Abstract
With the widespread adoption of laparoscopic cholecystectomy and living-donor liver transplantation in recent years, complications involving the biliary system, stenosis in particular, are increasing. Various invasive and non-invasive techniques are now available for the treatment of biliary stenosis, but all are compromised by a high risk of recurrence and other problems. As a potential solution, our group has developed a bioabsorbable polymer (BAP) tube for implantation as a bypass graft. In the study reported here, we implanted this BAP tube and confirmed bile duct regeneration at the graft site after the tube had been degraded and absorbed into the body. We briefly describe our findings on extrahepatic biliary tissue regeneration, focusing on the possibility of its clinical application. This artificial bile duct may promote the development of novel treatments for biliary disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The current treatment for an extrahepatic bile duct affected by cancer or stenosis is to surgically remove the affected portion and anastomose the hilar bile duct to the small intestine. This approach is flawed, however, as the postoperative course is frequently complicated by retrograde infections via the intestine or by stenosis at the anastomosis, a condition requiring re-anastomosis [1–3]. In the worst case, bile stagnation due to impaired bile flow may require liver transplantation, even when the impairment is limited to the bile duct [4, 5]. And when liver transplantation is required, chronic rejection of the transplanted organ may result in bile duct stenosis leading to liver graft failure [6, 7]. This devastating outcome is possible even when the pathology is confined to the bile duct, and transplantation, or rather re-translation, may be required [6, 7]. If an artificial bile duct functionally identical to the natural organ is a feasible option, it can be used as a substitute for the pathologic bile duct. This approach would prevent the condition from aggravating to an extent requiring liver transplantation and would thereby effect a cure. Our group has been developing an artificial bile duct similar to the native duct in both function and morphology [8]. Although the literature dealing with the creation of an artificial bile duct is scarce [9–11], other researchers have succeeded in fabricating blood vessels [12, 13] and small intestines [14, 15] with biocompatible polymers.
This article briefly reviews our findings on extrahepatic biliary tissue regeneration with the possibility of its clinical application in mind. We also summarize earlier reports on various methods and materials devised to directly replace or regenerate bile ducts.
Extrahepatic bile duct regeneration in the artificial bile duct implantation model
Bile ducts with epithelial cells serve various functions, the most important of which is to carry bile out of the liver to the duodenum. Several investigators have attempted to develop substitute bile ducts to fulfill this function [11, 16], but among the substitutes tested so far, no epithelium has been able to grow on the lumen of the duct where the bile flows or on the anastomosis with the native duct. This limitation ultimately leads to obstruction and renders the substitutes unsuitable for long-term use. With help from rapidly evolving tissue-engineering techniques now available, our group has been working to regenerate bile ducts with a bioabsorbable polymer tube seeded with autologous bone marrow cells.
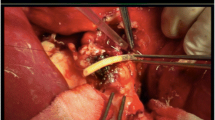
Briefly, bone marrow cells taken from swine sterna were seeded onto the interior of a tubular scaffold of a bioabsorbable polymer consisting of a copolymer of polylactic acid and polycaprolactone reinforced with polyglycolic acid fibers. Our target in selecting and fabricating the material was to construct a graft that would be completely absorbed into the body within 6–8 weeks (Fig. 1) [17]. Hybrid pigs served as the recipients of the artificial bile duct fabricated by tissue engineering. One hour after seeding the scaffold with bone marrow cells, the artificial duct was implanted into each of the pigs from which the bone marrow cells had been collected. The common bile duct was cut around the confluence with the cystic duct. The duodenal end of the common bile duct was ligated, while the hepatic end was anastomosed to the artificial bile duct. Next, the remaining end of the artificial bile duct was sutured to a 5-mm-diameter hole cut into the descending duodenum (Fig. 2). The graft site was recovered 6 months after implantation and observed macroscopically and histologically. All of the recipient pigs survived until sacrifice at 6 months after implantation. All had gained weight after the operation, with no evidence of jaundice. In terms of both histology and macroscopy, the morphology of the neo-bile duct was almost identical to that of the native common bile duct (Fig. 3), and the portion of the neo-bile duct that appeared to correspond to bile duct epithelial cells exhibited the same positive staining for CK19 exhibited by the native duct. The tubular artificial bile duct of the bioabsorbable polymer seeded with autologous bone marrow cells effectively functioned as a bile duct for 6 months. Over the short term following implantation, our tubular artificial bile duct, a substitute for the extrahepatic bile duct, carried bile to the duodenum without any leakage into the peritoneal cavity or any deformation of its tubular form. Once the artificial bile duct had been degraded and absorbed by the body, a new extrahepatic bile duct similar to the native duct developed at the graft site and functioned identically to that of a bile duct without any signs of stenosis.
Neo-bile duct 6 months after artificial bile duct implantation. a The neo-bile duct similar to the native bile duct formed at the graft site (arrow). b Histology of the graft site revealed a newly grown structure similar to that of the native duct, with cuboidal columnar epithelial cells in the lumen and accessory glandular structures in the adventitia
Histology of extrahepatic bile duct regeneration
In the early stages of our study we seeded the interior of the artificial duct with bone marrow cells prior to implantation. We had two reasons for doing so: first, to prevent bile leakage, as the scaffold we used was tubular in form and made of a porous spongy polymer; second, to investigate whether the bone marrow cells accelerate biliary epithelialization in the same manner seen in blood vessels [18, 19]. No bile leakage was observed from the neo-bile ducts arising from the scaffold unseeded by bone marrow cells in the early post-implantation phase. The rate and extent of biliary epithelialization were comparable in the scaffolding with and without the bone marrow cell seeding. On these grounds, we concluded that the seeding did not contribute to regeneration in this model. The observation that the polymer graft implanted without cell seeding gave rise to biliary epithelium demonstrated that migrating cells from outside the graft site formed biliary epithelium. The cell source for biliary epithelial regeneration was sought using this model. Findings at 7 weeks post-implantation showed that epithelial regeneration proceeded in a non-directed manner, starting neither from the hepatic nor duodenal part of the neo-bile duct. Rather, the graft site was uniformly re-epithelized at about the same rate. Re-epithelialization may result not from continuous division, proliferation, and differentiation of cells in the hepatic or duodenal part of the graft, but from the differentiation of stem/progenitor cells into biliary epithelial cells that uniformly adhere to the scaffold. Bone marrow cells are reported to migrate to an injured liver via peripheral circulation and to differentiate into hepatocytes at the injured site [20–22]. Speculating that the same process may take place in our model, we are currently investigating whether juvenile cells such as bone marrow cells adhere to the scaffold and differentiate into a regenerated bile duct. Smooth muscle is distributed throughout the subepithelium of the extrahepatic bile duct. In this study we used our bile duct implantation model to assess whether smooth muscle regenerates together with the epithelium. Cells positive for desmin, a distinct marker of regenerating smooth muscle, were detected in the subepithelium of the neo-bile duct at 7 weeks post-implantation, but the cells were scanty compared with those in the native extrahepatic bile duct. These results demonstrated the potential of this artificial bile duct as a scaffold for the regeneration of the bile duct epithelium and smooth muscle and, by extension, regeneration of the entire bile duct tissue.
Development of novel therapies for biliary disease
The outcomes of the current treatment strategies for biliary disease are not always favorable, which may reflect our poor knowledge of the biliary system. Much remains to be clarified; for example, with regard to balloon dilatation of the bile duct, the effects of the dilatation on epithelial cells, the adventitial connective tissue, and smooth muscle are largely unknown. No criterion has been established for defining the extent of dilatation, and the mechanism and process of bile duct healing and repair following severe injury during balloon dilatation remain unclear [23–25]. The disregard of bile duct regeneration in treatment modalities for biliary disease may be partly responsible for the unfavorable outcome [26, 27]. We propose that our method for inducing bile duct regeneration should be applied in the following ways as a treatment aid in clinical practice.
Development of a bioabsorbable biliary patch for the treatment of biliary stenosis
With the recent widespread use of laparoscopic cholecystectomy and living-donor liver transplantation, the incidence of complications involving the biliary system, stenosis in particular, has been increasing [28, 29]. Although various invasive and non-invasive techniques are now available for the treatment of biliary stenosis, recurrence and other problems limit their value and utility [30, 31]. Our group investigated whether a bioabsorbable polymer (BAP) patch could dilate a narrowed bile duct as a novel treatment for biliary stenosis [32]. The results were encouraging, with good bile duct dilation following the implantation of the BAP patch. The patch served as a scaffold for the regeneration of tissue similar to that of native duct tissue while allowing the bile to drain normally without leaving traces of foreign matter in the body. These advantages, together with the advantages of simple manipulation and enhanced safety, affirm the therapeutic potential of this patch for the treatment of humans with bile duct stenosis.
Development of a novel reflux-free bilioenteric anastomosis procedure
Surgery in the twenty-first century seeks to preserve the biological function to the utmost. The papilla of Vater is one example. Retrograde infection following the loss of papilla function causes narrowing and chronic inflammation at the anastomosis, conditions that have recently been reported to promote the development of carcinomas [33–37]. We sought to develop a reflux-free procedure for bilioenteric anastomosis endowed with a papilla-like function using an artificial bile duct (ABD) fashioned from a bioabsorbable polymer tube [38]. An ABD of 5 mm in diameter was implanted as a bypass graft in the extrahepatic bile duct of hybrid pigs. Anti-reflux function was created at the anastomosis of the graft to the duodenum by making an incision into the intestinal serous membrane, then burying the graft in the seromuscular layer to a depth of about 2 cm and making it open into the intestine. These methods conferred a verifiable anti-reflux function and provided quantitative evidence of inhibited bowel fluid reflux from the duodenum. Bilioenteric anastomosis is associated with a loss of duodenal papilla function and, consequently, with the risk of retrograde cholangitis. As technologies advance in the twenty-first century, we have better opportunities to improve this far-from-ideal anastomosis and to develop techniques that will lead to good long-term quality of life. We believe that our reflux-free anastomosis with the ABD is a promising operative procedure in the days ahead.
Grafting of an extrahepatic bile duct with a BAP tube
First, we succeeded in reproducing a bile duct which could serve as a bypass between the bile duct and the duodenum using a BAP [8]. Next, we demonstrated that if the bile duct has been damaged slightly, it can be restored and reproduced simply by suturing the BAP patch onto the damaged region even if the damage has resulted in a major procedure, such as the biliary–jejunal anastomosis [32]. In actual clinical practice, however, it is ideal to resect the bile duct having advanced fibril formation as in biliary stricture after laparoscopic cholecystectomy and then reproduce it in the shape of a loop between each of the bile ducts.
We are currently investigating whether this polymer is suited for such cases. Our initial results are favorable and have encouraged us to believe that this extrahepatic bile duct could be easily reproduced in the near future.
Development of a bioabsorbable biliary stent to induce favorable bile duct regeneration
Complications after biliary surgeries are currently managed by one of two non-surgical interventions, namely, balloon dilation or tube stent placement. Both are associated with high recurrence rates and less-than-adequate outcomes. The failures of these interventions can often be attributed to a poor understanding of either of two important points: the extent to which the stenosed portion should be dilated with a balloon [11], and how long the tube stent (TS) should be left in place [39, 40]. Crucially, no studies have been performed following such interventions to assess the histological changes of the biliary epithelium or the conditions that induce restenosis in the narrowed area.
Our group has developed a bioabsorbable biliary stent (BAS). This device has two important advantages: it can dilate the bile duct for longer than a balloon and to a larger diameter than a tube stent, and it can be left to degrade naturally in the body without subsequent endoscopic removal [41]. Our aims were to dilate the stenosed bile duct with this stent and induce “a process of favorable bile duct regeneration.” The results from our early attempts at this have been promising, and we are continuing forward in the same direction. In the past, reproduction of the bile duct epithelium was not taken into account during insertion of a biliary stent. However, the development of the bioabsorbable stent has progressed; this stent would be biodegradable in the body after completing its role of reproducing the epithelium at the site of the biliary anastomosis in a healthy condition, as is the case with our biliary stent [42].
Scaffolds to regenerate extrahepatic bile ducts by tissue engineering: literature review
Our group was the first to regenerate the bile duct by grafting a BAP patch to an injured or narrowed segment of the duct [9, 32, 38]. Various methods and materials have been devised to directly replace or reconstruct the narrowed duct. When the tract is reconstructed with non-absorbable vascular prosthetic materials, such as Gore-Tex [43–46], the strictures of the tract often recur early due to infection or late due to chronic foreign-body reactions. Our BAP patch disintegrates quickly: it clears from the body via the intestinal tract within 5 weeks, leaving no foreign matter behind. Meanwhile, the tissue regenerating outside the patch grows into a neo-bile duct similar to the native duct. Autologous grafts have also been proposed as prosthetic materials [47–50]. Yet the time required to collect and process them renders them unsuitable for emergency cases.
The BAP patch can be trimmed to any shape and size and may be useful in the repair of biliary tract injuries during surgery. Rosen et al. [11] have described a method of biliary tract regeneration using a porcine small intestinal submucosa (SIS), another prosthetic material that leaves no foreign matter in the body. However, SIS also has drawbacks, as it leaves the patient susceptible to zoonotic infection and is liable to induce cicatricial contractions [51, 52]. Because of its fibrous structure, the BAP patch is more resistant to rupture and easier to manipulate than other substitutive materials for bile duct reconstruction. And as an artificial material, it has no zoonotic potential [53, 54].
Conclusions
Our group has successfully applied tissue engineering techniques to extrahepatic bile duct regeneration. Encouraged by the results, we are now attempting to develop a reliable and clinically applicable method for inducing bile duct regeneration. The concept on which our method is based is still quite new and evidence of its feasibility may still be inadequate. Progress in the understanding of regeneration factors in bile will foster the development of therapeutic strategies aimed at the preservation of biological function and built on tissue engineering techniques.
References
Ammori BJ, Joseph S, Attia M, Lodge JP. Biliary strictures complicating pancreaticoduodenectomy. Int J Pancreatol. 2000;28:15.
Egawa H, Inomata Y, Uemoto S, Asonuma K, Kiuchi T, Fujita S, Hayashi M, Matamoros MA, Itou K, Tanaka K. Biliary anastomotic complications in 400 living related liver transplantations. World J Surg. 2001;25:1300.
Wojcicki M, Milkiewicz P, Silva M. Biliary tract complications after liver transplantation: a review. Dig Surg. 2008;25:245–57.
Maheshwari A, Maley W, Li Z, Thuluvath PJ. Biliary complications and outcomes of liver transplantation from donors after cardiac death. Liver Transpl. 2007;13:1645–53.
Nishida S, Nakamura N, Kadono J, Komokata T, Sakata R, Madariaga JR, Tzakis AG. Intrahepatic biliary strictures after liver transplantation. J Hepatobiliary Pancreat Surg. 2006;13:511–6.
Sugawara Y, Makuuchi M, Takayama T, Imamura H, Dowaki S, Mizuta K, Kawarasaki H, Hashizume K. Small-for-size grafts in living-related liver transplantation. J Am Coll Surg. 2001;192:510.
Halme L, Hockerstedt K, Lautenschlager I. Cytomegalovirus infection and development of biliary complications after liver transplantation. Transplantation. 2003;75:1853.
Miyazawa M, Torii T, Toshimitsu Y, Okada K, Koyama I, Ikada Y. A tissue-engineered artificial bile duct grown to resemble the native bile duct. Am J Transplant. 2005;5:1541–7.
Shimono K, Nose Y. The need to develop artificial bile ducts. Artif Organs. 1995;19:115.
Xu J, Sun S, Zhang Q, Chen J, Wu L, Liu W, Guo G. Experiment for a polyurethane replacement of the common bile duct. Chin Med J (Engl). 1998;111:86.
Rosen M, Ponsky J, Petras R, Fanning A, Brody F, Duperier F. Small intestinal submucosa as a bioscaffold for biliary tract regeneration. Surgery. 2002;132:480.
Teebken OE, Haverich A. Tissue engineering of small diameter vascular grafts. Eur J Vasc Endovasc Surg. 2002;23:475.
Shin’oka T, Imai Y, Ikada Y. Transplantation of a tissue-engineered pulmonary artery. N Engl J Med. 2001;344:532.
Kaihara S, Kim S, Benvenuto M, Kim BS, Mooney DJ, Tanaka K, Vacanti JP. End-to-end anastomosis between tissue-engineered intestine and native small bowel. Tissue Eng. 1999;5:339.
Perez A, Grikscheit TC, Blumberg RS, Ashley SW, Vacanti JP. Tissue-engineered small intestine: ontogeny of the immune system. Transplantation. 2002;74:619.
Ishizaki Y, Bandai Y, Shimomura K, Idezuki Y, Makuuchi M. Healing process of sutureless choledochojejunostomy in an experimental model. Br J Surg. 1995;82:1118–21.
Watanabe M, Shin’oka T, Tohyama S, Hibino N, Konuma T, Matsumura G, Kosaka Y, Ishida T, Imai Y, Yamakawa M, Ikada Y, Morita S. Tissue-engineered vascular autograft: inferior vena cava replacement in a dog model. Tissue Eng. 2001;7:429–39.
Noishiki Y, Tomizawa Y, Yamane Y, Matsumoto A. Autocrine angiogenic vascular prosthesis with bone marrow transplantation. Nat Med. 1996;2:90–3.
Bhattacharya V, McSweeney PA, Shi Q, Bruno B, Ishida A, Nash R, Storb RF, Sauvage LR, Hammond WP, Wu MH. Enhanced endothelialization and microvessel formation in polyester grafts seeded with CD34(+) bone marrow cells. Blood. 2000;95:581–5.
Dalakas E, Newsome PN, Boyle S, Brown R, Pryde A, McCall S, Hayes PC, Bickmore WA, Harrison DJ, Plevris JN. Bone marrow stem cells contribute to alcohol liver fibrosis in humans. Stem Cells Dev. 2010;19:1417–25.
Jang YY, Collector MI, Baylin SB, Diehl AM, Sharkis SJ. Hematopoietic stem cells convert into liver cells within days without fusion. Nat Cell Biol. 2004;6:532–9.
Oh SH, Witek RP, Bae SH, Zheng D, Jung Y, Piscaglia AC, Petersen BE. Bone marrow-derived hepatic oval cells differentiate into hepatocytes in 2-acetylaminofluorene/partial hepatectomy-induced liver regeneration. Gastroenterology. 2007;132:1077–87.
Tabibian JH, Asham EH, Han S, Saab S, Tong MJ, Goldstein L, Busuttil RW, Durazo FA. Endoscopic treatment of postorthotopic liver transplantation anastomotic biliary strictures with maximal stent therapy (with video). Gastrointest Endosc. 2010;71:505–12.
Pottakkat B, Vijayahari R, Prakash A, Singh RK, Behari A, Kumar A, Kapoor VK, Saxena R. Factors predicting failure following high bilio-enteric anastomosis for post-cholecystectomy benign biliary strictures. J Gastrointest Surg. 2010;14:1389–94.
Cantwell CP, Pena CS, Gervais DA, Hahn PF, Dawson SL, Mueller PR. Thirty years’ experience with balloon dilation of benign postoperative biliary strictures: long-term outcomes. Radiology. 2008;249:1050–7.
Sikora SS, Srikanth G, Agrawal V, Gupta RK, Kumar A, Saxena R, Kapoor VK. Liver histology in benign biliary stricture: fibrosis to cirrhosis… and reversal? J Gastroenterol Hepatol. 2008;23:1879–84.
Corvera CU, Blumgart LH, Darvishian F, Klimstra DS, DeMatteo R, Fong Y, D’Angelica M, Jarnagin WR. Clinical and pathologic features of proximal biliary strictures masquerading as hilar cholangiocarcinoma. J Am Coll Surg. 2005;201:862–9.
Lillemoe KD, Melton GB, Cameron JL, Pitt HA, Campbell KA, Talamini MA, Sauter PA, Coleman J, Yeo CJ. Postoperative bile duct strictures: management and outcome in the 1990 s. Ann Surg. 2000;232:430–41.
Shah SA, Grant DR, McGilvray ID, Greig PD, Selzner M, Lilly LB, Girgrah N, Levy GA, Cattral MS. Biliary strictures in 130 consecutive right lobe living donor liver transplant recipients: results of a Western center. Am J Transplant. 2007;7:161–7.
Judah JR, Draganov PV. Endoscopic therapy of benign biliary strictures. World J Gastroenterol. 2007;13:3531–9.
Lillemoe KD, Pitt HA, Cameron JL. Current management of benign bile duct strictures. Adv Surg. 1992;25:119–74.
Aikawa M, Miyazawa M, Okamoto K, Toshimitsu Y, Torii T, Okada K, Akimoto N, Ohtani Y, Koyama I, Yoshito I. A novel treatment for bile duct injury with a tissue-engineered bioabsorbable polymer patch. Surgery. 2010;147:575–80.
Tocchi A, Mazzoni G, Liotta G, Lepre L, Cassini D, Miccini M. Late development of bile duct cancer in patients who had biliary-enteric drainage for benign disease: a follow-up study of more than 1, 000 patients. Ann Surg. 2001;234:210–4.
Bettschart V, Clayton RA, Parks RW, Garden OJ, Bellamy CO. Cholangiocarcinoma arising after biliary-enteric drainage procedures for benign disease. Gut. 2002;51:128–9.
Herba MJ, Casola G, Bret PM, Lough J, Hampson LG. Cholangiocarcinoma as a late complication of choledochoenteric anastomoses. AJR Am J Roentgenol. 1986;147:513–5.
Gouma DJ, Konsten J, Soeters PB, Von Meyenfeldt M, Obertop H. Long-term follow-up after choledochojejunostomy for bile duct stones with complex clearance of the bile duct. Br J Surg. 1989;76:451–3.
Maeda A, Yokoi S, Kunou T, Saeki S, Niinomi N, Uesaka K. Bile duct cancer developing 21 years after choledochoduodenostomy. Dig Surg. 2003;20:331–4.
Aikawa M, Miyazawa M, Okada K, Toshimitsu Y, Okamoto K, Akimoto N, Koyama I, Ikada Y. Development of a novel reflux-free bilioenteric anastomosis procedure by using a bioabsorbable polymer tube. J Hepatobiliary Pancreat Sci. 2010;17:284–90.
Sakai Y, Tsuyuguchi T, Ishihara T, Yukisawa S, Sugiyama H, Miyakawa K, Kuroda Y, Yamaguchi T, Ozawa S, Yokosuka O. Long-term prognosis of patients with endoscopically treated postoperative bile duct stricture and bile duct stricture due to chronic pancreatitis. J Gastroenterol Hepatol. 2009;24:1191–7.
Roumilhac D, Poyet G, Sergent G, Declerck N, Karoui M, Mathurin P, Ernst O, Paris JC, Gambiez L, Pruvot FR. Long-term results of percutaneous management for anastomotic biliary stricture after orthotopic liver transplantation. Liver Transpl. 2003;9:394–400.
Miyazawa M, Aikawa M, Okada K, Torii T, Otani Y, Koyama I. Development of bioabsorbable biliary tract stens for treatment of benign biliary stenosis. Jpn J Gastroenterol Surg. 2007;40:1548.
Kasuya K, Shimazu M, Abe Y, Kikuchi S, Itoi T, Ikada Y, Aoki T, Tsuchida A. A newly developed degradable stent for pancreaticojejunostomy after pancreatoduodenectomy. Int Surg. 2010;95:247–56.
Bandura WP, Arbulu A. Experimental replacement of the common bile duct with teflon graft. Am Surg. 1961;27:518–24.
Gomez NA, Alvarez LR, Mite A, Andrade JP, Alvarez JR, Vargas PE, Tomala NE, Vivas AF, Zapatier JA. Repair of bile duct injuries with Gore-Tex vascular grafts: experimental study in dogs. J Gastrointest Surg. 2002;6:116–20.
Christensen M, Laursen HB, Rokkjaer M, Jensen PF, Yasuda Y, Mortensen FV. Reconstruction of the common bile duct by a vascular prosthetic graft: an experimental study in pigs. J Hepatobiliary Pancreat Surg. 2005;12:231–4.
Mendelowitz DS, Beal JM. Expanded polytetrafluoroethylene in reconstruction of the canine biliary system. Am J Surg. 1982;143:221–4.
Bottger T, Mann B, Pickel B, Weber W, Sorger K, Junginger T. Animal experiment studies of pedicled small intestine transplantation as partial extrahepatic bile duct replacement. Langenbecks Arch Chir. 1991;376:77–84.
Belzer FO, Watts JM, Ross HB, Dunphy JE. Auto-reconstruction of the common bile duct after venous patch graft. Ann Surg. 1965;162:346–55.
Aydin M, Bakir B, Kosem M, Kisli E, Genccelep M. Biliary tract reconstruction with autologous rectus sheath graft—an experimental study. Hepatogastroenterology. 2005;52:1019–22.
Sedgwick CE. Reconstruction of the common bile duct with a free ureteral graft; an experimental study. Surg Gynecol Obstet. 1951;92:571–3.
Gomez NA, Zapatier JA, Vargas PE. Re: “Small intestinal submucosa as a bioscaffold for biliary tract regeneration”. Surgery. 2004;135:460.
El-Assmy A, Hafez AT, El-Sherbiny MT, El-Hamid MA, Mohsen T, Nour EM, Bazeed M. Use of single layer small intestinal submucosa for long segment ureteral replacement: a pilot study. J Urol. 2004;171:1939–42.
Paradis K, Langford G, Long Z, Heneine W, Sandstrom P, Switzer WM, Chapman LE, Lockey C, Onions D, Otto E. Search for cross-species transmission of porcine endogenous retrovirus in patients treated with living pig tissue. The XEN 111 Study Group. Science. 1999;285:1236–41.
Fishman JA, Patience C. Xenotransplantation: infectious risk revisited. Am J Transplant. 2004;4:1383–90.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Miyazawa, M., Aikawa, M., Okada, K. et al. Regeneration of extrahepatic bile ducts by tissue engineering with a bioabsorbable polymer. J Artif Organs 15, 26–31 (2012). https://doi.org/10.1007/s10047-011-0590-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10047-011-0590-8