol. 2017;34:313–33.
Haase M, Bellomo R, Devarajan P, Ma Q, Bennett MR, Möckel M, et al. Novel biomarkers early predict the severity of acute kidney injury after cardiac surgery in adults. Ann Thorac Surg. 2009;88:124–30.
Edelstein CL. Biomarkers of acute kidney injury. Adv Chronic Kidney Dis. 2008;15:222–34.
Denault A, Deschamps A, Murkin JM. a proposed algorithm for the intraoperative use of cerebral near-infrared spectroscopy. Semin Cardiothorac Vasc Anesth. 2007;11:274–81.
Colak Z, Borojevic M, Bogovic A, Ivancan V, Biocina B, Majeric-Kogler V. Influence of intraoperative cerebral oximetry monitoring on neurocognitive function after coronary artery bypass surgery; randomized, prospective study. Eur J Cardiothoracic Surg. 2015;47:447–54.
Subramanian B, Nyman C, Fritock M, Klinger RY, Sniecinski R, Roman P, et al. a multicenter pilot study assessing regional cerebral oxygen desaturation frequency during cardiopulmonary bypass and responsiveness to an intervention algorithm. Anesth Analg. 2016;122:1786–93.
Hagino I, Anttila V, Zurakowski D, Duebener LF, Lidov HG, Jonas RA. Tissue oxygenation index is a useful monitor of histologic and neurologic outcome after cardiopulmonary bypass in piglets. J Thorac Cardiovasc Surg. 2005;130:384–92.
IV Billings FT, Jiang Y, Shaw AD. Renal oxygen flux during cardiopulmonary bypass; tubular damage to preserve glomerular filtration – what’s a kidney to do? Anesthesiology. 2017;126:199–201.
Choi DK, Kim WJ, Chin JH, Lee EH, Don Hahm K, Yeon Sim J, et al. intraoperative renal regional oxygen desaturation can be a predictor for acute kidney injury after cardiac surgery. J Cardiothoracic Vasc Anesth. 2014;28:564–71.
Kobayashi K, Kitamura T, Kohira S, Torii S, Mishima T, Ohkubo H, et al. cerebral oximetry for cardiac surgery: a preoperative comparison of device characteristics and pitfalls in interpretation. J Artif Organs. 2018. https://doi.org/10.1007/s10047-018-1052-3.
de Somer F, Mulholland JW, Bryan MR, Aloisio T, Van Nooten GJ, Ranucci M. O2 delivery and CO2 production during cardiopulmonary bypass as determinants of acute kidney injury: time for a goal-directed perfusion management? Crit Care. 2011;15:R192.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sakaki, K., Kitamura, T., Kohira, S. et al. Regional thigh tissue oxygen saturation during cardiopulmonary bypass predicts acute kidney injury after cardiac surgery. J Artif Organs 23, 315–320 (2020). https://doi.org/10.1007/s10047-020-01175-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10047-020-01175-y