Abstract
Characteristics of pathological alterations in long-term peritoneal dialysis (PD) are thickening of submesothelial compact (SMC) zone, small-vessel vasculopathy, and loss of mesothelial cells. Bioincompatible PD fluid plays crucial roles in peritoneal injury. Encapsulating peritoneal sclerosis (EPS), a rare and serious complication, occurred in patients on long-term PD or frequent peritonitis episodes, and ~50 % of EPS developed after PD cessation. We hypothesized that PD-related peritoneal injury factors induced by bioincompatible PD fluid accumulated in the peritoneum and might induce EPS. We therefore examined the accumulation of advanced glycation end products (AGE) and beta 2-microglobulin (β2M) in peritoneum and evaluated the relationship between their accumulation, clinical parameters, and outcome after PD cessation. Forty-five parietal peritoneal specimens were obtained from 28 PD patients, 14 uremic patients, and three patients with normal kidney function. The peritoneal equilibration test was used for peritoneal function. AGE- and β2M-expressing areas were found in vascular walls, perivascular areas, and the deep layer of the SMC in short-term PD patients and extended over the entire SMC in long-term patients. Peritonitis and prolonged PD treatment aggravated peritoneal thickening and the proportion of AGE-expressing areas. The proportion of β2M-expressing areas was increased in long-term PD patients. Thickening of the SMC and the proportions of AGE- and β2M-expressing areas were not related to ascites or EPS after PD withdrawal. It appears that the increased proportion of AGE and β2M deposition induced by long-term exposure of PD fluid may be a marker of peritoneal injury.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Long-term peritoneal dialysis (PD) induces peritoneal functional changes defined as ultrafiltration failure and deterioration of solute transport [1, 2]. Morphological changes, such as detachment of mesothelial cells, fibrotic thickening of the submesothelial compact (SMC) zone, and vasculopathy, are associated with PD duration [3, 4]. Encapsulating peritoneal sclerosis (EPS) is a rare and serious complication. The longer PD is necessary and the more PD sessions required, the greater the risk of EPS development [5]. Approximately 50 % of EPS develops after PD discontinuation and transfer to hemodialysis or transplantation [5]. Honda and Oda [6] suggested that development of peritoneal injury after PD cessation is induced by superimposition of inflammatory stimuli as some type of “second hit.” We hypothesized that PD-related peritoneal injury factors induced by incompatible PD fluid that accumulates in the peritoneum might induce EPS.
Bioincompatible PD fluid (PDF), containing acid, glucose degradation products (GDPs) and having high osmolality, plays a central role in peritoneal injury during and after PD treatment, and a uremic condition may be accelerated by their presence. Extremely high concentrations of glucose in PDF may promote advanced glycation end products (AGE). Nakayama et al. [7] reported that AGE are present in the mesothelial layer, vascular walls, and connective tissues in the peritoneum and that AGE staining scores in semiquantitative assessment increased with PD duration. Therefore, quantitative analysis of accumulated AGE in the peritoneum may a worthy assessment of PD-related stimuli and may be associated with morphological and functional peritoneal alterations.
Beta 2-microglobulin (β2M) is one of the middle molecular uremic toxin substances, and its retention influences residual renal function and PDF bioincompatibility. β2M deposits are confirmed in synovial tissues, joint structures, and periarticular bones of dialysis-related amyloidosis (DRA) patients and lead to tissue injury [8]. These deposits appear to be involved in the pathogenesis of DRA by macrophage aggregation [9, 10]. Yokoyama et al. [11] suggested that β2M is useful as a screening maker for EPS onset and suspected that β2M and accumulation of middle molecular uremic substances may be related to the pathophysiology of EPS. However, there was a poor correlation between 2M concentration in serum and fibril load in osteoarticular tissues in long-term dialysis patients. Increased β2M concentration in the serum of patients on dialysis causes deposition of β2M in high-affinity space [12]. We previously reported that decorin, a predominant proteoglycan (PG) in normal human peritoneum, disappeared during PD treatment, and versican and hyaluronan were presented in the thickened SMC [13]. As some glycosaminoglycans (GAGs) and PGs could enhance the deposition of β2M-related amyloid fibril and possibly by binding directly to the surface of the fibrils and stabilizing the conformation of β2M in the fibrils [14], alterations in PG may contribute to deposition of degraded β2M and development of tissue injury in the peritoneum, such as DRA.
The relationship between AGE and β2M accumulation and functional and morphological peritoneal injury in PD patients remains unclear. In particular, there are few observations regarding the impact of such accumulation in long-term PD patients. We proposed quantitative assessment of AGE and β2M accumulation, evaluated their distribution, and examined correlations between AGE and β2M deposition and peritoneal function and clinical outcomes after PD cessation.
Materials and methods
Patients
Peritoneal specimens were obtained from 28 PD and 14 uremic patients and three patients without chronic kidney disease (CKD). All PD patients provided informed consent to participate in this study. In uremic patients and non-CKD patients, family members gave their consent in writing. The Ethics Committee of Juntendo University Faculty of Medicine approved this study, including evaluation of peritoneal morphology and peritoneal function. Intractable, noninfectious ascites, which could not be corrected by fluid control and administration of antibiotics, was defined as pre-EPS and treated with steroids according to the previous report [15]. EPS was diagnosed by clinical symptoms such as abdominal pain, nausea, vomiting, and macroscopic findings in laparoscopy.
Characteristics of patients
Three non-CKD patients had cancer of the oral cavity, uterus, and esophagus, respectively. Two PD patients had diabetic nephropathy; no diabetic nephropathy was seen in uremic patients. Reasons for withdrawal of PD treatment were 13 long-term PD, nine cases of uremia caused by underdialysis, three cases of peritonitis, two cases of ultrafiltration failure, and one notes simply as “other reason.” Non-CKD patients and uremic patients had no peritoneal diseases. We obtained peritoneal specimens and performed the peritoneal equilibration test [16] after overall improvement of peritonitis clinically and serologically. Total dialysate glucose during PD treatment was calculated by referring to the clinical chart and delivery records.Patient characteristics are presented in Table 1.
Peritoneal biopsy
Specimens were collected at the Juntendo University Hospital (Tokyo, Japan) from 1988 to 2010 after obtaining informed consent and approval from the Ethics Committee. Anteroabdominal parietal peritoneal specimens were obtained on the opposite side of PD catheter insertion when removing the PD catheter under laparoscopy in patients with no episodes of infectious peritonitis for 6 months prior to the examination. Peritoneal parietal specimens were also obtained from 14 uremic patients and three non-CKD patients on autopsy. Specimens were fixed in 10 % neutral formalin, embedded in paraffin, and stained with hematoxylin and eosin (H&E).
Histological analysis
Measurement of peritoneal thickness and SMC area
Thickness of the SMC was defined as the distance between the basal border of the mesothelial cell surface and upper border of adipose tissues. We randomly selected ten points in each of five fields in the section (50 points per patient) by ×200 magnification, and we measured SMC thickness using KS400, Universal Image Analysis Software (Carl Zeiss, Oberkocken, Germany). To calculate the area element, an outline of the SMC zone was traced in each specimen, avoiding artifacts such as compression or rupture. Using the assumption that the area approximated a square, each area was divided by its width using Imaging System KS400.
Immunohistological staining
-
1.
Diaminobenzidine (DAB) and fluorescent staining using anti-AGE and β2M
Peritoneal sections of 4 μm were processed for immunohistochemical staining with diaminobenzidine (DAB) before fluorescent staining. Monoclonal mouse anti-human AGE antibody, 6D12 (Trans Genic Inc, Kobe, Japan), carboxymethyl lysine protein adduct [17], was used to determine AGE deposition in peritoneal tissues. Polyclonal rabbit anti-human β2M, code no. A 0072 (DAKO Cytomation, Glostrup, Denmark) was used for determining human β2M [18]. These antibodies were also used in double staining. Sections of peritoneal specimens were deparaffinized by xylene and dehydrated by ethanol. Following blockade of endogenous peroxidase using 0.3 % hydrogen peroxide (H2O2) in methanol, sections were activated by citric acid in the microwave oven for 12 min. After cooling the sections at room temperature, 10 % nonimmune horse serum was used for blocking nonspecific binding sites. Sections were incubated with each antibody at 4 °C overnight. Anti-AGE and anti-β2M antibodies were diluted to 1:100 and 1:600, respectively, with 10 % nonimmune horse serum. In immunohistochemical staining with DAB, following addition of the biotin-labeled horse anti-mouse immunoglobulin G (IgG) secondary antibody, sections were treated with avidin–biotin–peroxidase complex (Vector Laboratories, Burlingame, CA, USA). Finally, sections were treated with DAB and H2O2 (DAKO Cytomation) to obtain a color reaction. Sections were counterstained with Mayer’s hematoxylin, and the primary antibody was not applied to the sections as a negative control. For double immunofluorescence, sections were washed with phosphate-buffered saline (PBS) after incubation of primary antibody and mounted with secondary antibody at room temperature for 30 min. Anti-mouse fluorescein isothiocyanate (FITC) antibody, anti-goat FITC antibody, and anti-rabbit tetramethyl rhodamine isothiocyanate (TRITC) antibody were used as secondary antibodies of AGE or β2M. Secondary antibodies were diluted to 1:200 with 10 % nonimmune horse serum.
-
2.
Quantitative analysis of AGE- and β2M-expressing areas
Anti-AGE- and anti-β2M-expressing areas in the SMC were measured by counting pixels with constant brightness using Image-Pro® for Image processing, enhancement, and analysis software (MediaCybernetics, Inc. Bethesda, MD, USA). To calculated the proportion of expressing area, we divided the AGE- or β2M-expressing areas by the entire SMC area. The proportion of the expressing area is shown in percentile.
Clinical assessment of the peritoneal equilibration test
Twenty-eight PD patients were classified into two groups: i.e., low-transport and high-transport patients. Peritoneal equilibration test was carried out using dialysate containing 2.5 % glucose according to the previous report [16]. Samples of dialysate and serum were refrigerated at −80 °C until measurement. Peritoneal equilibration test was performed within the 6 months prior to PD catheter removal. β2M in dialysate and serum was measured by the latex agglutination turbidimetric immunoassay method (SRL, Inc, Tokyo, Japan). Interleukin 6 (IL-6) was measured by chemiluminescent enzyme immunoassay method (SRL, Inc).
Statistical analysis
Nonparametric comparison was performed by the Mann–Whitney U test to estimate statistical significance between groups. The Kruskal–Wallis test was performed as a post hoc test, or the Dunnett method with Bonferroni correction was performed when we confirmed significant differences between groups. We also examined statistical significance using stepwise regression analysis. Data are expressed as means ± standard deviations (SD); p < 0.05 was considered significant. These statistical analyses were performed with StatView 5.0 software (Abacus Concepts, Piscataway, NJ, USA).
Results
Localization of AGE in SMC and β2M depositions
AGE deposition in short-term PD patients was found in the perivascular areas or in the deep layer of the SMC (Fig. 1a, b). The deposits were observed in the entire or the deep layer of the SMC in long-term PD patients (Fig. 1c). Patchy β2M deposition in SMC was found in short-term PD patients (Fig. 1d); depositions were present in perivascular or deep layer of SMC (Fig. 1e, f). Deposits in long-term PD patients extended over entire or the deep layer of the SMC (Fig. 1g).
Localization of advanced glycation end products (AGE) and beta 2-microglobulin (β2M) deposition in the peritoneum. AGE expression was present in the deep layer of the submesothelial compact (SMC) zone (a ×100) and in the periarteriolar area only in short-term peritoneal dialysis (PD) patients (c ×400). In long-term PD patients, AGE expression was observed in the entire layer of the SMC (c ×100). β2M deposits were present in the deep layer of the SMC in short-term PD patients (d ×100, f ×400) and in vascular walls (e ×400). β2M deposition was observed in the entire layer of the SMC in long-term PD patients (g ×400)
Quantitative analysis of AGE and β2M depositions in peritoneum
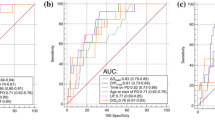
SMC thickness and the proportions of AGE- and β2M-expressing areas in PD patients were significantly higher compared with those in non-CKD and uremic patients (Fig. 2a–c). Long-term PD accelerated SMC thickening and accumulation of AGE- and β2M-expressing areas (Fig. 2d–f). Participants were divided into four groups according to PD duration and peritonitis episodes (Table 2). Patients who had >5 years on PD and episodes of peritonitis exhibited SMC thickening and a higher proportion of AGE- and β2M-expressing areas compared with the other groups (Table 2). There were no significant differences in morphological alterations corrected by PD duration between patients receiving acidic PD fluid and and those receiving neutral PD fluid (data not shown).
Quantitative analysis of advanced glycation end products (AGE) and beta 2-microglobulin (β2M) deposition in the peritoneum Thickness of submesothelial compact (SMC) zone and proportion of AGE- and β2M-expression areas in peritoneal dialysis (PD) patients was significantly increased compared with patients without chronic kidney disease (non-CKD) and those with uremia (a–c). Thickness of SMC and proportions of AGE- and β2M-expression areas in long-term PD patients were significantly higher than in short-term PD patients (d–f)
Colocalization of AGE and β2M expression in SMC
AGE and β2M expression was observed in mesothelial cells in short-term PD patients (Fig. 3a–c). AGE (in green) and β2M (in red) deposits were scattered over the entire SMC and mutually overlapped (in yellow) in long-term PD patients (Fig. 3d–f). AGE distribution was different from that of β2M in the interstitium, and the double-positive area (in yellow) was in the shallow submesothelia. Colocalization of AGE andβ2M was found in mesothelial cells covering the peritoneal surface in patients in the early stage of PD.
Colocalization of advanced glycation end products (AGE) and beta 2-microglobulin (β2M) expression in the peritoneum. In long-term peritoneal dialysis (PD) patients, AGE [a; anti-mouse fluorescein isothiocyanate (FITC) antibody] and β2M(b; rhodamine) expression was observed over the entire thickened submesothelial compact (SMC) zone. β2M expression partially overlapped the AGE-expressing area (c merge, white arrows). In long-term PD patients, both AGE (d; FITC) and β2M (e; rhodamine) expression were scattered over the entire SMC. However, β2M expression partially overlapped the AGE-expressing area (f merge, white arrows)
Relationship between clinical outcomes and parameters
After withdrawal of PD, duration of PD with episodes of ascites was significantly longer than that in patients without ascites (131.0 ± 34.7 vs no 154.6 ± 28.1 months, respectively; p < 0.0001). However, the amount of dialysate glucose and IL-6 and β2M levels in dialysate were not significantly different between patients with and without ascites. Morphological alterations, i.e., SMC thickening, proportion of AGE- and β2M-expressing areas, were not independent relative factors contributing to ascites. PD duration in patients complicated with EPS was significantly higher than that in those without EPS (153.6 ± 37.2 vs 69.6 ± 36.4 months, respectively; p < 0.0001). Morphological changes, SMC thickness, and proportion of AGE and β2M deposition areas were not independent contributing factors in EPS development after PD withdrawal. IL-6 and β2M levels in dialysate were not significantly different between patients with and without EPS (data not shown).
Discussion
Morphological peritoneal changes in PD patients are defined as mesothelial denudation, interstitial fibrosis, and vasculopathy in small vessels [1]. In quantitative assessment of peritoneal fibrosis and vasculopathy, Williams et al. [4] and Shimaoka et al. [19] reported a positive correlation between PD duration and SMC thickness. In our study, both PD duration and incidence of peritonitis accelerated morphologic alterations in the peritoneum. Most EPS developed after PD withdrawal. We hypothesize the quantitative alterations in the peritoneum may contribute to the development of peritoneal injury and EPS after discontinuation of bioincompatible PDF stimuli. Clinical course of dialysis-related amyloidosis, such as carpal tunnel syndrome (CTS), is quite similar to that of EPS, as it occurs in long-term dialysis patients; also, the second-hit phenomenon plays a role in CTS development [12].
This study showed that both the proportions of AGE and β2M deposition in the thicken peritoneum were increased in long-term PD patients. Depositions in perivascular areas and the deep SMC layer were found in short-term PD patients and extended over the entire peritoneal interstitium with PD duration. Peritonitis accelerated AGE deposition in PD patients and was partially colocalized with that of β2M. Accurately determining quantitative assessment for the double-positive area of AGE and β2M expression was a study limitation because it is difficult to detect and measure the double-positive area using the enzyme antibody technique.
In relation to quantitative peritoneal changes, long-term contact with glucose-based PD dialysate promotes accumulation of AGE in the peritoneum [20, 21], which alters peritoneal vasculatures and induces interstitial fibrosis [22]. Nakayama et al. [7] noted that AGE were present in the mesothelial layer, vascular walls, and connective tissues. Park et al. [23] reported that peritoneal AGE accumulation and peritoneal permeability in PD patients were higher than in uremic patients, noting that peritoneal accumulation of AGE increased with increased time on PD and number of peritonitis episodes.
AGE contribute to receptor-independent alteration of the extracellular matrix (ECM) structure by nonenzymatic glycation and formation of protein cross-links [24]. The other mechanism of tissue alteration by AGE in diabetic patients is its interaction with the receptor for AGE (RAGE). In this study, RAGE expression partly overlapped with AGE deposits. The study by Bucciarelli et al. [25], using homozygous RAGE null (knock-out) mice, reported that RAGE accelerated AGE formation in a hyperglycemic environment. Interaction of AGE with RAGE induces transforming growth factor beta (TGF-β) production, a pivotal factor in the process of epithelial to mesenchymal transition (EMT), with the acquisition of myofibroblast characteristics [26]. Among inflammatory cytokines, bacterial peritonitis has been associated with marked elevation of IL-1, IL-6, and TGF-β levels in dialysate [27].
PD duration might be closely related to the accumulation of β2M, but the incidence of peritonitis was not correlated with the density of β2M deposition. These results suggest that deposition of β2M in the peritoneum was not related to β2M serum levels but to long-term contact with β2M. β2M amyloidosis causes CTS in DRA patients. The incidence of CTS is associated with not only PD duration but also plasma β2M levels [8]. That report supports our opinion concerning the above-mentioned factors. Immunohistochemical staining revealed that β2M deposits overlapped AGE deposits to a wide extent in this study. Naiki et al. [28] suggested that specific molecules, such as apolipoprotein E (ApoE), GAGs, and PGs, affect formation and deposition of β2M-related amyloid fibrils. We reported that the composition of PGs in the peritoneum was altered in PD patients and a conversion from short-chain decorin to long-chain versican [13]. Based on the alteration of constituent collagens and PG in the thickened SMC, β2M deposition might be accelerated in long-term PD. AGE-modified β2M causes tissue injury by increasing TNF-α and IL-1β secretion from macrophages [29]. It is still unclear whether or not β2M deposited in the peritoneum is AGE modified and has a pathogenic role in the progression of peritoneal injury after PD discontinuation.
In this study, the proportions of AGE- andβ2M-expressing areas and SMC thickening were higher in patients with ascites or EPS. As there are a number of inadequacies in this study, it is impossible to assess the hazard ratio of EPS and ascites for the proportions of AGE and β2M depositions. The relationship between clinical outcomes and further morphological assessment should be examined over the long term in a large number of PD patients. AGE and β2M are characteristic morphological alterations contributing to peritoneal damage induced by PD fluid and peritonitis in PD patients.
References
Di Paolo N, Sacchi G, De Mia M, et al. Morphology of the peritoneal membrane during continuous ambulatory peritoneal dialysis. Nephron. 1986;44:204–11.
Gotloib L, Shostak A. Ultrastructural morphology of the peritoneum: new findings and speculations on transfer of solutes and water during peritoneal dialysis. Perit Dial Bull. 1987;7:119–29.
Honda K, Nitta K, Horita S, Yumura W, Nihei H. Morphological changes in the peritoneal vasculature of patients on CAPD with ultrafiltration failure. Nephron. 1996;72:171–6.
Williams JD, Craig KJ, Topley N, et al. Peritoneal Biopsy Study Group: morphologic changes in the peritoneal membrane of patients with renal disease. J Am Soc Nephrol. 2002;13:470–9.
Kawanishi H, Kawaguchi Y, Fukui H, et al. Encapsulating peritoneal sclerosis in Japan: a prospective, controlled, multicenter study. Am J Kidney Dis. 2004;44:729–37.
Honda K, Oda H. Pathology of encapsulating peritoneal sclerosis. Perit Dial Int. 2005;25:S19–29.
Nakayama M, Kawaguchi Y, Yamada K, et al. Immunohistochemical detection of advanced glycosylation end-products in the peritoneum and its possible pathophysiological role in CAPD. Kidney Int. 1997;51:182–6.
Ohashi K. Pathogenesis of beta2-microglobulin amyloidosis. Pathol Int. 2001;51:1–10.
Ohashi K, Hara M, Kawai R, et al. Cervical discs are most susceptible to beta2-microglobulin amyloid deposition in the vertebral column. Kidney Int. 1992;41:1646–52.
Argiles A, Mourad G, Kerr PG, et al. Cells surrounding haemodialysis-associated amyloid deposits are mainly macrophages. Nephrol Dial Transplant. 1994;9:662–7.
Yokoyama K, Yoshida H, Matsuo N, et al. Serum beta2 microglobulin (beta2MG) level is a potential predictor for encapsulating peritoneal sclerosis (EPS) in peritoneal dialysis patients. Clin Nephrol. 2008;69:121–6.
Eichner T, Radford SE. Understanding the complex mechanisms of β2-microglobulin amyloid assembly. FEBS J. 2011;278:3868–83.
Osada S, Hamada C, Shimaoka T, et al. Alterations in proteoglycan components and histopathology of the peritoneum in uraemic and peritoneal dialysis (PD) patients. Nephrol Dial Transplant. 2009;24:3504–12.
Yamaguchi I, Suda H, Tsuzuike N, et al. Glycosaminoglycan and proteoglycan inhibit the depolymerization of beta2-microglobulin amyloid fibrils in vitro. Kidney Int. 2003;64:1080–8.
Lo WK, Kawanishi H. Encapsulating peritoneal sclerosis–medical and surgical treatment. Perit Dial Int. 2009;29 Suppl 2:S211–4.
Twardowski ZJ, Nolph kDa, Khanna R, et al. Peritoneal equilibration test. Perit Dial Bull. 1987;7:138–47.
Ikeda K, Higashi T, Sano H, et al. N(epsilon)-(carboxymethyl) lysine protein adduct is a major immunological epitope in proteins modified with advanced glycation end products of the Maillard reaction. Biochemistry. 1996;35:8075–83.
Solé M, Muñoz-Gómez J, Campistol JM. Role of amyloid in dialysis-related arthropathies. A morphological analysis of 23 cases. Virchows Arch A Pathol Anat Histopathol. 1990;417:523–8.
Shimaoka T, Hamada C, Kaneko K, et al. Quantitative evaluation and assessment of peritoneal morphologic changes in peritoneal dialysis patients. Nephrol Dial Transplant. 2010;10:3379–85.
Nakamura S, Miyazaki S, Sasaki S, et al. Localization of imidazolone in the peritoneum of CAPD patients: a factor for a loss of ultrafiltration. Am J Kidney Dis. 2001;38:S107–10.
Miyata T, Horie K, Ueda Y, et al. Advanced glycation and lipid oxidation of the peritoneal membrane: respective roles of serum and peritoneal fluid reactive carbonyl compounds. Kidney Int. 2000;58:425–35.
Honda K, Hamada C, Nakayama M, Peritoneal Biopsy Study Group of the Japanese Society for Peritoneal Dialysis, et al. Impact of uremia, diabetes, and peritoneal dialysis itself on the pathogenesis of peritoneal sclerosis: a quantitative study of peritoneal membrane morphology. Clin J Am Soc Nephrol. 2008;3:720–8.
Park MS, Lee HA, Chu WS, et al. Peritoneal accumulation of AGE and peritoneal membrane permeability. Perit Dial Int. 2000;20:452–60.
Brownlee M, Vlassara H, Cerami M. Nonenzymatic glycosylation and the pathogenesis of diabetic complications. Ann Intern Med. 1984;101:527–37.
Bucciarelli LG, Ananthakrishnan R, Hwang YC, et al. RAGE and modulation of ischemic injury in the diabetic myocardium. Diabetes. 2008;57:1941–51.
De Vriese AS, Tilton RG, Mortier S, Lameire NH. Myofibroblast transdifferentiation of mesothelial cells is mediated by RAGE and contributes to peritoneal fibrosis in uraemia. Nephrol Dial Transplant. 2006;21:2549–55.
Lai KN, Lai KB, Lam CW, et al. Changes of cytokine profiles during peritonitis in patients on continuous ambulatory peritoneal dialysis. Am J Kidney Dis. 2000;35:644–52.
Naiki H, Yamamoto S, Hasegawa K, et al. Molecular interactions in the formation and deposition of beta2-microglobulin-related amyloid fibrils. Amyloid. 2005;12:15–25.
Miyata T, Inagi R, Iida Y, et al. Involvement of beta 2-microglobulin modified with advanced glycation end products in the pathogenesis of hemodialysis-associated amyloidosis. Induction of human monocyte chemotaxis and macrophage secretion of tumor necrosis factor-alpha and interleukin-1. J Clin Invest. 1994;93:521–8.
Conflict of interest
We have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Deceased: H. Nakamoto.
Rights and permissions
About this article
Cite this article
Nakamoto, H., Hamada, C., Shimaoka, T. et al. Accumulation of advanced glycation end products and beta 2-microglobulin in fibrotic thickening of the peritoneum in long-term peritoneal dialysis patients. J Artif Organs 17, 60–68 (2014). https://doi.org/10.1007/s10047-013-0741-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10047-013-0741-1